Clinical Focus ›› 2022, Vol. 37 ›› Issue (3): 243-247.doi: 10.3969/j.issn.1004-583X.2022.03.008
Previous Articles Next Articles
Monitoring significance of CD4+ T lymphocyte count on evaluating frailty status of chronic renal failure in patients
Li Yingying1a, Li Ting1b, Zhang Ming1a, Fan Minghua2, Xing Guangqun1a( )
)
- 1a. Department of Nephropathy, Affiliated Hospital of Qingdao University, Qingdao 266555, China
1b. Phase I Clinical Research Center, Affiliated Hospital of Qingdao University, Qingdao 266555, China
2. Department of Nephrology, People's Hospital of Rizhao, Rizhao 276800, China
-
Received:2021-06-21Online:2022-03-20Published:2022-04-02 -
Contact:Xing Guangqun E-mail:gqx99monash@163.com
CLC Number:
Cite this article
Li Yingying, Li Ting, Zhang Ming, Fan Minghua, Xing Guangqun. Monitoring significance of CD4+ T lymphocyte count on evaluating frailty status of chronic renal failure in patients[J]. Clinical Focus, 2022, 37(3): 243-247.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2022.03.008
| 项目 | A组(n=67) | B组(n=175) | C组(n=139) | 统计值 | P值 |
|---|---|---|---|---|---|
| 年龄 | 60.00(54.09,62.87) | 65.00(59.97,64.99) | 58.00(55.78,61.19) | H=1.290 | 0.069 |
| 性别[例(%)] | |||||
| 男 女 | 35(52.2) 32(47.8) | 86(49.1) 89(50.9) | 77(55.4) 62(44.6) | χ2=2.567 | 0.277 |
| 透析方式[例(%)] | |||||
| 血液透析 腹膜透析 | 19(28.4) 11(16.4) | 78(44.6) 22(12.6) | 43(30.9) 22(15.8) | χ2=12.704 | 0.122 |
| 原发病[例(%)] | |||||
| 慢性肾小球肾炎 | 22(32.8) | 58(33.1) | 53(38.1) | χ2=0.125 | 0.940 |
| 糖尿病肾病 | 21(31.3) | 59(33.7) | 45(32.4) | χ2=0.163 | 0.922 |
| 高血压肾病 | 16(23.9) | 28(16.0) | 23(16.6) | χ2=2.080 | 0.354 |
| 痛风性肾病 | 2(3.0) | 2(1.1) | 2(1.4) | χ2=1.052 | 0.591 |
| 梗阻性肾病 | 1(1.5) | 7(4.0) | 5(3.6) | χ2=0.967 | 0.617 |
| 多囊肾 | 0(0) | 8(4.6) | 2(1.4) | χ2=4.943 | 0.084 |
