Clinical Focus ›› 2024, Vol. 39 ›› Issue (3): 239-243.doi: 10.3969/j.issn.1004-583X.2024.03.007
Previous Articles Next Articles
Clinical analysis of 11 cases of coronavirus disease-19 associated with acute pancreatitis: Case report
Wei Fang1, Zhang Yu2, Wang Qingqing1, Zheng Guoqi1( )
)
- 1. Department of Gastroenterology, Cangzhou Central Hospital, Cangzhou 061001, China
2. Department of Gastroenterology, Hejian Hospital of Traditional Chinese Medicine, Cangzhou 062450, China
-
Received:2023-12-29Online:2024-03-20Published:2024-06-12 -
Contact:Zheng Guoqi E-mail:xhkzgq@sina.com
CLC Number:
Cite this article
Wei Fang, Zhang Yu, Wang Qingqing, Zheng Guoqi. Clinical analysis of 11 cases of coronavirus disease-19 associated with acute pancreatitis: Case report[J]. Clinical Focus, 2024, 39(3): 239-243.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.03.007
| 病例 序号 | 性别 | 年龄 (岁) | 甘油三酯 (mmol/L) | 血淀粉酶 (U/L) | 血脂肪酶 (U/L) | C反应蛋白 (mg/L) | 往病史 | 主要治疗 |
|---|---|---|---|---|---|---|---|---|
| 1 | 男 | 29 | 2.57 | 58 | 27 | 21.7 | 无 | 抑酸、抑制胰腺分泌 |
| 2 | 女 | 79 | 0.84 | 320 | 80 | 75.6 | 高血压,甲状腺术后 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 3 | 女 | 43 | 2.43 | 38 | 54 | 26.08 | 2型糖尿病 | 抑酸、控糖、抑制胰腺分泌 |
| 4 | 男 | 40 | 4.2 | 139 | 109 | 21.7 | 无 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 5 | 男 | 38 | 0.72 | 708 | 196 | 未查 | 无 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 6 | 男 | 39 | 3.57 | 475 | 132 | 未查 | 既往甘油三酯2.78 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 7 | 男 | 48 | 2.82 | 489 | 未查 | 未查 | 2型糖尿病 | 抑酸、控糖、抑制胰腺分泌 |
| 8 | 男 | 52 | 2.63 | 851 | 未查 | 147 | 2型糖尿病 | 抑酸、控糖、抑制胰腺分泌、抑制胰酶活性 |
| 9 | 男 | 40 | 3.73 | 63 | 68 | 未查 | 无 | 抑酸、抑制胰腺分泌 |
| 10 | 女 | 37 | 2.43 | 66 | 56 | 230 | 无 | 抑酸、抑制胰腺分泌 |
| 11 | 男 | 63 | 0.69 | 60 | 未查 | 129 | 胆囊息肉切除术 | 抑酸、抑制胰腺分泌 |
