Clinical Focus ›› 2021, Vol. 36 ›› Issue (3): 270-276.doi: 10.3969/j.issn.1004-583X.2021.03.017
Previous Articles Next Articles
-
Received:2020-09-15Online:2021-03-20Published:2021-03-29
CLC Number:
Cite this article
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2021.03.017
| 神经源性 | 非神经源性 |
|---|---|
| 自主神经功能衰竭 脑干损伤/肿瘤 颈动脉窦过敏症 脑血管意外 多巴胺β-羟化酶缺乏症 多发性硬化 多系统萎缩 神经心源性晕厥 帕金森病 周围神经系统 HIV/AIDS,淀粉样变性,糖尿病,吉兰-巴雷综合征,肾衰竭,维生素 B12或叶酸缺乏症 脊髓(脊髓空洞症,脊髓痨,肿瘤,脊髓炎) 延髓空洞症 | 心血管疾病(主动脉狭窄,心力衰竭,心肌梗死,心肌炎,心包炎,快速性心律失常) 血容量下降 (出血,烧伤,脱水,尿崩症,腹泻,失盐肾病,呕吐) 静脉池(饮酒、发烧、发热、长时间卧床或站立、败血症) 药物 |
| 神经源性 | 非神经源性 |
|---|---|
| 自主神经功能衰竭 脑干损伤/肿瘤 颈动脉窦过敏症 脑血管意外 多巴胺β-羟化酶缺乏症 多发性硬化 多系统萎缩 神经心源性晕厥 帕金森病 周围神经系统 HIV/AIDS,淀粉样变性,糖尿病,吉兰-巴雷综合征,肾衰竭,维生素 B12或叶酸缺乏症 脊髓(脊髓空洞症,脊髓痨,肿瘤,脊髓炎) 延髓空洞症 | 心血管疾病(主动脉狭窄,心力衰竭,心肌梗死,心肌炎,心包炎,快速性心律失常) 血容量下降 (出血,烧伤,脱水,尿崩症,腹泻,失盐肾病,呕吐) 静脉池(饮酒、发烧、发热、长时间卧床或站立、败血症) 药物 |
| 药物种类 | 药物 |
|---|---|
| α-受体阻滞剂 降压药 | 特拉唑嗪,多沙唑嗪,哌唑嗪,坦索罗辛利尿药(噻嗪类和袢类),β-受体阻断剂,可乐定,长效钙通道阻断剂 |
| 抗精神病药 | 奥氮平,利培酮 |
| 单胺氧化酶抑制剂 | 雷沙吉兰,司来吉兰 |
| 麻醉剂 | 吗啡 |
| 帕金森病 | 溴隐亭,左旋多巴 |
| 三环类抗抑郁药 | 阿米替林,去甲替林 |
| 血管扩张剂 | 肼苯哒嗪,硝酸酯 |
| 药物种类 | 药物 |
|---|---|
| α-受体阻滞剂 降压药 | 特拉唑嗪,多沙唑嗪,哌唑嗪,坦索罗辛利尿药(噻嗪类和袢类),β-受体阻断剂,可乐定,长效钙通道阻断剂 |
| 抗精神病药 | 奥氮平,利培酮 |
| 单胺氧化酶抑制剂 | 雷沙吉兰,司来吉兰 |
| 麻醉剂 | 吗啡 |
| 帕金森病 | 溴隐亭,左旋多巴 |
| 三环类抗抑郁药 | 阿米替林,去甲替林 |
| 血管扩张剂 | 肼苯哒嗪,硝酸酯 |
| [1] |
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines[J]. J Am Coll Cardiol, 2018,71(19):e127-127e248.
doi: 10.1016/j.jacc.2017.11.006 URL |
| [2] |
Sheppard JP, Stevens S, Stevens R, et al. Benefits and harms of antihypertensive treatment in low-risk patients with mild hypertension[J]. JAMA Intern Med, 2018,178(12):1626-1634.
