Clinical Focus ›› 2025, Vol. 40 ›› Issue (1): 33-38.doi: 10.3969/j.issn.1004-583X.2025.01.005
Previous Articles Next Articles
Analysis of influencing factors of sleep quality and metabolically associated fatty liver disease in the physical examination population
Gou Caixia, Zhang Jie( ), Baoyixiamu·Ababaikeli , Wang Yiming, Yao Lei, Zheng Rongjiong, Pan Jinliang, Lu Xiaobo
), Baoyixiamu·Ababaikeli , Wang Yiming, Yao Lei, Zheng Rongjiong, Pan Jinliang, Lu Xiaobo
- Infectious Liver Disease Center,the First Affiliated Hospital of Xinjiang Medical University,Urumqi 830054,China
-
Received:2024-08-24Online:2025-01-20Published:2025-01-17 -
Contact:Zhang Jie,Email: zj12377@126.com
CLC Number:
Cite this article
Gou Caixia, Zhang Jie, Baoyixiamu·Ababaikeli , Wang Yiming, Yao Lei, Zheng Rongjiong, Pan Jinliang, Lu Xiaobo. Analysis of influencing factors of sleep quality and metabolically associated fatty liver disease in the physical examination population[J]. Clinical Focus, 2025, 40(1): 33-38.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2025.01.005
| 项目 | 非MAFLD组 ( | MAFLD组 ( | χ2/ | |
|---|---|---|---|---|
| 年龄(岁) | 43.03±10.99 | 46.62±11.05 | 1.753 | 0.080 |
| 性别[例(%)] | ||||
| 男 女 | 32(40.0) 48(60.0) | 37(61.7) 23(38.3) | 6.439 | 0.011 |
| 高血压[(%)] | ||||
| 无 有 | 71(88.7) 9(11.3) | 48(80.0) 12(20.0) | 2.059 | 0.151 |
Tab.1 General information between groups
| 项目 | 非MAFLD组 ( | MAFLD组 ( | χ2/ | |
|---|---|---|---|---|
| 年龄(岁) | 43.03±10.99 | 46.62±11.05 | 1.753 | 0.080 |
| 性别[例(%)] | ||||
| 男 女 | 32(40.0) 48(60.0) | 37(61.7) 23(38.3) | 6.439 | 0.011 |
| 高血压[(%)] | ||||
| 无 有 | 71(88.7) 9(11.3) | 48(80.0) 12(20.0) | 2.059 | 0.151 |
| 指标 | 非MAFLD组 ( | MAFLD组( | ||
|---|---|---|---|---|
| HGB(g/L) | 143.76±15.46 | 152.75±12.98 | -3.435 | 0.001 |
| PLT(×109 g/L) | 248.36±53.74 | 249.58±70.66 | -0.048 | 0.961 |
| ALB(g/L) | 44.95(43.54, 46.65) | 45.65±2.23 | -1.295 | 0.195 |
| T-BIL(μmol/L) | 13.56±4.01 | 16.46±6.02 | -2.684 | 0.007 |
| CR(μmol/L) | 76.41(68.49, 87.98) | 80.53±11.99 | -1.192 | 0.233 |
| UA(μmol/L) | 281.48(239.75, 355.72) | 369.01±91.85 | -4.114 | 0.000 |
| CK(U/L) | 86.34±29.82 | 102.86±56.12 | -1.916 | 0.055 |
| CK-MB(U/L) | 8.22(6.29, 11.42) | 8.59(6.53, 10.73) | -0.423 | 0.672 |
