Clinical Focus ›› 2022, Vol. 37 ›› Issue (5): 472-476.doi: 10.3969/j.issn.1004-583X.2022.05.017
Previous Articles Next Articles
-
Received:2022-02-08Online:2022-05-20Published:2022-06-22
CLC Number:
Cite this article
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2022.05.017
| [1] |
Sieper J, Poddubnyy D. Axial spondyloarthritis[J]. Lancet, 2017, 390(10089):73-84.
doi: 10.1016/S0140-6736(16)31591-4 URL |
| [2] | Wenker KJ, Quint JM. Ankylosing spondylitis[M]. In: Statpearls. Treasure Island (fl): Statpearls Publishing llc, 2022. |
| [3] |
Korotaeva T, Dina o, Holdsworth E, et al. Investigating diagnosis, treatment, and burden of disease in patients with ankylosing spondylitis in central eastern europe and the United States: A real-world study[J]. Clin Rheumatol, 2021, 40(12):4915-4926.
doi: 10.1007/s10067-021-05864-8 pmid: 34319479 |
| [4] |
Golder V, Schachna L. Ankylosing spondylitis: An update[J]. Aust Fam Physician, 2013, 42(11):780-784.
pmid: 24217097 |
| [5] |
de Bruin F, Treyvaud MO, Feydy A, et al. Prevalence of degenerative changes and overlap with spondyloarthritis-associated lesions in the spine of patients from the desir cohort[J]. Rmd Open 2018, 4(1):e000657.
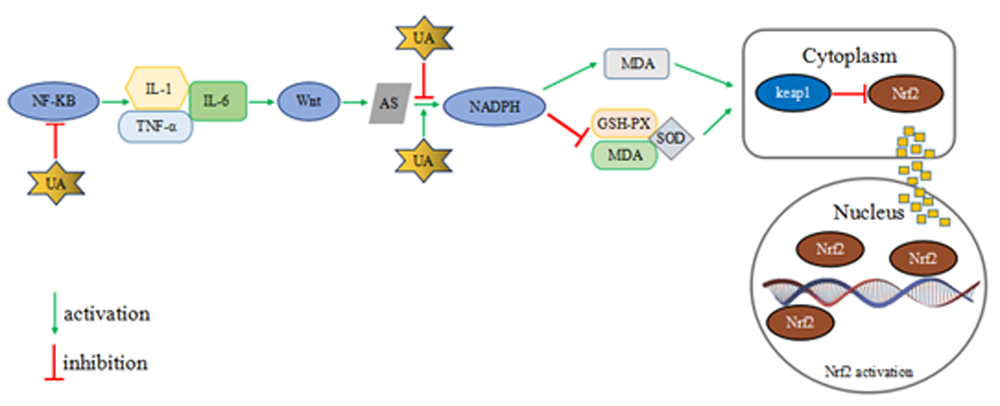
doi: 10.1136/rmdopen-2018-000657 URL |
| [6] |
van der Heijde D, Braun J, Deodhar A, et al. Modified stoke ankylosing spondylitis spinal score as an outcome measure to assess the impact of treatment on structural progression in ankylosing spondylitis[J]. Rheumatology (Oxford), 2019, 58(3):388-400.
doi: 10.1093/rheumatology/key128 URL |
| [7] |
Magrey M, Ritchlin C. Measuring outcomes in ankylosing spondylitis: Pearls and pitfalls[J]. Curr Opin Rheumatol, 2019, 31(2):109-117.
doi: 10.1097/BOR.0000000000000588 URL |
| [8] |
Liu L, Yuan Y, Zhang S, et al. Osteoimmunological insights into the pathogenesis of ankylosing spondylitis[J]. J Cell Physiol, 2021, 236(9):6090-6100.
doi: 10.1002/jcp.30313 URL |
| [9] |
Song C, Zhao X. Uric acid promotes oxidative stress and enhances vascular endothelial cell apoptosis in rats with middle cerebral artery occlusion[J]. Biosci Rep, 2018, 38(3):bsr20170939.