doi: 10.1001/jamainternmed.2018.4684 pmid: 30383082 |
| [3] |
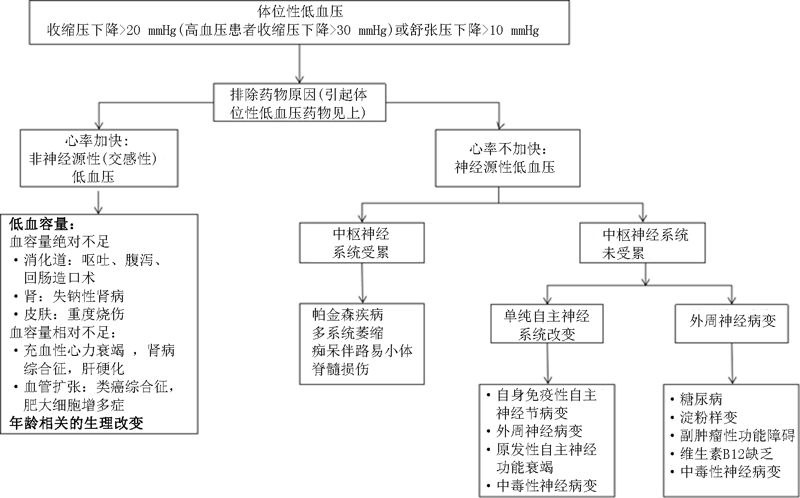
Joseph A, Wanono R, Flamant M, et al. Orthostatic hypotension: A review[J]. Nephrol Ther, 2017,13(Suppl 1):S55-55S67.
doi: 10.1016/j.nephro.2017.01.003 URL |
| [4] |
Chisholm P, Anpalahan M. Orthostatic hypotension: pathophysiology, assessment, treatment and the paradox of supine hypertension[J]. Intern Med J, 2017,47(4):370-379.
doi: 10.1111/imj.13171 pmid: 27389479 |
| [5] |
Lasserson DS, Buclin T, Glasziou P. How quickly should we titrate antihypertensive medication? Systematic review modelling blood pressure response from trial data[J]. Heart, 2011,97(21):1771-1775.
doi: 10.1136/hrt.2010.221473 pmid: 21586424 |
| [6] |
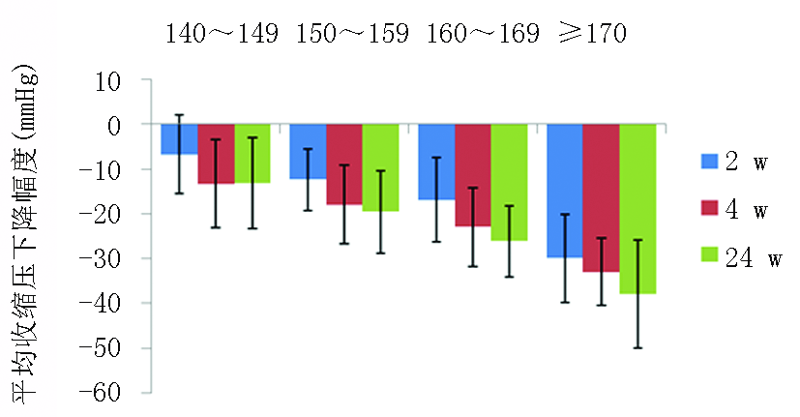
Kjeldsen SE, Cha G, Villa G, et al. Nifedipine GITS/Candesartan Combination Therapy Lowers Blood Pressure Across Different Baseline Systolic and Diastolic Blood Pressure Categories: DISTINCT Study Subanalyses[J]. J Clin Pharmacol, 2016,56(9):1120-1129.
doi: 10.1002/jcph.v56.9 URL |
| [7] | 中国高血压防治指南修订委员会, 高血压联盟(中国), 中华医学会心血管病学分会, 等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019,24(1):24-56. |
| [8] |
Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines[J]. J Hypertens, 2020,38(6):982-1004.