| 药物所致肾衰竭 | 1(1.5) | 3(1.7) | 1(0.7) | χ2=0.537 | 0.764 |
| 其他原因 | 4(6.0) | 10(5.7) | 8(5.8) | χ2=0.017 | 0.991 |
| 项目 | A组(n=67) | B组(n=175) | C组(n=139) | 统计值 | P值 |
|---|---|---|---|---|---|
| 年龄 | 60.00(54.09,62.87) | 65.00(59.97,64.99) | 58.00(55.78,61.19) | H=1.290 | 0.069 |
| 性别[例(%)] | |||||
| 男 女 | 35(52.2) 32(47.8) | 86(49.1) 89(50.9) | 77(55.4) 62(44.6) | χ2=2.567 | 0.277 |
| 透析方式[例(%)] | |||||
| 血液透析 腹膜透析 | 19(28.4) 11(16.4) | 78(44.6) 22(12.6) | 43(30.9) 22(15.8) | χ2=12.704 | 0.122 |
| 原发病[例(%)] | |||||
| 慢性肾小球肾炎 | 22(32.8) | 58(33.1) | 53(38.1) | χ2=0.125 | 0.940 |
| 糖尿病肾病 | 21(31.3) | 59(33.7) | 45(32.4) | χ2=0.163 | 0.922 |
| 高血压肾病 | 16(23.9) | 28(16.0) | 23(16.6) | χ2=2.080 | 0.354 |
| 痛风性肾病 | 2(3.0) | 2(1.1) | 2(1.4) | χ2=1.052 | 0.591 |
| 梗阻性肾病 | 1(1.5) | 7(4.0) | 5(3.6) | χ2=0.967 | 0.617 |
| 多囊肾 | 0(0) | 8(4.6) | 2(1.4) | χ2=4.943 | 0.084 |
| 药物所致肾衰竭 | 1(1.5) | 3(1.7) | 1(0.7) | χ2=0.537 | 0.764 |
| 其他原因 | 4(6.0) | 10(5.7) | 8(5.8) | χ2=0.017 | 0.991 |
| 组别 | ALB (g/L) | PAB (mg/L) | TP (g/L) | T淋巴细胞计数 (×109/L) | SCr (μmol/L) | 估算肾小球滤过率 [ml/ (min·1.73 m2)] | TC (mmol/L) | LDL-C (mmol/L) |
|---|---|---|---|---|---|---|---|---|
| A组 | 26.25 (23.78,29.49) | 179.00 (134.98,228.12) | 53.50 (39.13,91.61) | 0.61 (0.24,1.76) | 541.60 (415.23,659.40) | 6.00 (5.32,10.68) | 3.55 (2.83,4.98) | 2.84 (2.18,17.57) |
| B组 | 31.60 (29.79,32.46) | 219.00 (201.86,251.95) | 60.40 (59.22,66.35) | 0.90 (0.93,0.90) | 521.50 (433.25,581.09) | 6.00 (7.42,17.03) | 4.2 (0.11,17.62) | 2.70 (2.44,3.12) |
| C组 | 33.91 (34.25,40.94) | 211.50 (197.56,246.38) | 58.40 (56.66,64.57) | 1.36 (1.31,1.65) | 573.75 (485.04,645.62) | 6.00 (6.25,9.75) | 3.81 (3.57,4.89) | 2.59 (2.51,3.73) |
| 统计值 | H=26.485 | H=15.961 | H=14.053 | H=2.492 | H=1.109 | H=1.057 | H=3.920 | H=2.588 |
