Clinical Focus ›› 2024, Vol. 39 ›› Issue (11): 993-999.doi: 10.3969/j.issn.1004-583X.2024.11.006
Previous Articles Next Articles
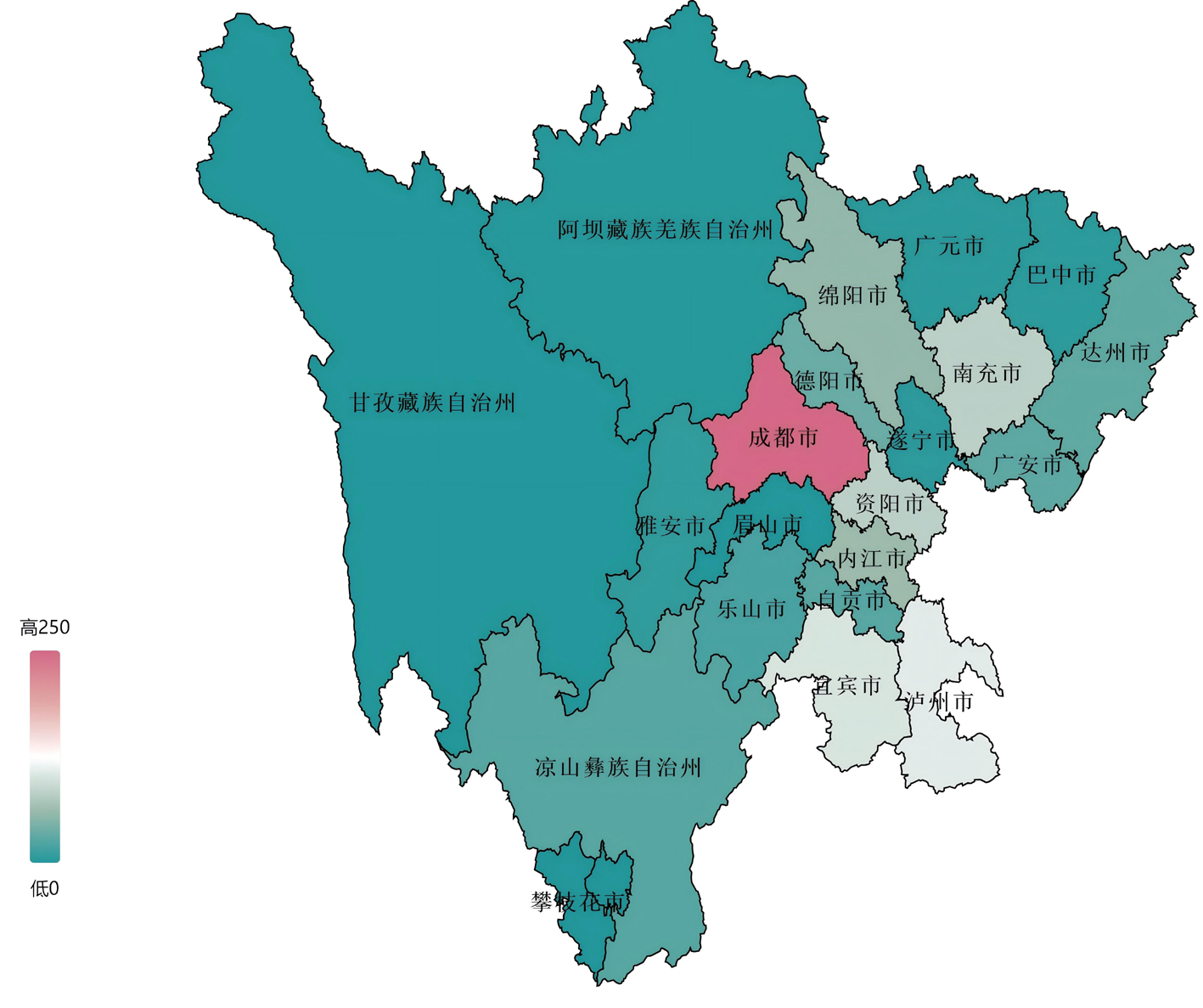
Survey of the application and demands of critical care ultrasound in critical illnesses in tertiary hospitals of Sichuan Province
Zeng Xueying1, Yin Wanhong1( ), Qin Yao1, Wang Yiping2, Cao Lianghai3, Lei Xianying4, Liao Xuelian1,5
), Qin Yao1, Wang Yiping2, Cao Lianghai3, Lei Xianying4, Liao Xuelian1,5
- 1. Intensive Care Unit,West China Hospital,Sichuan University,Chengdu,610041,China
2. Department of Critical Care Medicine,Sichuan Academy of Medical Sciences,Sichuan Provincial People’s Hospital,Chengdu 610072,China
3. Intensive Care Unit,the Second People’s Hospital of Yibin,Yibin 644000,China
4. Department of Critical Care Medicine,the Affiliated Hospital of Southwest Medical University,Luzhou 646000,China
5. Department of Critical Care Medicine, West China Tianfu Hospital,Sichuan University,Chengdu 610213,China
-
Received:2024-08-30Online:2024-11-20Published:2024-12-04 -
Contact:Yin Wanhong E-mail:yinwanhong@wchscu.cn
CLC Number:
Cite this article
Zeng Xueying, Yin Wanhong, Qin Yao, Wang Yiping, Cao Lianghai, Lei Xianying, Liao Xuelian. Survey of the application and demands of critical care ultrasound in critical illnesses in tertiary hospitals of Sichuan Province[J]. Clinical Focus, 2024, 39(11): 993-999.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.11.006
| 累计进行重症超声 评估情况(例次) | 医生 | 护士 | |||
|---|---|---|---|---|---|
| 人数 | 占比(%) | 人数 | 占比(%) | ||