doi: 10.1097/HJH.0000000000002453 URL |
| [9] |
Hu H, Zhang J, Wang Y, et al. Impact of baseline blood pressure on the magnitude of blood pressure lowering by nifedipine gastrointestinal therapeutic system: refreshing the Wilder's principle[J]. Drug Des Devel Ther, 2017,11:3179-3186.
doi: 10.2147/DDDT URL |
| [10] |
Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension[J]. J Chin Med Assoc, 2015,78(1):1-47.
doi: 10.1016/j.jcma.2014.11.005 URL |
| [11] |
Mourad JJ, Amodeo C, de Champvallins M, et al. Blood pressure-lowering efficacy and safety of perindopril/indapamide/amlodipine single-pill combination in patients with uncontrolled essential hypertension: a multicenter, randomized, double-blind, controlled trial[J]. J Hypertens, 2017,35(7):1481-1495.
doi: 10.1097/HJH.0000000000001359 URL |
| [12] |
Motaweih AK, Usova E, Hussain W, et al. Effectiveness of combination therapy with nifedipine GITS: a prospective, 12-week observational study (AdADOSE)[J]. BMC Cardiovasc Disord, 2015,15:35.
doi: 10.1186/s12872-015-0037-x URL |
| [13] |
Hoshide S, Kario K, Tomitani N, et al. Highlights of the 2019 Japanese Society of Hypertension Guidelines and perspectives on the management of Asian hypertensive patients[J]. J Clin Hypertens (Greenwich), 2020,22(3):369-377.
doi: 10.1111/jch.v22.3 URL |
| [14] |
SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control[J]. N Engl J Med, 2015,373(22):2103-2116.
doi: 10.1056/NEJMoa1511939 URL |
| [15] |
Rueda-Ochoa OL, Rojas LZ, Ahmad S, et al. Impact of cumulative SBP and serious adverse events on efficacy of intensive blood pressure treatment: a randomized clinical trial[J]. J Hypertens, 2019,37(5):1058-1069.
doi: 10.1097/HJH.0000000000002001 pmid: WOS:000473104200023 |
| [16] |
Peters R, Anstey KJ, Booth A, et al. Orthostatic hypotension and symptomatic subclinical orthostatic hypotension increase risk of cognitive impairment: an integrated evidence review and analysis of a large older adult hypertensive cohort[J]. Eur Heart J, 2018,39(33):3135-3143.
doi: 10.1093/eurheartj/ehy418 URL |
| [17] |
Foster-Dingley JC, Moonen J, de Ruijter W, et al. Orthostatic hypotension in older persons is not associated with cognitive functioning, features of cerebral damage or cerebral blood flow[J]. J Hypertens, 2018,36(5):1201-1206.
doi: 10.1097/HJH.0000000000001681 URL |
| [18] |
Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome[J]. Clin Auton Res, 2011,21(2):69-72.
doi: 10.1007/s10286-011-0119-5 URL |
| [19] |
Juraschek SP, Daya N, Appel LJ, et al. Orthostatic hypotension in middle-age and risk of falls[J]. Am J Hypertens, 2017,30(2):188-195.
doi: 10.1093/ajh/hpw108 URL |
| [20] |
Mol A, Bui Hoang P, Sharmin S, et al. Orthostatic hypotension and falls in older adults: a systematic review and meta-analysis[J]. J Am Med Dir Assoc, 2019, 20(5):589-597.e5.
doi: 10.1016/j.jamda.2018.11.003 URL |
| [21] |
Momeyer MA, Mion LC. Orthostatic hypotension: an often overlooked risk factor for falls[J]. Geriatr Nurs, 2018,39(4):483-486.