doi: 10.1042/BSR20170939 URL |
| [10] | Suzuki T, Yamamoto M. Molecular basis of the keap1-Nrf2 system[J]. Free Radic Biol Med, 2015, 88(Pt B):93-100. |
| [11] | Zou YC, Yang XW, Yuan SG, et al. Celastrol inhibits prostaglandin e2-induced proliferation and osteogenic differentiation of fibroblasts isolated from ankylosing spondylitis hip tissues in vitro[J]. Drug Des Devel Ther, 2016, 10:933-948. |
| [12] |
Zhu J, Li A, Jia E, et al. Monosodium urate crystal deposition associated with the progress of radiographic grade at the sacroiliac joint in axial spa: A dual-energy CT study[J]. Arthritis Res Ther, 2017, 19(1):83.
doi: 10.1186/s13075-017-1286-0 URL |
| [13] | Zhang XJ, Cui XM, Chen RY, et al. The analysis of clinical characteristics and disease activity in ankylosing spondylitis patients with hyperuricemia[J]. Zhonghua Yi Xue Za Zhi, 2018, 98(13):982-986. |
| [14] | 曾沛英, 钟剑球, 黄雪婷, 等. 合并高尿酸血症的强直性脊柱炎患者的临床分析[J]. 中华风湿病学杂志, 2019, 23(7):454-458. |
| [15] |
Ye G, Xie Z, Zeng H, et al. Oxidative stress-mediated mitochondrial dysfunction facilitates mesenchymal stem cell senescence in ankylosing spondylitis[J]. Cell Death Dis, 2020, 11(9):775.
doi: 10.1038/s41419-020-02993-x URL |
| [16] | Dong M, Yu D, Duraipandiyan V, et al. The protective effect of chrysanthemum indicum extract against ankylosing spondylitis in mouse models[J]. Biomed Res Int, 2017:8206281. |
| [17] |
Müller SG, Jardim NS, Quines CB, et al. Diphenyl diselenide regulates nrf2/keap-1 signaling pathway and counteracts hepatic oxidative stress induced by bisphenol a in male mice[J]. Environ Res, 2018, 164:280-287.
doi: 10.1016/j.envres.2018.03.006 URL |
| [18] |
Vnukovb VV, Gutsenko OI, Milyutina NP, et al. Skq1 regulates expression of nrf2, are-controlled genes encoding antioxidant enzymes, and their activity in cerebral cortex under oxidative stress[J]. Biochemistry (Mosc), 2017, 82(8):942-952.
doi: 10.1134/S0006297917080090 URL |
| [19] |
Zhang N, Shu HY, Huang T, et al. Nrf2 signaling contributes to the neuroprotective effects of urate against 6-ohda toxicity[J]. PLoS One, 2014, 9(6):e100286.
doi: 10.1371/journal.pone.0100286 URL |
| [20] | Ya BL, Liu Q, Li HF, et al. Uric acid protects against focal cerebral ischemia/reperfusion-induced oxidative stress via activating nrf2 and regulating neurotrophic factor expression[J]. Oxid Med Cell Longev, 2018:6069150. |
| [21] | 沈瑞明, 李国铨, 郭峰. 血尿酸通过keap1-nrf2信号通路对强直性脊柱炎氧化应激作用机制研究[J]. 海南医学院学报, 2020, 26(10):771-774, 781. |
| [22] | Singh HJ, Nimarpreet K, Ashima, et al. Study of bone mineral density in patients with ankylosing spondylitis[J]. J Clin Diagn Res, 2013, 7(12):2832-2835. |
| [23] | Wang C, Li W. Effects of etanercept and infliximab on bone metabolism indexes in patients with ankylosing spondylitis[J]. Exp Ther Med, 2020, 19(1):585-590. |
| [24] |
Rozenberg K, Wollman A, Ben-Shachar M, et al. Anti-inflammatory effects of sarcopoterium spinosum extract[J]. J Ethnopharmacol, 2020, 249:112391.