| P值 | <0.01 | <0.01 | <0.01 | 0.077 | 0.582 | 0.346 | 0.144 | 0.080 |
| 组别 | ALB (g/L) | PAB (mg/L) | TP (g/L) | T淋巴细胞计数 (×109/L) | SCr (μmol/L) | 估算肾小球滤过率 [ml/ (min·1.73 m2)] | TC (mmol/L) | LDL-C (mmol/L) |
|---|---|---|---|---|---|---|---|---|
| A组 | 26.25 (23.78,29.49) | 179.00 (134.98,228.12) | 53.50 (39.13,91.61) | 0.61 (0.24,1.76) | 541.60 (415.23,659.40) | 6.00 (5.32,10.68) | 3.55 (2.83,4.98) | 2.84 (2.18,17.57) |
| B组 | 31.60 (29.79,32.46) | 219.00 (201.86,251.95) | 60.40 (59.22,66.35) | 0.90 (0.93,0.90) | 521.50 (433.25,581.09) | 6.00 (7.42,17.03) | 4.2 (0.11,17.62) | 2.70 (2.44,3.12) |
| C组 | 33.91 (34.25,40.94) | 211.50 (197.56,246.38) | 58.40 (56.66,64.57) | 1.36 (1.31,1.65) | 573.75 (485.04,645.62) | 6.00 (6.25,9.75) | 3.81 (3.57,4.89) | 2.59 (2.51,3.73) |
| 统计值 | H=26.485 | H=15.961 | H=14.053 | H=2.492 | H=1.109 | H=1.057 | H=3.920 | H=2.588 |
| P值 | <0.01 | <0.01 | <0.01 | 0.077 | 0.582 | 0.346 | 0.144 | 0.080 |
| 组别 | APACHEⅡ评分(分) | SOFA评分(分) | 衰弱评分(分) | 死亡人数[例(%)] |
|---|---|---|---|---|
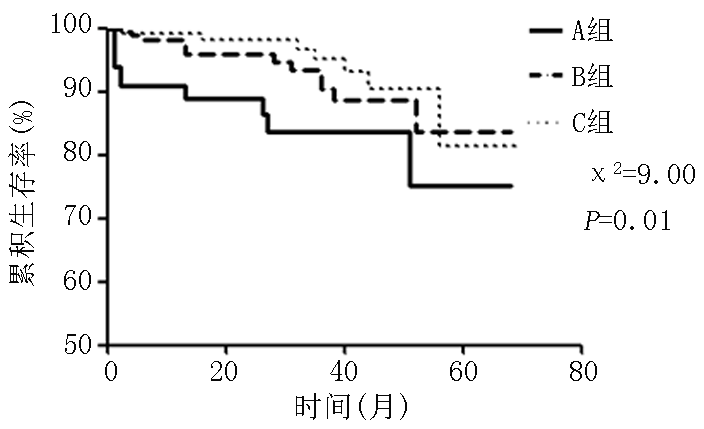
| A组 | 24.00(23.19,25.88) | 18.00(17.51,18.96) | 9.00(8.1,9.12) | 11(0.16) |
| B组 | 16.00(14.56,15.91)* | 13.00(12.31,13.59)* | 5.00(4.78,5.44)* | 12(0.07)* |
| C组 | 7.00(6.79,7.56)*# | 7.00(6.20,6.91)*# | 1.50(1.62,2.15)*# | 8(0.06)*# |
| 统计值 | H=449.401 | H=282.378 | H=9.392 | χ2=9.002 |
| P值 | <0.01 | <0.01 | <0.01 | 0.010 |
| 组别 | APACHEⅡ评分(分) | SOFA评分(分) | 衰弱评分(分) | 死亡人数[例(%)] |
|---|---|---|---|---|
| A组 | 24.00(23.19,25.88) | 18.00(17.51,18.96) | 9.00(8.1,9.12) | 11(0.16) |
| B组 | 16.00(14.56,15.91)* | 13.00(12.31,13.59)* | 5.00(4.78,5.44)* | 12(0.07)* |
| C组 | 7.00(6.79,7.56)*# | 7.00(6.20,6.91)*# | 1.50(1.62,2.15)*# | 8(0.06)*# |
| 统计值 | H=449.401 | H=282.378 | H=9.392 | χ2=9.002 |
| P值 | <0.01 | <0.01 | <0.01 | 0.010 |
| 变量 | A组 | B组 | C组 | |||||