| 从未使用 | 76 | 14.73 | 247 | 58.95 | |
| 50以下 | 181 | 35.08 | 126 | 30.07 | |
| 50~200 | 148 | 28.68 | 32 | 7.64 | |
| 200~500 | 68 | 13.18 | 9 | 2.15 | |
| 500以上 | 43 | 8.33 | 5 | 1.19 | |
Tab.1 Application number of critical care ultrasound in medical staff
| 累计进行重症超声 评估情况(例次) | 医生 | 护士 | |||
|---|---|---|---|---|---|
| 人数 | 占比(%) | 人数 | 占比(%) | ||
| 从未使用 | 76 | 14.73 | 247 | 58.95 | |
| 50以下 | 181 | 35.08 | 126 | 30.07 | |
| 50~200 | 148 | 28.68 | 32 | 7.64 | |
| 200~500 | 68 | 13.18 | 9 | 2.15 | |
| 500以上 | 43 | 8.33 | 5 | 1.19 | |
| 超声机配置情况 | 三甲 | 三乙 | |
|---|---|---|---|
| 超声机台数(台) | 0 | 9(9.89) | 28(37.33) |
| 1 | 63(69.23) | 44(58.67) | |
| 2 | 14(15.38) | 3(4.00) | |
| 3 | 4(4.40) | / | |
| 4 | 1(1.10) | / | |
| 配置超声机类型 | 掌上超声 | 3 | 1 |
| 便携超声/笔记本 | 27 | 22 | |
| 台式超声 | 56 | 30 | |
| 其他 | 9 | 24 | |
Tab.2 Configuration of critical care ultrasound in critical care departments of 166 hospitals (number of hospitals [n, %])
| 超声机配置情况 | 三甲 | 三乙 | |
|---|---|---|---|
| 超声机台数(台) | 0 | 9(9.89) | 28(37.33) |
| 1 | 63(69.23) | 44(58.67) | |
| 2 | 14(15.38) | 3(4.00) | |
| 3 | 4(4.40) | / | |
| 4 | 1(1.10) | / | |
| 配置超声机类型 | 掌上超声 | 3 | 1 |
| 便携超声/笔记本 | 27 | 22 | |
| 台式超声 | 56 | 30 | |
| 其他 | 9 | 24 | |
| 疾病群体分类 | 进行重症超声评估的比例 | ||||
|---|---|---|---|---|---|
| 无 | 20%以下 | 20%~50% | 50%~80% | 80%~100% | |
| 休克 | 6.19% | 19.03% | 17.92% | 22.79% | 34.07% |
| ARDS | 7.74% | 21.68% | 19.69% | 26.55% | 24.34% |
| TBI | 19.25% | 27.21% | 21.46% | 17.70% | 14.38% |
| 脑卒中 | 25.00% | 34.51% | 19.69% | 13.50% | 7.30% |