doi: S0197-4572(18)30320-3 pmid: 30017455 |
| [22] |
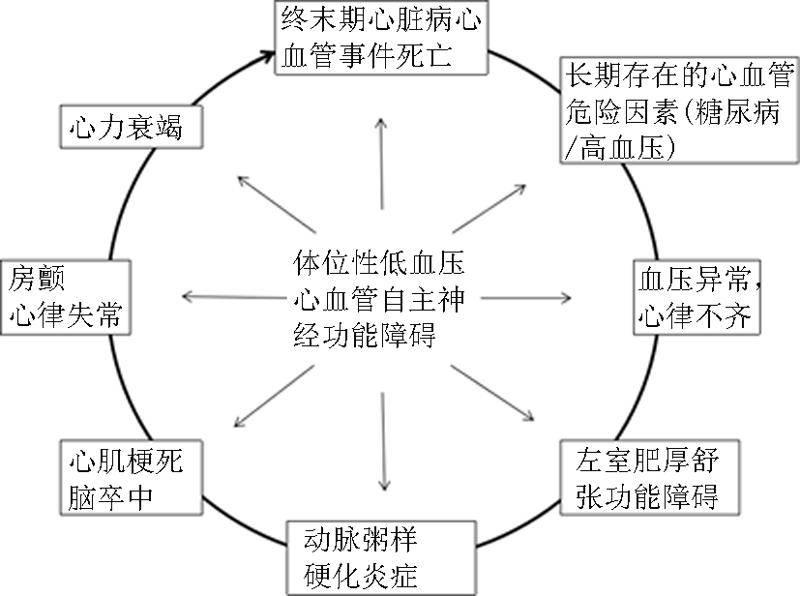
Fedorowski A, Wahlstrand B, Hedner T, et al. Systolic and diastolic component of orthostatic hypotension and cardiovascular events in hypertensive patients: the Captopril Prevention Project[J]. J Hypertens, 2014,32(1):75-81.
doi: 10.1097/HJH.0b013e328365cd59 URL |
| [23] |
Rose KM, Tyroler HA, Nardo CJ, et al. Orthostatic hypotension and the incidence of coronary heart disease: the Atherosclerosis Risk in Communities study[J]. Am J Hypertens, 2000,13(6 Pt 1):571-578.
pmid: 10912737 |
| [24] |
Mancia G, Grassi G. Orthostatic hypotension and cardiovascular risk: defining the epidemiological and prognostic relevance[J]. Eur Heart J, 2010,31(1):12-14.
doi: 10.1093/eurheartj/ehp389 URL |
| [25] |
Juraschek SP, Lipsitz LA, Beach JL, et al. Association of orthostatic hypotension timing with clinical events in adults with diabetes and hypertension: Results From the ACCORD trial[J]. Am J Hypertens, 2019,32(7):684-694.
doi: 10.1093/ajh/hpz015 pmid: WOS:000489127400012 |
| [26] |
Hiorth YH, Pedersen KF, Dalen I, et al. Orthostatic hypotension in Parkinson disease: A 7-year prospective population-based study[J]. Neurology, 2019,93(16):e1526-1526e1534.
doi: 10.1212/WNL.0000000000008314 URL |
| [27] |
Fedorowski A, Ricci F, Sutton R. Orthostatic hypotension and cardiovascular risk[J]. Kardiol Pol, 2019,77(11):1020-1027.
doi: 10.33963/KP.15055 pmid: 31713533 |
| [28] |
Xin W, Mi S, Lin Z, et al. Orthostatic hypotension and the risk of incidental cardiovascular diseases: A meta-analysis of prospective cohort studies[J]. Prev Med, 2016,85:90-97.
