Clinical Focus ›› 2023, Vol. 38 ›› Issue (9): 813-818.doi: 10.3969/j.issn.1004-583X.2023.09.007
Previous Articles Next Articles
Analysis of the follow-up results of 163 patients with acute promyelocytic leukemia
Dong Zhengrong, Tao Qianshan, Shen Yuanyuan, Dong Yi( )
)
- Department of Hematology,the Second Hospital of Anhui Medical University,Hefei 230601,China
-
Received:2023-06-01Online:2023-09-20Published:2023-11-21 -
Contact:Dong Yi,Email:dongyixx@126.com
CLC Number:
Cite this article
Dong Zhengrong, Tao Qianshan, Shen Yuanyuan, Dong Yi. Analysis of the follow-up results of 163 patients with acute promyelocytic leukemia[J]. Clinical Focus, 2023, 38(9): 813-818.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2023.09.007
| 临床特征 | 数值 |
|---|---|
| 年龄(岁) | 35(2~84) |
| 性别[例(%)] | |
| 男 | 75(46.0) |
| 女 | 88(54.0) |
| 风险分层[例(%)] | |
| 低危 | 38(23.3) |
| 中危 | 74(45.4) |
| 高危 | 51(31.3) |
| 早期死亡[例(%)] | 14(8.6) |
| FLT3突变[例(%)] | |
| 有 | 19(11.7) |
| 无 | 144(88.3) |
| ACA[例(%)] | |
| 有 | 23(14.1) |
| 无 | 140(85.9) |
| 联合化疗[例(%)] | |
| 是 | 78(47.9) |
| 否 | 85(52.1) |
Tab. 1 Clinical characteristics of the patients
| 临床特征 | 数值 |
|---|---|
| 年龄(岁) | 35(2~84) |
| 性别[例(%)] | |
| 男 | 75(46.0) |
| 女 | 88(54.0) |
| 风险分层[例(%)] | |
| 低危 | 38(23.3) |
| 中危 | 74(45.4) |
| 高危 | 51(31.3) |
| 早期死亡[例(%)] | 14(8.6) |
| FLT3突变[例(%)] | |
| 有 | 19(11.7) |
| 无 | 144(88.3) |
| ACA[例(%)] | |
| 有 | 23(14.1) |
| 无 | 140(85.9) |
| 联合化疗[例(%)] | |
| 是 | 78(47.9) |
| 否 | 85(52.1) |
| 因素 | 早期死亡( | 非早期死亡( | 统计值 | |
|---|---|---|---|---|
| 年龄(岁) | 61(27~84) | 33(2~80) | <0.01 | 30.856 |
| 性别[例(%)] | ||||
| 男 女 | 4(30.8) 9(69.2) | 71(47.3) 79(52.7) | 0.250 | 1.321 |
| 血红蛋白(g/L) | 75(35~117) | 80(32~143) | 0.857 | 0.181 |
| WBC(×109/L) | 21(0.53~116.94) | 2.9(0.23~122) | 0.004 | 2.855 |
| PLT(×109/L) | 15(5~41) | 20.5(1~134) | 0.192 | 1.305 |
| 纤维蛋白(mg/dl) | 0.85(0.52~5.68) | 1.23(0.20~5.47) | 0.128 | 1.522 |
| PT(s) | 15.9(11.4~30.8) | 13.15(9.6~19.8) | 0.086 | 1.719 |
| APTT(s) | 28.2(22.1~57.6) | 27.85(16.5~48) | 0.360 | 0.916 |
| 危险分层[例(%)] | ||||
| 低危 | 0(0) | 38(25.3) | ||
| 中危 | 3(23.1) | 71(47.3) | 0.001 | 14.246 |