| 脓毒症 | 6.64% | 15.49% | 14.16% | 26.33% | 37.39% |
| 胰腺炎 | 14.82% | 18.36% | 14.16% | 24.34% | 28.32% |
| CPR术后 | 11.50% | 18.81% | 15.49% | 21.68% | 32.52% |
| 急性呼吸循环障碍(1 h内) | 10.62% | 30.53% | 23.67% | 17.26% | 17.92% |
Tab.3 Use of critical care ultrasound in assessing critical illnesses of physicians
| 疾病群体分类 | 进行重症超声评估的比例 | ||||
|---|---|---|---|---|---|
| 无 | 20%以下 | 20%~50% | 50%~80% | 80%~100% | |
| 休克 | 6.19% | 19.03% | 17.92% | 22.79% | 34.07% |
| ARDS | 7.74% | 21.68% | 19.69% | 26.55% | 24.34% |
| TBI | 19.25% | 27.21% | 21.46% | 17.70% | 14.38% |
| 脑卒中 | 25.00% | 34.51% | 19.69% | 13.50% | 7.30% |
| 脓毒症 | 6.64% | 15.49% | 14.16% | 26.33% | 37.39% |
| 胰腺炎 | 14.82% | 18.36% | 14.16% | 24.34% | 28.32% |
| CPR术后 | 11.50% | 18.81% | 15.49% | 21.68% | 32.52% |
| 急性呼吸循环障碍(1 h内) | 10.62% | 30.53% | 23.67% | 17.26% | 17.92% |
| 项目 | 应用重症超声比例 | ||||
|---|---|---|---|---|---|
| 无 | 20%以下 | 20%~50% | 50%~80% | 80%~100% | |
| 深静脉穿刺 | 4.87% | 17.04% | 20.13% | 26.55% | 31.42% |
| 胸腹腔穿刺 | 5.09% | 11.73% | 9.73% | 15.27% | 58.19% |
| 心包穿刺 | 33.19% | 17.48% | 6.86% | 6.86% | 35.62% |
| ECMO置管/引导 | 51.55% | 12.17% | 4.20% | 5.09% | 26.11% |
| IABP置管/引导 | 52.88% | 13.72% | 6.86% | 7.52% | 18.36% |
Tab.4 Application of critical care ultrasound in invasive diagnosis and treatment of critical illnesses by physicians
| 项目 | 应用重症超声比例 | ||||
|---|---|---|---|---|---|
| 无 | 20%以下 | 20%~50% | 50%~80% | 80%~100% | |
| 深静脉穿刺 | 4.87% | 17.04% | 20.13% | 26.55% | 31.42% |
| 胸腹腔穿刺 | 5.09% | 11.73% | 9.73% | 15.27% | 58.19% |
| 心包穿刺 | 33.19% | 17.48% | 6.86% | 6.86% | 35.62% |