doi: 10.1016/j.ypmed.2016.01.007 URL |
| [29] | 中国老年医学学会高血压分会, 国家老年疾病临床医学研究中心中国老年心血管病防治联盟. 中国老年高血压管理指南2019[J]. 中国心血管杂志, 2019,24(1):1-23. |
| [30] |
Task Force for the Diagnosis and Management of Syncope, European Society of Cardiology (ESC), European Heart Rhythm Association (EHRA), et al. Guidelines for the diagnosis and management of syncope (version 2009)[J]. Eur Heart J, 2009,30(21):2631-2671.
doi: 10.1093/eurheartj/ehp298 URL |
| [31] |
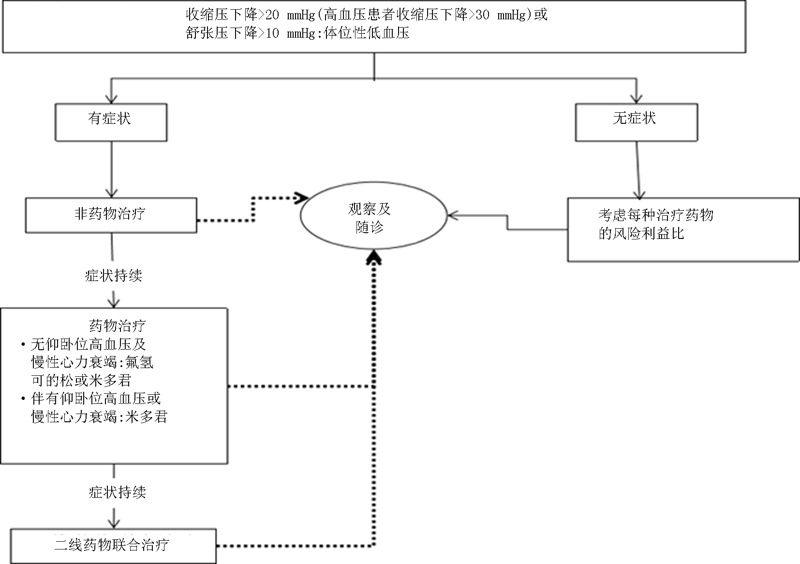
Ricci F, De Caterina R, Fedorowski A. Orthostatic hypotension: Epidemiology, prognosis, and treatment[J]. J Am Coll Cardiol, 2015,66(7):848-860.
doi: 10.1016/j.jacc.2015.06.1084 URL |
| [32] |
Hale GM, Valdes J, Brenner M. The treatment of primary orthostatic hypotension[J]. Ann Pharmacother, 2017,51(5):417-428.
doi: 10.1177/1060028016689264 URL |
| [33] |
Victor RG. Carotid baroreflex activation therapy for resistant hypertension[J]. Nat Rev Cardiol, 2015,12(8):451-463.
doi: 10.1038/nrcardio.2015.96 URL |
| [34] |
Freeman R, Abuzinadah AR, Gibbons C, et al. Orthostatic Hypotension: JACC State-of-the-Art Review[J]. J Am Coll Cardiol, 2018,72(11):1294-1309.
doi: 10.1016/j.jacc.2018.05.079 URL |
| [35] |
Lahrmann H, Cortelli P, Hilz M, et al. EFNS guidelines on the diagnosis and management of orthostatic hypotension[J]. Eur J Neurol, 2006,13(9):930-936.
doi: 10.1111/ene.2006.13.issue-9 URL |
| [36] |
Cheshire WP. Chemical pharmacotherapy for the treatment of orthostatic hypotension[J]. Expert Opin Pharmacother, 2019,20(2):187-199.
doi: 10.1080/14656566.2018.1543404 pmid: 30376728 |
| [37] |
Biaggioni I. Orthostatic hypotension in the hypertensive patient[J]. Am J Hypertens, 2018,31(12):1255-1259.
doi: 10.1093/ajh/hpy089 URL |
| [38] |
Shibao C, Lipsitz LA, Biaggioni I. ASH position paper: evaluation and treatment of orthostatic hypotension[J]. J Clin Hypertens (Greenwich), 2013,15(3):147-153.