| GLU(mmol/L) | 4.81(4.36, 6.26) | 5.19(4.52, 7.64) | -0.973 | 0.061 |
| TG(mmol/L) | 1.04(0.79, 1.32) | 1.65(1.29, 2.38) | -5.512 | 0.000 |
| TC(mmol/L) | 4.56±0.80 | 4.84±0.86 | -2.103 | 0.035 |
| HDL-C(mmol/L) | 1.47(1.24, 1.86) | 1.13(0.95, 1.44) | -4.672 | 0.000 |
| ALT(U/L) | 16.94(12.60, 23.85) | 24.06(16.91, 36.87) | -4.057 | 0.000 |
| AST(U/L) | 19.55(16.45, 22.45) | 21.1(17.72, 26.47) | -2.080 | 0.038 |
| 甲胎蛋白(μg/L) | 3.11(2.36, 4.62) | 3.39(2.52, 5.26) | -1.126 | 0.260 |
Tab.2 Laboratory data between groups
| 指标 | 非MAFLD组 ( | MAFLD组( | ||
|---|---|---|---|---|
| HGB(g/L) | 143.76±15.46 | 152.75±12.98 | -3.435 | 0.001 |
| PLT(×109 g/L) | 248.36±53.74 | 249.58±70.66 | -0.048 | 0.961 |
| ALB(g/L) | 44.95(43.54, 46.65) | 45.65±2.23 | -1.295 | 0.195 |
| T-BIL(μmol/L) | 13.56±4.01 | 16.46±6.02 | -2.684 | 0.007 |
| CR(μmol/L) | 76.41(68.49, 87.98) | 80.53±11.99 | -1.192 | 0.233 |
| UA(μmol/L) | 281.48(239.75, 355.72) | 369.01±91.85 | -4.114 | 0.000 |
| CK(U/L) | 86.34±29.82 | 102.86±56.12 | -1.916 | 0.055 |
| CK-MB(U/L) | 8.22(6.29, 11.42) | 8.59(6.53, 10.73) | -0.423 | 0.672 |
| GLU(mmol/L) | 4.81(4.36, 6.26) | 5.19(4.52, 7.64) | -0.973 | 0.061 |
| TG(mmol/L) | 1.04(0.79, 1.32) | 1.65(1.29, 2.38) | -5.512 | 0.000 |
| TC(mmol/L) | 4.56±0.80 | 4.84±0.86 | -2.103 | 0.035 |
| HDL-C(mmol/L) | 1.47(1.24, 1.86) | 1.13(0.95, 1.44) | -4.672 | 0.000 |
| ALT(U/L) | 16.94(12.60, 23.85) | 24.06(16.91, 36.87) | -4.057 | 0.000 |
| AST(U/L) | 19.55(16.45, 22.45) | 21.1(17.72, 26.47) | -2.080 | 0.038 |
| 甲胎蛋白(μg/L) | 3.11(2.36, 4.62) | 3.39(2.52, 5.26) | -1.126 | 0.260 |
| 项目 | 非MAFLD组 ( | MAFLD组 ( | χ2值 | |
|---|---|---|---|---|
| 睡眠时长[例(%)] | ||||
| <4 h | 0 | 0 | ||
| 4~6 h | 34(42.5) | 28(46.7) | 0.244 | 0.885 |
| 6~8 h | 43(53.8) | 30(50.0) | ||
| >8 h | 3(3.7) | 2(3.3) | ||
| 睡眠质量[例(%)] | ||||
| 好(PSQI量表总分<5分) | 15(18.8) | 8(13.3) | ||
| PSQI量表总分=5分 | 16(20.0) | 10(16.7) | 1.221 | 0.543 |
| 差(PSQI量表总分>5分) | 49(61.2) | 42(70.0) | ||
| 日间小憩时间[例(%)] | ||||
| 0 | 35(43.7) | 15(25.0) | ||
| >0~30 min | 38(47.5) | 28(46.7) | 11.050 | 0.004 |
| 31~60 min | 7(8.8) | 17(28.3) | ||
| ≥61 min | 0 | 0 |
Tab.3 Sleep status between groups
| 项目 | 非MAFLD组 ( | MAFLD组 ( | χ2值 | |
|---|---|---|---|---|
| 睡眠时长[例(%)] | ||||