| ECMO置管/引导 | 51.55% | 12.17% | 4.20% | 5.09% | 26.11% |
| IABP置管/引导 | 52.88% | 13.72% | 6.86% | 7.52% | 18.36% |
| 项目 | 医生 | 护士 | |||||
|---|---|---|---|---|---|---|---|
| 无 | 0~50% | 50%~100% | 无 | 0~50% | 50%~100% | ||
| 采用重症超声评估 | 18.14% | 40.27% | 41.59% | 9.23% | 39.49% | 51.28% | |
| 使用后改变决策 | 17.92% | 43.14% | 38.94% | 10.26% | 30.77% | 58.97% | |
| 使用后提高成功率 | 17.26% | 38.27% | 44.47% | 9.74% | 27.18% | 63.08% | |
| 重症超声未提供有效信息 | 27.21% | 60.18% | 12.61% | 21.03% | 43.59% | 35.38% | |
| 导致误判 | 29.42% | 63.94% | 6.64% | 24.62% | 45.64% | 29.74% | |
Tab.5 Evaluation of peripheral arteriovenous puncture by medical staff using critical care ultrasound in critical illnesses within the past 3 years
| 项目 | 医生 | 护士 | |||||
|---|---|---|---|---|---|---|---|
| 无 | 0~50% | 50%~100% | 无 | 0~50% | 50%~100% | ||
| 采用重症超声评估 | 18.14% | 40.27% | 41.59% | 9.23% | 39.49% | 51.28% | |
| 使用后改变决策 | 17.92% | 43.14% | 38.94% | 10.26% | 30.77% | 58.97% | |
| 使用后提高成功率 | 17.26% | 38.27% | 44.47% | 9.74% | 27.18% | 63.08% | |
| 重症超声未提供有效信息 | 27.21% | 60.18% | 12.61% | 21.03% | 43.59% | 35.38% | |
| 导致误判 | 29.42% | 63.94% | 6.64% | 24.62% | 45.64% | 29.74% | |
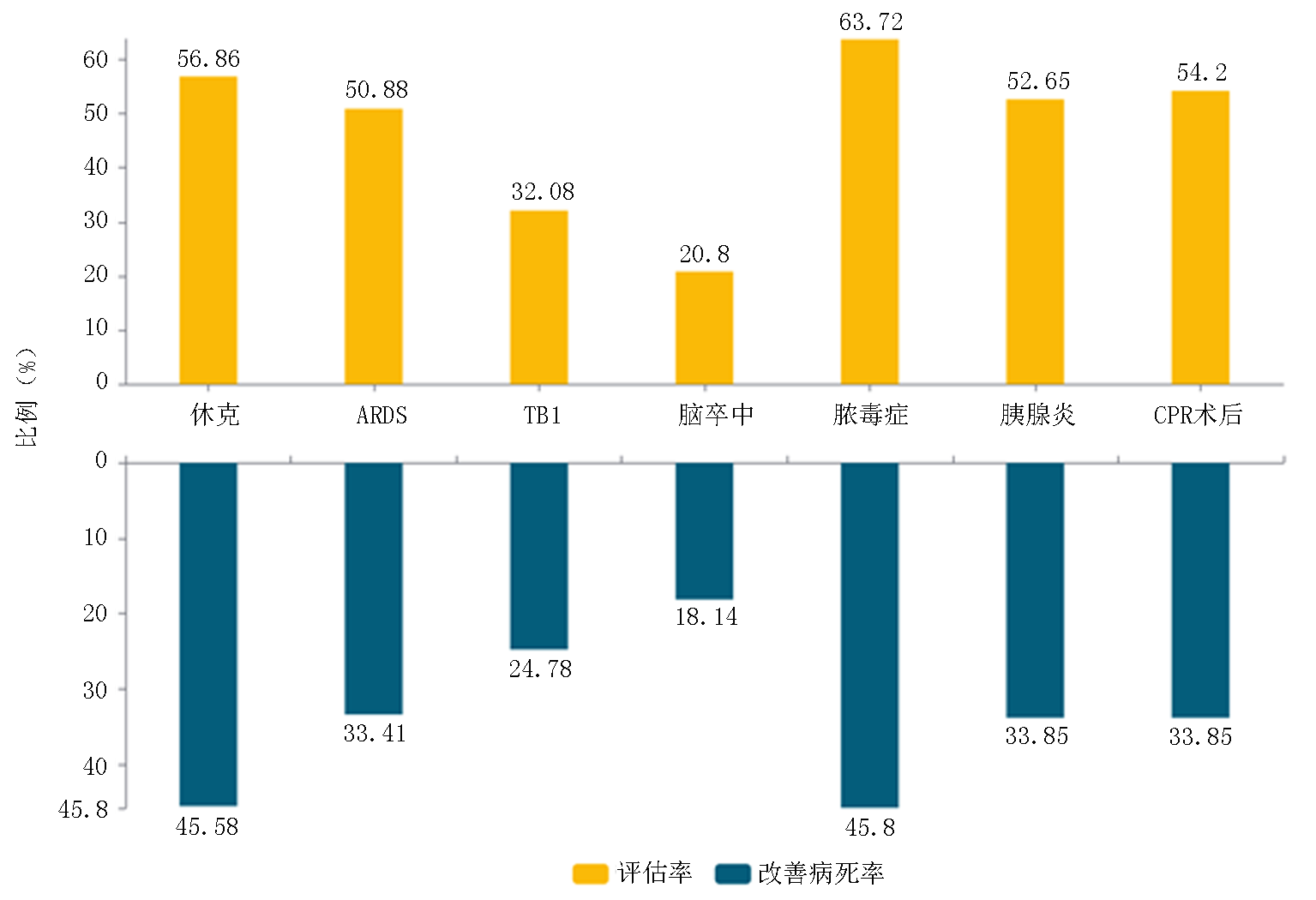
Fig.2 The proportion of critical syndrome with 50% use of critical care ultrasound in critical ill patients and the change rate of diagnosis and treatment decision
| 比例/准确率 | 完整方案化检查 (比例) | 评估脏器异常情况 (准确率) | 解读病理生理异常及 机体反应失调(准确率) | 获取达质控标准图像 (标准率) | 标准率 |
|---|---|---|---|---|---|
| 0~20% | 63.05% | 24.56% | 31.64% | 27.21% | 10%以下 |