|---|---|---|---|---|---|---|---|---|
| r值 | P值 | r值 | P值 | r值 | P值 | |||
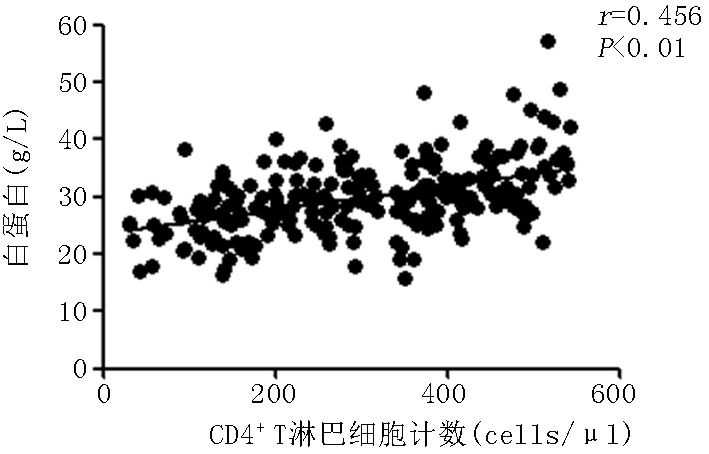
| ALB | 0.261 | <0.01 | 0.322 | <0.01 | 0.059 | 0.491 | ||
| PAB | 0.123 | 0.409 | 0.148 | 0.073 | 0.144 | 0.128 | ||
| TP | 0.435 | <0.01 | 0.114 | 0.169 | 0.101 | 0.286 | ||
| T淋巴细胞计数 | 0.211 | 0.089 | 0.328 | <0.01 | 0.309 | <0.01 | ||
| SCr | 0.145 | 0.274 | -0.019 | 0.766 | 0.011 | 0.968 | ||
| TC | 0.033 | 0.852 | -0.003 | 0.989 | 0.205 | 0.031 | ||
| LDL-C | -0.036 | 0.810 | -0.137 | 0.112 | 0.224 | 0.015 | ||
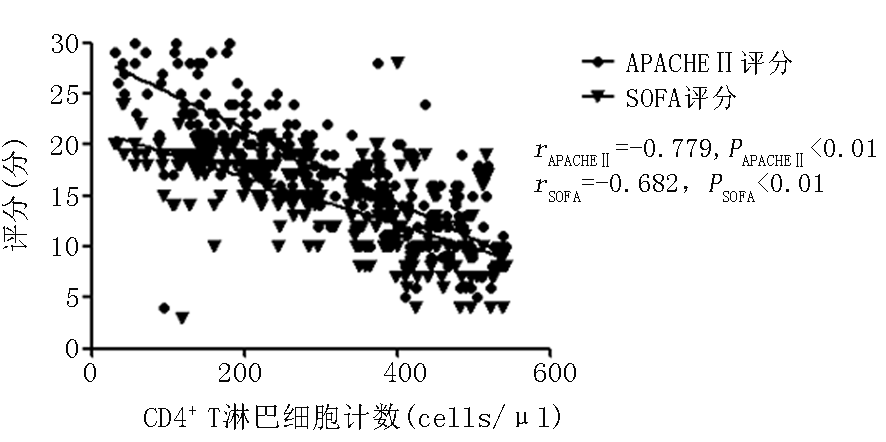
| APACHEⅡ评分 | -0.372 | <0.01 | -0.680 | <0.01 | -0.207 | 0.154 | ||
| SOFA评分 | -0.255 | 0.038 | -0.609 | <0.01 | 0.018 | 0.090 | ||
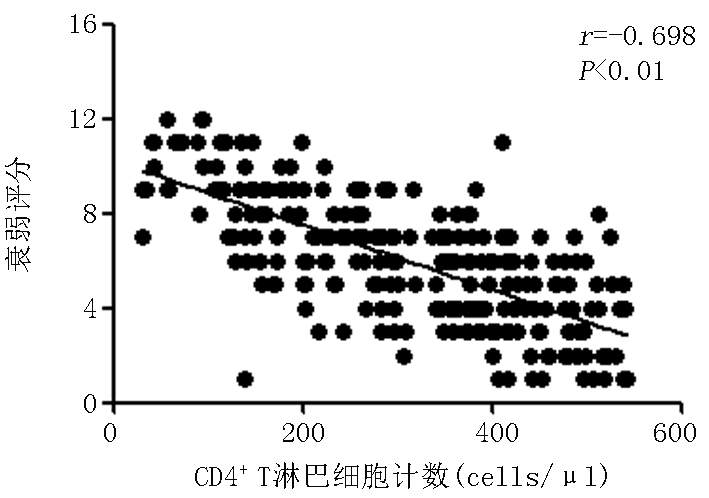
| 衰弱评分 | -0.409 | 0.010 | -0.521 | <0.01 | -0.206 | 0.024 | ||
| 变量 | A组 | B组 | C组 | |||||
|---|---|---|---|---|---|---|---|---|
| r值 | P值 | r值 | P值 | r值 | P值 | |||
| ALB | 0.261 | <0.01 | 0.322 | <0.01 | 0.059 | 0.491 | ||
| PAB | 0.123 | 0.409 | 0.148 | 0.073 | 0.144 | 0.128 | ||
| TP | 0.435 | <0.01 | 0.114 | 0.169 | 0.101 | 0.286 | ||
| T淋巴细胞计数 | 0.211 | 0.089 | 0.328 | <0.01 | 0.309 | <0.01 | ||
| SCr | 0.145 | 0.274 | -0.019 | 0.766 | 0.011 | 0.968 | ||
| TC | 0.033 | 0.852 | -0.003 | 0.989 | 0.205 | 0.031 | ||
| LDL-C | -0.036 | 0.810 | -0.137 | 0.112 | 0.224 | 0.015 | ||
| APACHEⅡ评分 | -0.372 | <0.01 | -0.680 | <0.01 | -0.207 | 0.154 | ||
| SOFA评分 | -0.255 | 0.038 | -0.609 | <0.01 | 0.018 | 0.090 | ||
| 衰弱评分 | -0.409 | 0.010 | -0.521 | <0.01 | -0.206 | 0.024 | ||
| [1] | 何爱萍, 何海玉. 慢性肾功能衰竭的营养与饮食[J]. 医学理论与实践, 2005, 18(2):128-130. |
| [2] | 徐雪峰, 张攀科. 百令胶囊对腹膜透析患者残余肾功能影响的临床观察[J]. 中国医药科学, 2012, 2(9):104-106. |
| [3] |
Vaziri ND. Oxidative stress in uremia: Nature, mechanisms, and potential consequences[J]. Semin Nephrol, 2004, 24(5):469-473.