doi: 10.1111/jch.12062 URL |
| [39] |
Benditt DG, Adkisson WO. Approach to the patient with syncope: venues, presentations, diagnoses[J]. Cardiol Clin, 2013,31(1):9-25.
doi: 10.1016/j.ccl.2012.09.002 pmid: 23217684 |
| [40] |
Mar PL, Raj SR. Orthostatic hypotension for the cardiologist[J]. Curr Opin Cardiol, 2018,33(1):66-72.
doi: 10.1097/HCO.0000000000000467 URL |
| [41] |
McDonell KE, Shibao CA, Biaggioni I, et al. Cognitive and behavioral changes in patients treated with droxidopa for neurogenic orthostatic hypotension: A retrospective review[J]. Cogn Behav Neurol, 2019,32(3):179-184.
doi: 10.1097/WNN.0000000000000198 URL |
| [42] |
Pérez-Lloret S, Quarracino C, Otero-Losada M, et al. Droxidopa for the treatment of neurogenic orthostatic hypotension in neurodegenerative diseases[J]. Expert Opin Pharmacother, 2019,20(6):635-645.
doi: 10.1080/14656566.2019.1574746 pmid: 30730771 |
| [43] |
Byun JI, Moon J, Kim DY, et al. Delayed orthostatic hypotension: Severity of clinical symptoms and response to medical treatment[J]. Auton Neurosci, 2018,213:81-85.
doi: 10.1016/j.autneu.2018.06.005 URL |
| [44] |
Chen JJ, Han Y, Tang J, et al. Standing and supine blood pressure outcomes associated with droxidopa and midodrine in patients with neurogenic orthostatic hypotension: A bayesian meta-analysis and mixed treatment comparison of randomized trials[J]. Ann Pharmacother, 2018,52(12):1182-1194.
doi: 10.1177/1060028018786954 URL |
| [45] |
Olshansky B, Muldowney J. Cardiovascular safety considerations in the treatment of neurogenic orthostatic hypotension[J]. Am J Cardiol, 2020,125(10):1582-1593.
doi: 10.1016/j.amjcard.2020.01.037 URL |
| [46] |
Baker J, Kimpinski K. Management of supine hypertension complicating neurogenic orthostatic hypotension[J]. CNS Drugs, 2017,31(8):653-663.
doi: 10.1007/s40263-017-0453-9 URL |
| [47] |
Vallelonga F, Maule S. Diagnostic and therapeutical management of supine hypertension in autonomic failure: a review of the literature[J]. J Hypertens, 2019,37(6):1102-1111.
doi: 10.1097/HJH.0000000000002008 pmid: WOS:000480759900002 |
| [48] |
Jordan J, Fanciulli A, Tank J, et al. Management of supine hypertension in patients with neurogenic orthostatic hypotension: scientific statement of the American Autonomic Society, European Federation of Autonomic Societies, and the European Society of Hypertension[J]. J Hypertens, 2019,37(8):1541-1546.
doi: 10.1097/HJH.0000000000002078 pmid: WOS:000480767600001 |
| [49] |
Schoevaerdts D, Iacovelli M, Toussaint E, et al. Prevalence and risk factors of postprandial hypotension among elderly people admitted in a geriatric evaluation and management unit: An observational study[J]. J Nutr Health Aging, 2019,23(10):1026-1033.
doi: 10.1007/s12603-019-1271-1 pmid: 31781734 |
| [50] | Madden KM, Feldman B, Meneilly GS. Baroreflex function and postprandial hypotension in older adults[J]. Clin Auton Res, 2020. |
| [51] |
Jang A. Postprandial hypotension as a risk factor for the development of new cardiovascular disease: A prospective cohort study with 36 month follow-up in community-dwelling elderly people[J]. J Clin Med, 2020,9(2):345.