doi: 10.1016/j.jep.2019.112391 URL |
| [25] |
Redlich K, Smolen JS. Inflammatory bone loss: Pathogenesis and therapeutic intervention[J]. Nat Rev Drug Discov, 2012, 11(3):234-250.
doi: 10.1038/nrd3669 pmid: 22378270 |
| [26] |
Cheng GM, Wang RL, Zhang B, et al. The protective effect of uric acid in reducing tlr4/nf-κb activation through the inhibition of hmgb1 acetylation in a model of ischemia-reperfusion injury in vitro[J]. Mol Biol Rep, 2020, 47(4):3233-3240.
doi: 10.1007/s11033-020-05324-7 URL |
| [27] |
Ishii S, Miyao M, Mizuno Y, et al. Association between serum uric acid and lumbar spine bone mineral density in peri- and postmenopausal Japanese women[J]. Osteoporos Int, 2014, 25(3):1099-1105.
doi: 10.1007/s00198-013-2571-7 pmid: 24318630 |
| [28] |
Kanzaki H, Shinohara F, Kajiya M, et al. The Keap1/Nrf2 protein axis plays a role in osteoclast differentiation by regulating intracellular reactive oxygen species signaling[J]. J Biol Chem, 2013, 288(32):23009-23020.
doi: 10.1074/jbc.M113.478545 URL |
| [29] |
Yin Y, Corry KA, Loughran JP, et al. Moderate Nrf2 activation by genetic disruption of keap1 has sex-specific effects on bone mass in mice[J]. Sci Rep, 2020, 10(1):348.
doi: 10.1038/s41598-019-57185-1 URL |
| [30] |
Bonaccorsi G, Trentini A, Greco P, et al. Changes in adipose tissue distribution and association between uric acid and bone health during menopause transition[J]. Int J Mol Sci, 2019, 20(24):6321.
doi: 10.3390/ijms20246321 URL |
| [31] |
Ibrahim WN, Younes N, Shi Z, et al. Serum uric acid level is positively associated with higher bone mineral density at multiple skeletal sites among healthy qataris[J]. Front Endocrinol (Lausanne), 2021, 12:653685.
doi: 10.3389/fendo.2021.653685 URL |
| [32] |
Yan DD, Wang J, Hou XH, et al. Association of serum uric acid levels with osteoporosis and bone turnover markers in a chinese population[J]. Acta Pharmacol Sin, 2018, 39(4):626-632.
doi: 10.1038/aps.2017.165 URL |
| [33] |
Wu Y, Zhang G, Wang N, et al. Risk factors of renal involvement based on different manifestations in patients with ankylosing spondylitis[J]. Kidney Blood Press Res, 2018, 43(2):367-377.
doi: 10.1159/000488071 URL |
| [34] |
Rauner M, Thiele S, Fert I, et al. Loss of bone strength in hla-b27 transgenic rats is characterized by a high bone turnover and is mainly osteoclast-driven[J]. Bone, 2015, 75:183-191.
doi: 10.1016/j.bone.2015.02.024 URL |
| [35] | Zhang T, Yang F, Zuo K, et al. HLA-B27 negativity is associated with renal function decline in patients with ankylosing spondylitis and secondary iga nephropathy[J]. Front Med (Lausanne), 2020, 7:89. |
| [36] |
Coppolino G, Leonardi G, Andreucci M, et al. oxidative stress and kidney function:A brief update[J]. Curr Pharm Des, 2018, 24(40):4794-4799.
doi: 10.2174/1381612825666190112165206 URL |
| [37] |
Tonelli C, Chio IIC, Tuveson DA. Transcriptional regulation by Nrf2[J]. Antioxid Redox Signal, 2018, 29(17):1727-1745.