Tab.1 Basic information of 11 COVID-19 patients with acute pancreatitis
| 病例 序号 | 性别 | 年龄 (岁) | 甘油三酯 (mmol/L) | 血淀粉酶 (U/L) | 血脂肪酶 (U/L) | C反应蛋白 (mg/L) | 往病史 | 主要治疗 |
|---|---|---|---|---|---|---|---|---|
| 1 | 男 | 29 | 2.57 | 58 | 27 | 21.7 | 无 | 抑酸、抑制胰腺分泌 |
| 2 | 女 | 79 | 0.84 | 320 | 80 | 75.6 | 高血压,甲状腺术后 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 3 | 女 | 43 | 2.43 | 38 | 54 | 26.08 | 2型糖尿病 | 抑酸、控糖、抑制胰腺分泌 |
| 4 | 男 | 40 | 4.2 | 139 | 109 | 21.7 | 无 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 5 | 男 | 38 | 0.72 | 708 | 196 | 未查 | 无 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 6 | 男 | 39 | 3.57 | 475 | 132 | 未查 | 既往甘油三酯2.78 | 抑酸、抑制胰腺分泌、抑制胰酶活性 |
| 7 | 男 | 48 | 2.82 | 489 | 未查 | 未查 | 2型糖尿病 | 抑酸、控糖、抑制胰腺分泌 |
| 8 | 男 | 52 | 2.63 | 851 | 未查 | 147 | 2型糖尿病 | 抑酸、控糖、抑制胰腺分泌、抑制胰酶活性 |
| 9 | 男 | 40 | 3.73 | 63 | 68 | 未查 | 无 | 抑酸、抑制胰腺分泌 |
| 10 | 女 | 37 | 2.43 | 66 | 56 | 230 | 无 | 抑酸、抑制胰腺分泌 |
| 11 | 男 | 63 | 0.69 | 60 | 未查 | 129 | 胆囊息肉切除术 | 抑酸、抑制胰腺分泌 |
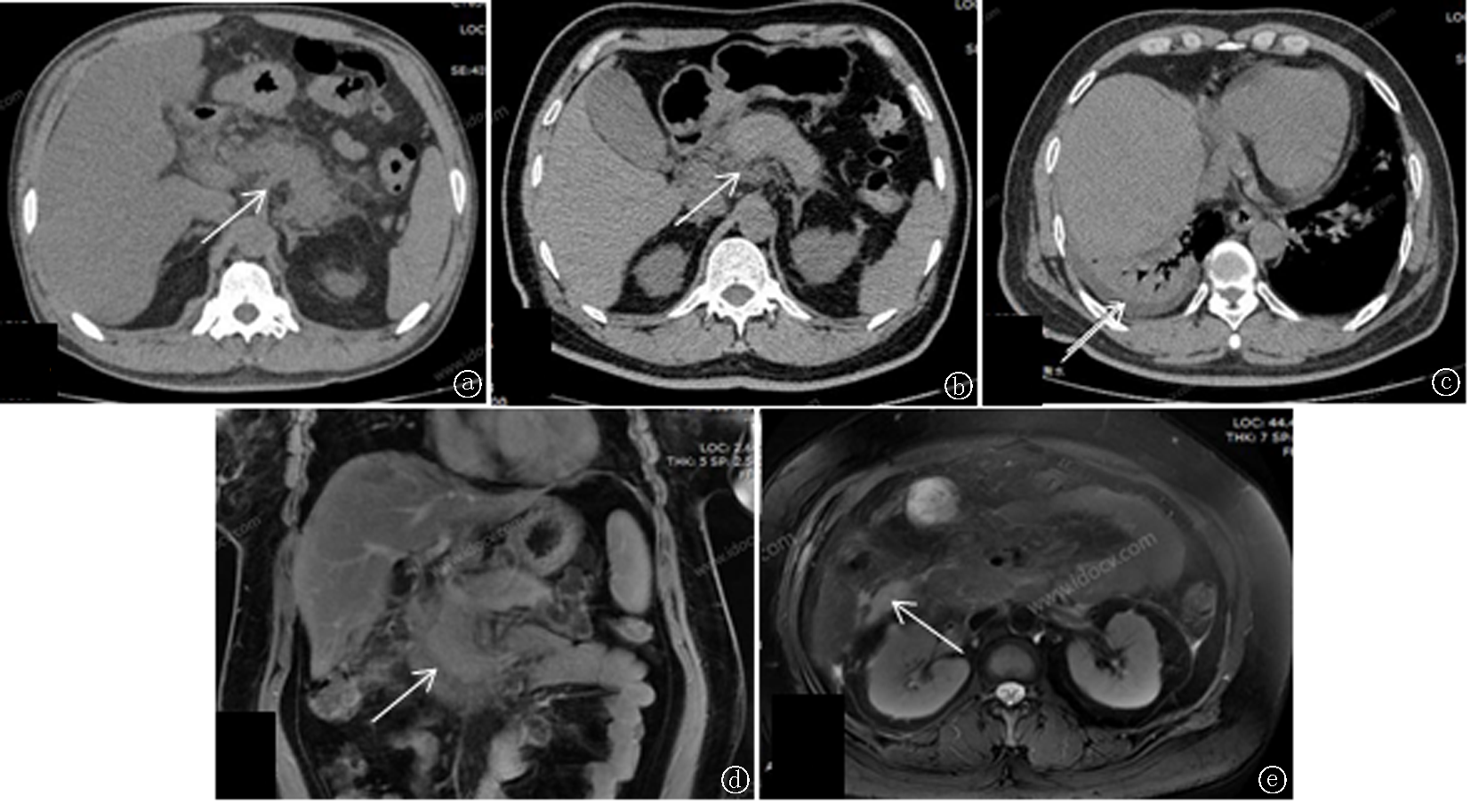
Fig.1 Imaging findings of 11 COVID-19 patients with acute pancreatitis a. CT shows pancreatic swelling with surrounding exudation; b. CT shows pancreatic swelling with visible exudation around it; c. A small amount of pleural effusion; d. MRI coronal plane, showing pancreatic swelling and exudation; e. MRI transverse section, showing encapsulated effusion around the pancreas
| [1] | Kandasamy S. An unusual presentation of COVID-19:Acute pancreatitis[J]. Ann Hepatobiliary Pancreat Surg, 2020, 24(4):539-541. |
| [2] | 李永春, 刘浏, 陈焰. 危重型新型冠状病毒肺炎并发急性胰腺炎1例并文献复习[J]. 现代消化及介入诊疗, 2020, 25(7):985-987. |
| [3] | Dalan R, Bornstein SR, El-Armouche A, et al. The ACE-2 in COVID-19:Foe or Friend?[J]. Horm Metab Res, 2020, 52 (5):257-263. |
| [4] |
熊号峰, 谭建波, 向攀, 等. 危重型新型冠状病毒肺炎合并急性胰腺炎1例并文献复习[J]. 首都医科大学学报, 2021, 42(4):681-683.