doi: 10.1016/j.semnephrol.2004.06.026 URL |
| [4] |
Pecoits-Filho R, Heimbürger O, Bárány P, et al. Associations between circulating inflammatory markers and residual renal function in CRF patients[J]. Am J Kidney Dis, 2003, 41(6):1212-1218.
pmid: 12776273 |
| [5] |
Locatelli F, Canaud B, Eckardt KU, et al. Oxidative stress in end-stage renal disease: An emerging threat to patient outcome[J]. Nephrol Dial Transplant, 2003, 18(7):1272-1280.
doi: 10.1093/ndt/gfg074 URL |
| [6] | Girndt M, Sester M, Sester U, et al. Molecular aspects of T- and B-cell function in uremia[J]. Kidney Int Suppl, 2001, 78:S206-S211. |
| [7] | 解德琼, 甘华, 杜晓刚, 等. 不同透析膜对维持性血液透析患者外周血T细胞凋亡的影响[J]. 中华肾脏病杂志, 2006,(12):738-742. |
| [8] | 龚英峰, 李顺利, 杜勇, 等. 尿毒症患者免疫功能与营养状态的相关性分析[J]. 检验医学与临床, 2015, 12(8):1042-1044. |
| [9] | 郝秋奎, 李峻, 董碧蓉, 等. 老年患者衰弱评估与干预中国专家共识[J]. 中华老年医学杂志, 2017, 36(3):251-256. |
| [10] |
Ferrucci L, Cavazzini C, Corsi A, et al. Biomarkers of frailty in older persons[J]. J Endocrinol Invest, 2002, 25(10 Suppl):10-15.
pmid: 12508906 |
| [11] |
Clegg A, Young J, Iliffe S, et al. Frailty in elderly people[J]. Lancet, 2013, 381(9868):752-762.
doi: 10.1016/S0140-6736(12)62167-9 URL |
| [12] |
Sullivan DH, Walls RC. Impact of nutritional status on morbidity in a population of geriatric rehabilitation patients[J]. J Am Geriatr Soc, 1994, 42(5):471-477.
pmid: 8176139 |
| [13] |
Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation[J]. J Am Geriatr Soc, 2010, 58(4):681-687.
doi: 10.1111/j.1532-5415.2010.02764.x URL |
| [14] | 于芹, 邢广群, 周泉. 中性粒细胞细胞外网络与接触系统在尿毒症急性冠状动脉综合征中的作用[J]. 临床荟萃, 2015, 30(5):540-544. |
| [15] | 龚非力. 医学免疫学[M]. 北京: 科学出版社, 2007. |
| [16] | Girndt M, Sester M, Sester U, et al. Molecular aspects of T- and B-cell function in uremia[J]. Kidney Int Suppl, 2001, 78:S206-S211. |
| [17] | Rolfson DB, Majumdar SR, Tsuyuki RT, et al. Validity and reliability of the Edmonton Frail Scale[J]. Age Ageing, 2006, 36(5):526-529. |
| [18] |
Ritzel K, Reincke M, Nitschmann S. Corticoids in patients with septic shock: Adjunctive glucocorticoid therapy in patients with septic shock (ADRENAL) trial and hydrocortisone plus fludrocortisone for adults with septic shock (APROCCHSS)[J]. Internist (Berl), 2018, 59(8):868-870.
doi: 10.1007/s00108-018-0450-1 pmid: 29947850 |
| [19] |
Zhang XM, Zhang WW, Yu XZ, et al. Comparing the performance of SOFA, TPA combined with SOFA and APACHE-II for predicting ICU mortality in critically ill surgical patients: A secondary analysis[J]. Clin Nutr, 2020, 39(9):2902-2909.