| <4 h | 0 | 0 | ||
| 4~6 h | 34(42.5) | 28(46.7) | 0.244 | 0.885 |
| 6~8 h | 43(53.8) | 30(50.0) | ||
| >8 h | 3(3.7) | 2(3.3) | ||
| 睡眠质量[例(%)] | ||||
| 好(PSQI量表总分<5分) | 15(18.8) | 8(13.3) | ||
| PSQI量表总分=5分 | 16(20.0) | 10(16.7) | 1.221 | 0.543 |
| 差(PSQI量表总分>5分) | 49(61.2) | 42(70.0) | ||
| 日间小憩时间[例(%)] | ||||
| 0 | 35(43.7) | 15(25.0) | ||
| >0~30 min | 38(47.5) | 28(46.7) | 11.050 | 0.004 |
| 31~60 min | 7(8.8) | 17(28.3) | ||
| ≥61 min | 0 | 0 |
| 项目 | 非MAFLD组 ( | MAFLD组 ( | ||
|---|---|---|---|---|
| 睡眠时长(h) | 7.00(6.00, 7.50) | 7.00(6.00, 7.50) | -0.334 | 0.738 |
| 日间小憩时间(min) | 20(0, 30) | 30(10, 40) | -3.083 | 0.002 |
Tab.4 Composition of sleep status between groups
| 项目 | 非MAFLD组 ( | MAFLD组 ( | ||
|---|---|---|---|---|
| 睡眠时长(h) | 7.00(6.00, 7.50) | 7.00(6.00, 7.50) | -0.334 | 0.738 |
| 日间小憩时间(min) | 20(0, 30) | 30(10, 40) | -3.083 | 0.002 |
| 组别 | 例数 | PSQI量表 总分 | 睡眠质量 因子得分 | 入睡时间 因子得分 | 睡眠时间 因子得分 | 睡眠效率 因子得分 | 睡眠障碍 因子得分 | 催眠药物 因子得分 | 日间功能障碍 因子得分 |
|---|---|---|---|---|---|---|---|---|---|
| MAFLD组 | 60 | 7(5, 9) | 1(1, 2) | 1(1, 1) | 1(1, 1) | 2(0, 3) | 1(1, 1) | 0(0, 0) | 1(1, 2) |
| 非MAFLD组 | 80 | 6(5, 7) | 1(1, 1) | 1(1, 1) | 1(1, 1) | 1(0, 3) | 1(1, 1) | 0(0, 0) | 1(1, 2) |
| -2.256 | -4.176 | -1.420 | -0.053 | -0.685 | -3.182 | 0.000 | -1.349 | ||
| 0.024 | 0.000 | 0.156 | 0.958 | 0.493 | 0.001 | 0.000 | 0.177 |
Tab.5 PSQI and sleep factors scores between groups
| 组别 | 例数 | PSQI量表 总分 | 睡眠质量 因子得分 | 入睡时间 因子得分 | 睡眠时间 因子得分 | 睡眠效率 因子得分 | 睡眠障碍 因子得分 | 催眠药物 因子得分 | 日间功能障碍 因子得分 |
|---|---|---|---|---|---|---|---|---|---|
| MAFLD组 | 60 | 7(5, 9) | 1(1, 2) | 1(1, 1) | 1(1, 1) | 2(0, 3) | 1(1, 1) | 0(0, 0) | 1(1, 2) |
| 非MAFLD组 | 80 | 6(5, 7) | 1(1, 1) | 1(1, 1) | 1(1, 1) | 1(0, 3) | 1(1, 1) | 0(0, 0) | 1(1, 2) |
| -2.256 | -4.176 | -1.420 | -0.053 | -0.685 | -3.182 | 0.000 | -1.349 | ||
| 0.024 | 0.000 | 0.156 | 0.958 | 0.493 | 0.001 | 0.000 | 0.177 |
| 因素 | 回归系数 | 标准误 | Wald χ2值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| T-BIL | 0.111 | 0.045 | 6.055 | 0.014 | 1.117 | 1.070 | 3.322 |
| HDL-C | -1.934 | 0.612 | 9.996 | 0.002 | 0.145 | -0.105 | 0.861 |
| 日间小憩时间 | 0.040 | 0.013 | 9.204 | 0.002 | 1.041 | 1.006 | 4.132 |
| 睡眠质量因子得分 | 1.527 | 0.466 | 10.752 | 0.001 | 4.605 | 2.362 | 6.521 |