| 20%~50% | 22.35% | 47.79% | 46.68% | 41.59% | 10%~50% |
| 50%~80% | 11.06% | 22.57% | 18.58% | 18.81% | 50%以上 |
| 80%以上 | 3.54% | 5.09% | 3.10% | 12.39% | 不清楚标准 |
Tab.6 Mastery of critical care ultrasound in physicians
| 比例/准确率 | 完整方案化检查 (比例) | 评估脏器异常情况 (准确率) | 解读病理生理异常及 机体反应失调(准确率) | 获取达质控标准图像 (标准率) | 标准率 |
|---|---|---|---|---|---|
| 0~20% | 63.05% | 24.56% | 31.64% | 27.21% | 10%以下 |
| 20%~50% | 22.35% | 47.79% | 46.68% | 41.59% | 10%~50% |
| 50%~80% | 11.06% | 22.57% | 18.58% | 18.81% | 50%以上 |
| 80%以上 | 3.54% | 5.09% | 3.10% | 12.39% | 不清楚标准 |
| 重症超声应用过程中存在的困难 | 计数 | 百分比 |
|---|---|---|
| 有资质人员不足 | 740 | 79.14% |
| 培训课程覆盖不够 | 584 | 62.46% |
| 重症超声设备不足 | 581 | 62.14% |
| 重症超声图像判读困难 | 538 | 57.54% |
| 重症超声信息解读困难 | 497 | 53.16% |
| 可视化信息太丰富应用困难 | 341 | 36.47% |
| 检查目的不清晰 | 228 | 24.39% |
| 其他 | 48 | 5.13% |
Tab.7 Difficulties in the application of critical care ultrasound
| 重症超声应用过程中存在的困难 | 计数 | 百分比 |
|---|---|---|
| 有资质人员不足 | 740 | 79.14% |
| 培训课程覆盖不够 | 584 | 62.46% |
| 重症超声设备不足 | 581 | 62.14% |
| 重症超声图像判读困难 | 538 | 57.54% |
| 重症超声信息解读困难 | 497 | 53.16% |
| 可视化信息太丰富应用困难 | 341 | 36.47% |
| 检查目的不清晰 | 228 | 24.39% |
| 其他 | 48 | 5.13% |
| [1] | 张秋彬, 徐军, 朱华栋, 等. 2018年国内300家三级医院急诊科即时超声检查现况调查[J]. 中华危重病急救医学, 2019, 31(4):484-487. |
| [2] | 王小亭, 刘大为, 于凯江, 等. 中国重症超声专家共识[J]. 临床荟萃, 2017, 32(5):369-383. |
| [3] |
Zieleskiewicz L, Fresco R, Duclos G, et al. Integrating extended focused assessment with sonography for trauma (eFAST) in the initial assessment of severe trauma: Impact on the management of 756 patients[J]. Injury, 2018, 49(10):1774-1780.