doi: 10.1016/j.clnu.2019.12.026 URL |
| [20] |
Visekruna A, Hartmann S, Sillke YR, et al. Intestinal development and homeostasis require activation and apoptosis of diet-reactive T cells[J]. J Clin Invest, 2019, 129(5):1972-1983.
doi: 10.1172/JCI98929 |
| [21] | 梅长林, 余学清. 内科学:肾脏内科分册[M]. 北京: 人民卫生出版社, 2015. |
| [22] | López Plaza B, Bermejo López LM. Nutrition and immune system disorders[J]. Nutr Hosp, 2017, 34(Suppl 4):68-71. |
| [23] | Pae M, Meydani SN, Wu D. The role of nutrition in enhancing immunity in aging[J]. Aging Dis, 2012, 3(1):91-129. |
| [24] |
Wu D, Lewis ED, Pae M, et al. Nutritional modulation of immune function: Analysis of evidence, mechanisms, and clinical relevance[J]. Front Immunol, 2019, 9:3160.
doi: 10.3389/fimmu.2018.03160 URL |
| [25] |
Goldszmid RS, Dzutsev A, Trinchieri G. Host immune response to infection and cancer: Unexpected commonalities[J]. Cell Host Microbe, 2014, 15(3):295-305.
doi: 10.1016/j.chom.2014.02.003 pmid: 24629336 |
| [26] |
Calder PC. Immunological parameters: What do they mean?[J]. J Nutr, 2007, 137(3 Suppl 2):773S-780S.
doi: 10.1093/jn/137.3.773S URL |
| [27] |
Batatinha H, Biondo LA, Lira FS, et al. Nutrients, immune system, and exercise: Where will it take us?[J]. Nutrition, 2019, 61:151-156.
doi: S0899-9007(18)30644-0 pmid: 30711864 |
| [1] | Zhang Jinjin, Jin Ruixia, Sun Wei. High-flux hemodialysis in the frailty of elderly patients with end-stage renal disease [J]. Clinical Focus, 2021, 36(4): 328-331. |
| [2] | Yao Can, Wang Rongzhen, Liu Tianxi. Correlation between level of serum klotho protein, FGF23 and nutritional status of peritoneal dialysis patients [J]. Clinical Focus, 2020, 35(10): 922-926. |
| [3] | Wang Lua, Tian Ronga, Zhou Weia, Niu Jianruia, Gao Maolongb. Effect of frailty on rehospitalization for acute exacerbations of COPD [J]. Clinical Focus, 2019, 34(4): 321-325. |
| [4] | He Huan1, 2, Zhi Min3, 4. Inflammatory bowel diseases and nutritional therapy [J]. Clinical Focus, 2018, 33(8): 666-669. |
| [5] | Tian Yu, Li Junxia, Wang Huahong. Nutritionalrelated diseases of inflammatory bowel disease [J]. Clinical Focus, 2018, 33(8): 656-660. |
| [6] | Wang Zekai, Hu Zhijuan, Dong Chunxia, Niu Kai, Liu Bing. Serum ghrelin and chronic kidney diseases [J]. Clinical Focus, 2018, 33(10): 849-853. |
| [7] | Kong Jianhua, Zhang Jie, Cui Yunjing, Hua Yingying. Comparison of two methods of nutritional assessment in elderly patients with diabetic nephropathy [J]. Clinical Focus, 2017, 32(4): 301-304. |
| [8] | . Nutritional risk screening and support therapy in elderly patients with pulmonary infection [J]. Clinical Focus, 2015, 30(7): 777-780. |
| [9] | He Lianyi. Application effect of different dialysis frequencies in uremic patients [J]. Clinical Focus, 2015, 30(11): 1292-1.29513e+007. |
| [10] | Yuan Xiaorong;Wang Yalan;Meng Lingru;Yu Huanxin;Yang Xuejie;Xu Xiuju. Analysis of nutritional status pre-and post-chemotherapy in patients with digestive carcinoma [J]. Clinical Focus, 2015, 30(11): 1261-1.26413e+007. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||