| 睡眠障碍因子得分 | 1.485 | 0.639 | 5.398 | 0.020 | 4.413 | 2.856 | 7.411 |
| 常数 | -3.689 | 1.521 | 5.886 | 0.015 | 0.025 | -1.204 | 0.762 |
Tab.6 Logistic regression analysis for influencing factors of MAFLD
| 因素 | 回归系数 | 标准误 | Wald χ2值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| T-BIL | 0.111 | 0.045 | 6.055 | 0.014 | 1.117 | 1.070 | 3.322 |
| HDL-C | -1.934 | 0.612 | 9.996 | 0.002 | 0.145 | -0.105 | 0.861 |
| 日间小憩时间 | 0.040 | 0.013 | 9.204 | 0.002 | 1.041 | 1.006 | 4.132 |
| 睡眠质量因子得分 | 1.527 | 0.466 | 10.752 | 0.001 | 4.605 | 2.362 | 6.521 |
| 睡眠障碍因子得分 | 1.485 | 0.639 | 5.398 | 0.020 | 4.413 | 2.856 | 7.411 |
| 常数 | -3.689 | 1.521 | 5.886 | 0.015 | 0.025 | -1.204 | 0.762 |
| 变量 | T-BIL | HDL-C | 日间小憩时间 | 睡眠质量因子得分 | 睡眠障碍因子得分 | |
|---|---|---|---|---|---|---|
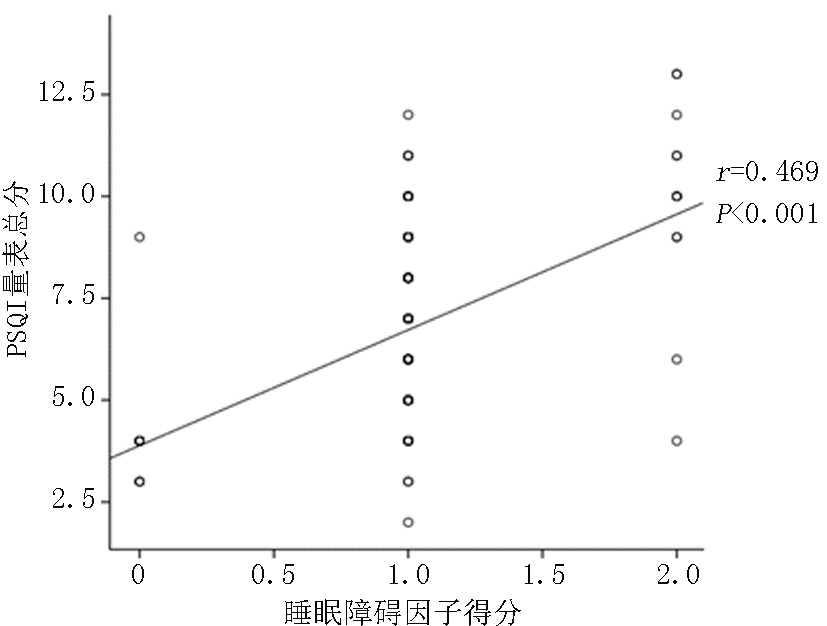
| PSQI量表总分 | -0.033 | -0.078 | 0.036 | 0.623 | 0.469 | |
| 0.699 | 0.358 | 0.671 | 0.000 | 0.000 |
Tab.7 Correlation between PSQI and influencing factors of MAFLD
| 变量 | T-BIL | HDL-C | 日间小憩时间 | 睡眠质量因子得分 | 睡眠障碍因子得分 | |
|---|---|---|---|---|---|---|
| PSQI量表总分 | -0.033 | -0.078 | 0.036 | 0.623 | 0.469 | |
| 0.699 | 0.358 | 0.671 | 0.000 | 0.000 |
| [1] |
Younossi ZM, Golabi P, de Avila L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis[J]. J Hepatol, 2019, 71(4): 793-801.
doi: S0168-8278(19)30393-9 pmid: 31279902 |
| [2] | 黄饺饺, 易默, 史丽萍. 代谢相关性脂肪性肝病的相关影响因素[J]. 临床医学进展, 2022, 12(1):331-336. |
| [3] | 王治兰, 李良平. 脂肪肝的营养处方[J]. 肝博士, 2016(4):51-53. |
| [4] |
Huang T, Behary J, Zekry A. Non-alcoholic fatty liver disease: A review of epidemiology, risk factors, diagnosis and management[J]. Intern Med J, 2020, 50(9): 1038-1047.
doi: 10.1111/imj.14709 pmid: 31760676 |
| [5] |
Younossi ZM. Non-alcoholic fatty liver disease-a global public health perspective[J]. J Hepatol, 2019, 70(3): 531-544.
doi: S0168-8278(18)32517-0 pmid: 30414863 |
| [6] | Fouad Y, Waked I, Bollipo S, et al. What's in a name? Renaming ‘NAFLD’to ‘MAFLD’[J]. Liver Int, 2020, 40(6): 1254-1261. |
| [7] | 中华医学会肝病学分会. 代谢相关(非酒精性)脂肪性肝病防治指南(2024年版)[J]. 中华肝脏病杂, 2024, 32(5):418-434. |
| [8] | 韩琳, 谢欢, 孙颖, 等. 代谢相关脂肪性肝病的诊断与评估现状[J]. 肝脏, 2021, 26(2): 205-210. |
| [9] |
Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement[J]. J Hepatol, 2020, 73(1): 202-209.