doi: S0020-1383(18)30358-9 pmid: 30017184 |
| [4] |
Gaspari R, Weekes A, Adhikari S, et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest[J]. Resuscitation, 2016, 109:33-39.
doi: S0300-9572(16)30478-6 pmid: 27693280 |
| [5] | Barjaktarevic I, Toppen WE, Hu S, et al. Ultrasound assessment of the change in carotid corrected flow time in fluid responsiveness in undifferentiated shock[J]. Crit Care Med, 2018, 46(11):e1040-e1046. |
| [6] |
Lichtenstein DA. BLUE-protocol and FALLS-protocol: Two applications of lung ultrasound in the critically ill[J]. Chest, 2015, 147(6):1659-1670.
doi: S0012-3692(15)37223-8 pmid: 26033127 |
| [7] |
Patel CJ, Bhatt HB, Parikh SN, et al. Bedside lung ultrasound in emergency protocol as a diagnostic tool in patients of acute respiratory distress presenting to emergency department[J]. J Emerg Trauma Shock, 2018, 11(2):125-129.
doi: 10.4103/JETS.JETS_21_17 pmid: 29937643 |
| [8] | 国家心血管病中心, 国家心血管病专家委员会心力衰竭专业委员会, 中国医师协会心力衰竭专业委员会, 等. 国家心力衰竭指南2023[J]. 中华心力衰竭和心肌病杂志, 2023, 7(4): 215-311. |
| [9] | 王小亭, 刘大为, 于凯江, 等. 中国重症超声专家共识[J]. 中华内科杂志, 2016, 55(11):900-912. |
| [10] | 尹万红, 王小亭, 刘大为, 等. 重症超声临床应用技术规范[J]. 中华内科杂志, 2018, 57(6):397-417. |
| [11] | 尹万红, 王小亭, 刘大为, 等. 重症超声应用及培训原则与质量控制标准[J]. 中华内科杂志, 2022, 61(6):631-643. |
| [12] | Quintard H, Philip I, Ichai C. French survey on current use of ultrasound in the critical care unit: ECHOREA[J]. Ann Fr Anesth Reanim, 2011, 30(11):e69-73. |
| [13] |
Seymour CW, Rosengart MR. Septic shock: Advances in diagnosis and treatment[J]. JAMA, 2015, 314(7):708-717.