doi: 10.1089/ars.2017.7342 URL |
| [38] |
Saito H. Toxico-pharmacological perspective of the Nrf2-Keap1 defense system against oxidative stress in kidney diseases[J]. Biochem Pharmacol, 2013, 85(7):865-872.
doi: 10.1016/j.bcp.2013.01.006 URL |
| [39] |
Nezu M, Suzuki N, Yamamoto M. Targeting the Keap1-Nrf2 system to prevent kidney disease progression[J]. Am J Nephrol, 2017, 45(6):473-483.
doi: 10.1159/000475890 URL |
| [40] | Lin Y, Xie Y, Hao Z, et al. Protective effect of uric acid on ox-ldl-induced huvecs injury via Keap1-Nrf2-are pathway[J]. J Immunol Res, 2021:5151168. |
| [41] |
Li B, Jiang T, Liu H, et al. Andrographolide protects chondrocytes from oxidative stress injury by activation of the Keap1-Nrf2-are signaling pathway[J]. J Cell Physiol, 2018, 234(1):561-571.
doi: 10.1002/jcp.26769 URL |
| [42] | He X, Liang B, Gu N. Th17/Treg imbalance and atherosclerosis[J]. Dis Markers, 2020: 8821029. |
| [43] | Tudoraᶊcu DR, Ciurea PL, Vreju AF, et al. Assessing endothelial dysfunction in patients with ankylosing spondylitis[J]. Curr Health Sci J, 2016, 42(1):61-68. |
| [44] | van-Assche T, Huygelen V, Crabtree MJ, et al. Gene therapy targeting inflammation in atherosclerosis[J]. Curr Health Sci J, 2011, 17(37):4210-4223. |
| [45] |
Zhu H, Jia Z, Zhang L, et al. Antioxidants and phase 2 enzymes in macrophages: Regulation by Nrf2 signaling and protection against oxidative and electrophilic stress[J]. Exp Biol Med (Maywood), 2008, 233(4): 463-474.
doi: 10.3181/0711-RM-304 URL |
| [46] |
Chen B, Lu Y, Chen Y, et al. The role of Nrf2 in oxidative stress-induced endothelial injuries[J]. J Endocrinol, 2015, 225(3):r83-99.
doi: 10.1530/JOE-14-0662 URL |
| [47] |
Ko J, Kang HJ, Kim DA, et al. Uric acid induced the phenotype transition of vascular endothelial cells via induction of oxidative stress and glycocalyx shedding[J]. FASEB J, 2019, 33(12):13334-13345.
doi: 10.1096/fj.201901148R URL |
| [48] |
Kurajoh M, Fukumoto S, Yoshida S, et al. Uric acid shown to contribute to increased oxidative stress level independent of xanthine oxidoreductase activity in medcity21 health examination registry[J]. Sci Rep, 2021, 11(1):7378.
doi: 10.1038/s41598-021-86962-0 URL |
| [49] |
Dalbeth N, House ME, Aati O, et al. Urate crystal deposition in asymptomatic hyperuricaemia and symptomatic gout: A dual energy CT study[J]. Ann Rheum Dis, 2015, 74(5):908-911.
doi: 10.1136/annrheumdis-2014-206397 pmid: 25637002 |
| [50] |
Andrés M, Quintanilla MA, Sivera F, et al. Silent monosodium urate crystal deposits are associated with severe coronary calcification in asymptomatic hyperuricemia: An exploratory study[J]. Arthritis Rheumatol, 2016, 68(6):1531-1539.
doi: 10.1002/art.39581 URL |
| [51] |
Kang KY, Hong YS, Park SH, et al. Low levels of serum uric acid increase the risk of low bone mineral density in young male patients with ankylosing spondylitis[J]. J Rheumatol, 2015, 42(6):968-974.