doi: 10.3390/jcm9020345 URL |
| [52] |
Trahair LG, Rajendran S, Visvanathan R, et al. Comparative effects of glucose and water drinks on blood pressure and cardiac function in older subjects with and without postprandial hypotension[J]. Physiol Rep, 2017,5(13):e13341.
doi: 10.14814/phy2.13341 URL |
| [53] |
Nair S, Visvanathan R, Gentilcore D. Intermittent walking: a potential treatment for older people with postprandial hypotension[J]. J Am Med Dir Assoc, 2015,16(2):160-164.
doi: 10.1016/j.jamda.2014.08.013 URL |
| [54] | 张亚楠, 陈天磊, 耿雪, 等. 住院高血压合并冠心病患者餐后低血压的临床观察[J]. 中华医学杂志, 2018,98(33):2641-2644. |
| [55] |
Qiao W, Li J, Li Y, et al. Acarbose, the α-glucosidase inhibitor, attenuates the blood pressure and splanchnic blood flow responses to meal in elderly patients with postprandial hypotension concomitant with abnormal glucose metabolism[J]. Blood Press Monit, 2016,21(1):38-42.
doi: 10.1097/MBP.0000000000000160 pmid: 26474001 |
| [56] |
Bhattarai M, Sainju NK, Bhandari B, et al. Prevalence of white coat hypertension among the patients visiting in a tertiary care center, Kathmandu, Nepal[J]. Kathmandu Univ Med J (KUMJ), 2019,17(66):119-122.
pmid: 32632058 |
| [57] |
Dele-Ojo B, Kolo P, Ogunmodede A, et al. Prevalence and predictors of white coat hypertension among newly-diagnosed hypertensive patients in a tertiary health centre in nigeria[J]. Ethiop J Health Sci, 2019,29(4):431-438.
doi: 10.4314/ejhs.v29i4.3 pmid: 31447515 |
| [58] |
Varlamova NG, Zenchenko TA, Boyko ER. Annual blood pressure dynamics and weather sensitivity in women[J]. Ter Arkh, 2017,89(12):56-63.
doi: 10.17116/terarkh201789656-61 URL |
| [59] | Ushigome E, Kitagawa N, Kitae A, et al. Seasonal variation in home blood pressure and its relationship with room temperature in patients with type 2 diabetes[J]. Diab Vasc Dis Res, 2020,17(1):1479164119883986. |
| [1] | ZHAO Ping;CHANG Pei-ye;LIU Zhi-yue;CHEN Yao. Association between rs1558139 of human CYP4F2 gene and essential hypertension in Mongolian ethnic [J]. Clinical Focus, 2012, 27(14): 1211-1.21312e+007. |
| [2] | LIN Tao;ZHANG Yu-qing;XU Chong-li. Effects of atorvastatin on heart rate variability in hypertensive patients with hyperlipidemia [J]. Clinical Focus, 2011, 26(15): 1305-1307. |
| [3] | . [J]. CLINICAL FOCUS, 2011, 26(5): 427-428. |
| [4] | HOU Cong-cong;LI Yong-jun;ZHANG Hui;YANG Rong;WANG Mei;WANG Ya-ling. Load amount of trimetazidine's influence on endothelial function in patients with coronary heart disease and hypertension [J]. CLINICAL FOCUS, 2011, 26(2): 110-112116. |
| [5] | YUAN Ai-zhong;YAO Xiao-jun;CHENG Chuan-bin;WANG Ji-wei;LIU Hong-sheng;SUN Cheng-du;LIU Jia-bing. Clinical study of minimally invasive surgery combined with method of activating blood circulation to dissipating blood stasis in treatment of hypertensive intracerebral hemorrhage [J]. CLINICAL FOCUS, 2010, 25(16): 1390-1392. |
| [6] | . [J]. CLINICAL FOCUS, 2010, 25(15): 1353-1355. |
| [7] | . [J]. CLINICAL FOCUS, 2007, 22(23): 1702-1703. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||