doi: 10.1001/jama.2015.7885 pmid: 26284722 |
| [14] | Cecconi M, De Backer D, Antonelli M, et al. Consensus on circulatory shock and hemodynamic monitoring: Task force of the European Society of Intensive Care Medicine[J]. Intensive Care Med, 2014, 40(12):1795-1815. |
| [15] | Wyckoff MH, Greif R, Morley PT, et al. 2022 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: Summary from the basic life support; Advanced life support; Pediatric life support; Neonatal life support; Education, implementation, and teams; and first aid task forces[J]. Circulation, 2022, 146(25):e483-e557. |
| [16] | Takekawa H, Tsukui D, Kobayasi S, et al. Point-of-care ultrasound for stroke patients in the emergency room[J]. J Med Ultrason (2001), 2022, 49(4):581-592. |
| [17] |
Zieleskiewicz L, Muller L, Lakhal K, et al. Point-of-care ultrasound in intensive care units: Assessment of 1073 procedures in a multicentric, prospective, observational study[J]. Intensive Care Med, 2015, 41(9):1638-1647.
doi: 10.1007/s00134-015-3952-5 pmid: 26160727 |
| [18] | Boulet N, Muller L, Rickard CM, et al. How to improve the efficiency and the safety of real-time ultrasound-guided central venous catheterization in 2023: A narrative review{j]. Ann Intensive Care, 2023, 13(1):46. |
| [19] | 王慧, 何伟, 丁欣, 等. 重症超声专项培训在重症医学教学中的作用[J]. 中国中西医结合急救杂志, 2023, 30(4):471-475. |
| [20] | 国家卫生健康委员会. 重症医学科建设与管理指南:卫办医政发〔2009〕23号[EB/OL]. (2009-02-26)[2023-12-01]. http://www.nhc.gov.cn/yzygj. |
| [21] | 省卫生健康委. 四川省医院机构信息[EB/OL]. 2023-08-29. https://scdata.net.cn/oportal/catalog/7d4aa55483164bbfb11849772149acc8. |
| [1] | . [J]. Clinical Focus, 2024, 39(9): 837-841. |
| [2] | . [J]. Clinical Focus, 2023, 38(2): 175-180. |
| [3] | . [J]. Clinical Focus, 2022, 37(9): 834-837. |
| [4] | Dan Haijun. Advances in differential diagnosis of thyroid nodules using high-resolution ultrasound [J]. Clinical Focus, 2016, 31(3): 286-288. |
| [5] | WANG Yong;BAI Ling;MAO Jing-ning;CHEN Wei;FAN Xue;ZHANG Yan;CHEN Cui-jing. Analysis of ultrasonic image signature in male breast cancer [J]. Clinical Focus, 2012, 27(5): 382-385. |
| [6] | WANG Xue-ou;LI Hui-zhen;LI Hong-mei;CHEN Li-ping;CUI Zhao-wen;QIU Wei. Scattered district feature and reason analysis of hyperlipidemia without symptoms and carotid atherosclerosis stenosis in Beidaihe area [J]. CLINICAL FOCUS, 2011, 26(2): 121-124. |
| [7] | WANG Wei-ping;ZHANG Yu-qiang;MEI Chang-lin. Microinflammatory state correlates cardiac structure and fuction in patients with maintenance hemodialysis [J]. CLINICAL FOCUS, 2011, 26(1): 1-5. |
| [8] | MENG Xuan;WANG Xin;SHI Zheng-hong;LI Xing-jie. Clinical analysis of intracerebral circulation changes in comatose patients after cardiopulmonary resuscitation [J]. CLINICAL FOCUS, 2010, 25(5): 394-396. |
| [9] | . [J]. CLINICAL FOCUS, 2009, 24(20): 1814-1815. |
| [10] | . [J]. CLINICAL FOCUS, 2009, 24(17): 1505-0. |
| [11] | . [J]. CLINICAL FOCUS, 2009, 24(6): 519-0. |
| [12] | . [J]. CLINICAL FOCUS, 2008, 23(19): 1392-1393. |
| [13] | . [J]. CLINICAL FOCUS, 2008, 23(15): 1092-1093. |
| [14] | . [J]. CLINICAL FOCUS, 2008, 23(4): 274-276. |
| [15] | . [J]. CLINICAL FOCUS, 2006, 21(15): 1123-1125. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||