doi: 10.3969/j.issn.1006-7795.2021.04.028 |
| [5] | 张韬, 朱帅, 黄耿文. 新型冠状病毒相关性急性胰腺炎的认识现状[J]. 中国普通外科杂志, 2021, 30(9):1017-1022. |
| [6] | 中华人民共和国国家卫生健康委员会. 新型冠状病毒感染诊疗方案(试行第十版)[J]. 中华临床感染病杂志, 2023, 16(1):1-9. |
| [7] | 中华医学会外科学分会胰腺外科学组. 中国急性胰腺炎诊治指南(2021)[J]. 中华消化外科杂志, 2021, 20(7):730-739. |
| [8] | 陈丽萍, 李微霞, 田成, 等. 冠状病毒感染患者消化系统表现的研究进展[J]. 中华消化杂志, 2020, 40(2):80-82. |
| [9] |
Hadi A, Werge M, Kristiansen KT, et al. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members[J]. Pancreatology, 2020, 20(4):665-667.
doi: S1424-3903(20)30147-2 pmid: 32387082 |
| [10] | 中华医学会急诊分会,京津冀急诊急救联盟, 北京医学会急诊分会, 北京医师协会急救医师专科分会, 中国医药卫生文化协会急诊急救分会. 急性胰腺炎急诊诊断及治疗专家共识[J]. 临床肝胆病杂志, 2021, 37(5):1034-1041. |
| [11] | Miao Y, Lidove O, Mauhin W. First case of acute pancreatitis related to SARS-CoV-2 infection[J]. Brit J Surg, 2020, 107 (8):e270. |
| [12] | Kataria S, Sharif A, Rehman A, et al. COVID-19 induced acute pancreatitis:A case report and literature review[J]. Cureus, 2020, 12(7):e9169. |
| [13] | Akarsu C, Karabulut M, Aydin H, et al. Association between acute pancreatitis and COVID-19: Could pancreatitis be the missing piece of the puzzle about increased mortality rates[J]. J Investigat Surg, 2022, 35(1):119-125. |
| [14] |
Wang F, Wang H, Fan J, et al. Pancreatic injury patterns in patients with coronavirus disease 19 pneumonia[J]. Gastroenterology, 2020, 159(1):367-370.
doi: S0016-5085(20)30409-1 pmid: 32247022 |
| [15] | de-Madaria E, Siau K, Cárdenas-Jaén K. Increased amylase and lipase in patients with COVID-19 pneumonia: Don't blame the pancreas just yet[J]! Gastroenterology, 2021, 160(5): 1871. |
| [16] | Yang JK, Lin SS, Ji XJ, et al. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes[J]. Acta Diabetol, 2010, 47(3): 193-199. |
| [17] | Wang KG, Luo JF, Tan F, et al. Acute pancreatitis as the initial manifestation in 2 cases of COVID-19 in Wuhan,China[J]. Open Forum Infect Dis, 2020, 7(9): ofaa324. |
| [18] |
McNabb-Baltar J, Jin DX, Grover AS, et al. Lipase elevation in patients with COVID-19[J]. Am J Gastroenterol, 2020, 115(8):1286-1288.
doi: 10.14309/ajg.0000000000000732 pmid: 32496339 |
| [19] |
Goyal H, Sachdeva S, Perisetti A, et al. Hyperlipasemia and potential pancreatic injury patterns in COVID-19: A marker of severity or innocent bystander?[J]. Gastroenterology, 2021, 160(3):946-948.e2
doi: 10.1053/j.gastro.2020.10.037 pmid: 33129845 |
| [20] | 方丹, 马敬东, 官佳轮, 等. 武汉地区新型冠状病毒肺炎住院患者消化系统表现的单中心描述性研究[J]. 中华消化杂志, 2020, 40(3):151-156. |
| [21] |
Han C, Duan C, Zhang S, et al. Digestive symptoms in COVID-19 patients with mild disease severity: Clinical presentation, stool viral RNA testing, and outcomes[J]. Am J Gastroenterol, 2020, 115(6):916-923.
doi: 10.14309/ajg.0000000000000664 pmid: 32301761 |
| [22] | Guan WI, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China[J]. N Engl J Med, 382(18):1708-1720. |
| [23] | 胡颖, 陆观珠, 许洁. 新型冠状病毒感染引起消化道症状的探讨[J]. 中华传染病杂志, 2020, 38(4):258-260. |
| [24] |
Zuo T, Zhang F, Lui GCY, et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization[J]. Gastroenterology, 2020, 159(3):944-955. e8.
doi: S0016-5085(20)34701-6 pmid: 32442562 |
| [25] | Van der Lelie D, Taghavi S. COVID-19 and the gut microbiome: More than a gut feeling[J]. mSystems, 2020, 5(4):e00453-20. |
| [26] |
Villapol S. Gastrointestinal symptoms associated with COVID-19: Impact on the gut microbiome[J]. Transl Res, 2020, 226:57-69.
doi: 10.1016/j.trsl.2020.08.004 pmid: 32827705 |
| [27] | Kariyawasam JC, Jayarajah U, Riza R, et al. Gastrointestinal manifestations in COVID-19[J]. Trans R Soc Trop Med Hyg, 2021, 115(12):1362-1388. |
| [28] | Chandra R, Lazar NJ, Goldman S, et al. Novel coronavirus (COVID-19) infection-attributed acute pancreatitis: A case report and literature review[J]. Cureus, 2021, 13(6):e15725. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||