doi: 10.3899/jrheum.140850 URL |
| [52] | 孙文婷, 朱峰, 郑丹妮, 等. 男性强直性脊柱炎患者骨密度与血尿酸水平相关性研究[J]. 中国骨质疏松杂志, 2020, 26(4):502-506. |
| [53] |
Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of ageing[J]. Nature, 2000, 408(6809):239-247.
doi: 10.1038/35041687 URL |
| [54] | 黎荣山, 黎文军, 王勇, 等. 柳州市人群血尿酸水平与骨密度之间的关系[J]. 中国医学创新 2016, 13(15):138-141. |
| [55] |
Chen Z, Yang P, Wu Y, et al. Serum uric acid shows inverted “u” type correlation with osteoporosis in chinese ankylosing spondylitis patients: A retrospective study[J]. Med Sci Monit, 2019, 25:9702-9711.
doi: 10.12659/MSM.918766 URL |
| [56] |
Zhang B, Yang N, Lin SP, et al. Suitable concentrations of uric acid can reduce cell death in models of OGD and cerebral ischemia-reperfusion injury[J]. Cell Mol Neurobiol, 2017, 37(5):931-939.
doi: 10.1007/s10571-016-0430-8 pmid: 27709309 |
| [1] | Gao Ying, Han Zhongli, Wang Hongyan, Li Xiaofu. Magnetic resonance imaging characteristics of Andersson lesions associated with ankylosing spondylitis [J]. Clinical Focus, 2022, 37(10): 927-930. |
| [2] | Li Huiting, Meng Jinghong, Gu Guang, Chen Haiying, Wang Junxiang. Clinical characteristics of ankylosing spondylitis with hip involvement [J]. Clinical Focus, 2021, 36(6): 500-503. |
| [3] | Yan Shu;Lu Yahua. Clinical features of pulmonary damage in ankylosing spondylitis patients and related factors [J]. Clinical Focus, 2015, 30(8): 879-882887. |
| [4] | Wen Haifeng;Feng Zhongjun;Han Wenlong;Qin Jin;Yu Wenjing. Establishment and evaluation of real-time fluorescence PCR with DNA melting curve for detection of HLA-B27 [J]. Clinical Focus, 2015, 30(6): 674-676677. |
| [5] | Xie Jianli;Wei Ping;Wang Junxiang;Zhang Zhipeng. Effect of active vitamin D combined with 99 Tc-MDP on bone metabolism of ankylosing spondylitis patients [J]. Clinical Focus, 2015, 30(1): 22-2425. |
| [6] | ZHANG Lu;YU Wu-zhong;ZHANG Qiong;ZOU Hong-yun. Interleukin-8,interleukin-1 beta testing in patients with ankylosing spondylitis and clinical significance [J]. Clinical Focus, 2013, 28(4): 394-396. |
| [7] | . [J]. Clinical Focus, 2012, 27(20): 1818-1819. |
| [8] | . [J]. Clinical Focus, 2012, 27(5): 440-0. |
| [9] | KE Dian-shan;YU Xuan-hua;WANG Yan;REN Xin-ying;YE Hong-jiang;LI Yi-nong. Study on comprehensive work ability indicators in 206 cases of ankylosing spondylitis [J]. Clinical Focus, 2011, 26(23): 2052-2054. |
| [10] | . Study of bone mineral density of Han and Muslim nationality in normal people in Lanzhou [J]. CLINICAL FOCUS, 2010, 25(9): 747-749753. |
| [11] | . [J]. CLINICAL FOCUS, 2009, 24(18): 1616-1616. |
| [12] | . [J]. CLINICAL FOCUS, 2009, 24(15): 1343-1344. |
| [13] | . [J]. CLINICAL FOCUS, 2007, 22(20): 1491-1492. |
| [14] | . [J]. CLINICAL FOCUS, 2007, 22(19): 1406-1407. |
| [15] | . [J]. CLINICAL FOCUS, 2006, 21(8): 573-574. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||