doi: S0168-8278(20)30201-4 pmid: 32278004 |
| [10] | 范建高. 代谢相关脂肪性肝病现已成为我国第一大慢性肝病[J]. 中华医学信息导报, 2021, 36(6): 6. |
| [11] | 崔月萌. 睡眠障碍与非酒精性脂肪肝病相关性研究进展[J]. 现代医药卫生, 2022, 38(22):3899-3903. |
| [12] | Miyake T, Kumagi T, Furukawa S, et al. Short sleep duration reduces the risk of nonalcoholic fatty liver disease onset in men:A community-based longitudinal cohort study[J]. J Gastroenterol, 2015, 50(5):583-589. |
| [13] |
Okamura T, Hashimoto Y, Hamaguchi M, et al. Short sleep duration is a risk of incident nonalcoholic fatty liver disease:A population-based longitudinal study[J]. J Gastrointestin Liver Dis, 2019, 28(1):73-81.
doi: 10.15403/jgld.2014.1121.281.alc pmid: 30851175 |
| [14] | Lou TW, Yang RX, Fan JG. The global burden of fatty liver disease: The major impact of China[J]. Hepatobiliary Surg Nutr, 2024, 13(1):119-123. |
| [15] | Ghevariya V, Sandar N, Patel K, et al. Knowing what’s out there: Awareness of non-alcoholic fatty liver disease[J]. Front Med (Lausanne), 2014, 1: 4. |
| [16] | Maurice J, Manousou P. Non-alcoholic fatty liver disease[J]. Clin Med (Northfield Il), 2018, 18(3):245-250. |
| [17] | Wu T, Ye J, Mo S, et al. Impact of nomenclature as metabolic associated steatotic liver disease on steatotic liver disease prevalence and screening: A prospective population survey in Asians[J]. J Gastroenterol Hepatol, 2024, 39(8):1636-1647. |
| [18] |
Zhou J, Zhou F, Wang W, et al. Epidemiological features of NAFLD from 1999 to 2018 in China[J]. Hepatology, 2020, 71(5):1851-1864.
doi: 10.1002/hep.31150 pmid: 32012320 |
| [19] | 劳雪莲, 沈丽丽, 陈艳红, 等. 不同年龄非酒精性单纯性脂肪肝患者受控衰减参数、血脂、肠道菌群与颈动脉粥样硬化的关系[J]. 中国老年学杂志, 2023, 43(11):2619-2623. |
| [20] | Yang J, Luo S, Li R, et al. Sleep factors in relation to metabolic dysfunction-associated fatty liver disease in middle-aged and elderly Chinese[J]. J Clin Endocrinol Metab, 2022, 107(10):2874-2882. |
| [21] | 石丽敏, 孙剑. 2型糖尿病合并非酒精性脂肪性肝病患者血清铁蛋白、胆红素水平与代谢指标的相关性研究[J]. 中国医药科学, 2024, 14(14):159-162, 170. |
| [22] | 石红宾, 李中南, 陈明月, 等. 2型糖尿病合并痛风性关节炎患者单核细胞高密度脂蛋白胆固醇比值与非酒精性脂肪肝关系研究[J]. 中国实用内科杂志, 2024, 44(5):397-402. |
| [1] | Xiong Lu, Guo Lian. Correlation of 25(OH)D and SUA/SCr with type 2 diabetes mellitus combined with non-alcoholic fatty liver disease [J]. Clinical Focus, 2024, 39(8): 706-711. |
| [2] | Cao Yumeng, Zhang Haiyan, Liu Lixin. Correlation between pathological changes and serum ferritin and iron levels in nonalcoholic fatty liver disease: A meta-analysis [J]. Clinical Focus, 2023, 38(3): 197-207. |
| [3] | Li Guohuan, Xie Xu, Huang Zhixia, Zhang Mingye, Tang Yunyun. Quantitative evaluation of transient elastography and acoustic radiation force pulse imaging for non-alcoholic fatty liver disease [J]. Clinical Focus, 2021, 36(6): 535-539. |
| [4] | Ye Jingjing, Qin Yu, Zhao Li, Yang Ling. Relationship between a body shape index and newly-diagnosed type 2 diabetes mellitus complicated with non-alcoholic fatty liver disease [J]. Clinical Focus, 2021, 36(2): 144-148. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||