| 高危 | 10(76.9) | 41(27.3) | ||
| ACA[例(%)] | ||||
| 有 无 | 0(0) 13(100) | 23(14.1) 127(85.9) | 0.268 | 1.228 |
| FLT3突变[例(%)] | ||||
| 有 无 | 2(15.4) 11(84.6) | 17(11.3) 133(88.7) | 0.663 | 0.435 |
Tab. 2 Clinical characteristics of early death patients
| 因素 | 早期死亡( | 非早期死亡( | 统计值 | |
|---|---|---|---|---|
| 年龄(岁) | 61(27~84) | 33(2~80) | <0.01 | 30.856 |
| 性别[例(%)] | ||||
| 男 女 | 4(30.8) 9(69.2) | 71(47.3) 79(52.7) | 0.250 | 1.321 |
| 血红蛋白(g/L) | 75(35~117) | 80(32~143) | 0.857 | 0.181 |
| WBC(×109/L) | 21(0.53~116.94) | 2.9(0.23~122) | 0.004 | 2.855 |
| PLT(×109/L) | 15(5~41) | 20.5(1~134) | 0.192 | 1.305 |
| 纤维蛋白(mg/dl) | 0.85(0.52~5.68) | 1.23(0.20~5.47) | 0.128 | 1.522 |
| PT(s) | 15.9(11.4~30.8) | 13.15(9.6~19.8) | 0.086 | 1.719 |
| APTT(s) | 28.2(22.1~57.6) | 27.85(16.5~48) | 0.360 | 0.916 |
| 危险分层[例(%)] | ||||
| 低危 | 0(0) | 38(25.3) | ||
| 中危 | 3(23.1) | 71(47.3) | 0.001 | 14.246 |
| 高危 | 10(76.9) | 41(27.3) | ||
| ACA[例(%)] | ||||
| 有 无 | 0(0) 13(100) | 23(14.1) 127(85.9) | 0.268 | 1.228 |
| FLT3突变[例(%)] | ||||
| 有 无 | 2(15.4) 11(84.6) | 17(11.3) 133(88.7) | 0.663 | 0.435 |
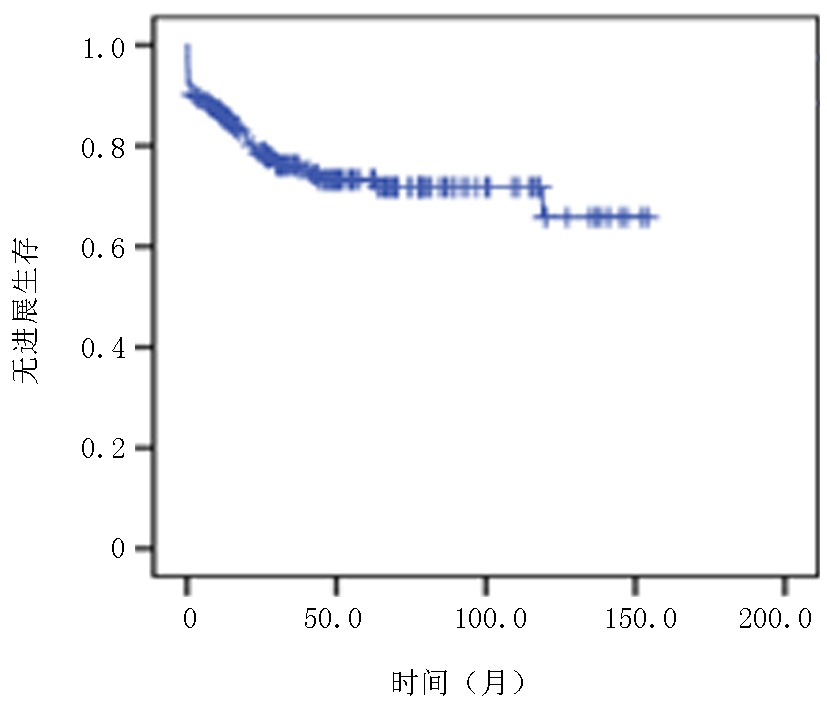
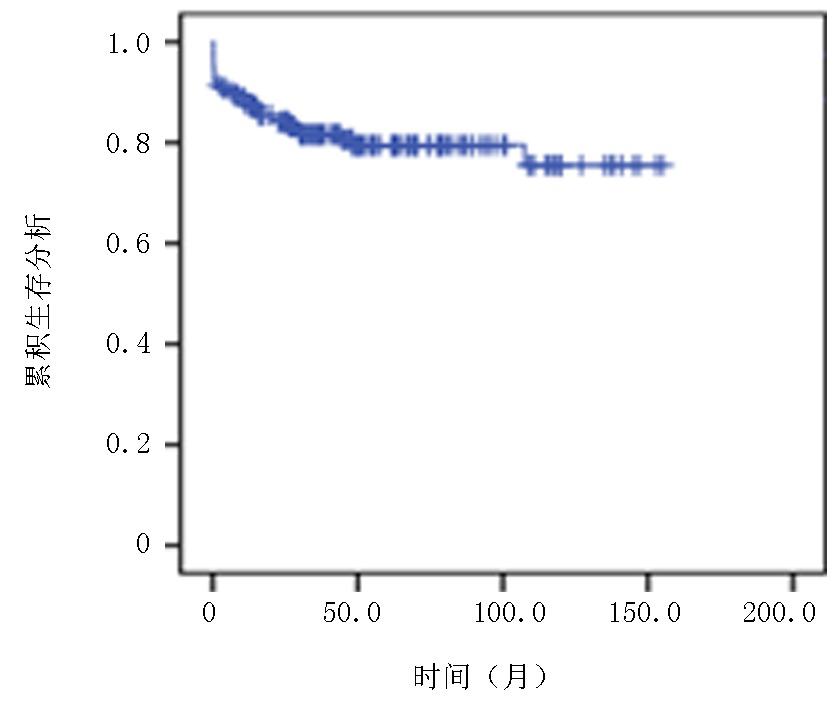
| 因素 | 例(%) | PFS | OS | |||
|---|---|---|---|---|---|---|
| χ2值 | χ2值 | |||||
| 年龄 | ||||||
| ≤60岁 >60岁 | 149(91.4) 14(8.6) | 28.289 | <0.01 | 29.296 | <0.01 | |
| 性别 | ||||||
| 男 女 | 75(46.0) 88(54.0) | 0.001 | 0.972 | 0.002 | 0.962 | |
| ACA | ||||||
| 有 无 | 23(14.1) 140(85.9) | 0.194 | 0.659 | 0.258 | 0.611 | |
| FLT3突变 | ||||||
| 有 无 | 19(11.7) 144(88.3) | 0.587 | 0.444 | 0.392 | 0.531 | |
| 危险分层 | ||||||
| 低危 | 38(23.3) | |||||
| 中危 | 74(45.4) | 2.554 | 0.279 | 2.655 | 0.265 | |
| 高危 | 51(31.3) | |||||
| 治疗方案 | ||||||
| 不联合化疗 联合化疗 | 85(52.1) 78(47.9) | 3.738 | 0.053 | 5.355 | 0.021 | |
Tab. 3 Univariable analysis of PFS and OS in APL patients
| 因素 | 例(%) | PFS | OS | |||
|---|---|---|---|---|---|---|
| χ2值 | χ2值 | |||||
| 年龄 | ||||||
| ≤60岁 >60岁 | 149(91.4) 14(8.6) | 28.289 | <0.01 | 29.296 | <0.01 | |
| 性别 | ||||||
| 男 女 | 75(46.0) 88(54.0) | 0.001 | 0.972 | 0.002 | 0.962 | |
| ACA | ||||||
| 有 无 | 23(14.1) 140(85.9) | 0.194 | 0.659 | 0.258 | 0.611 | |
| FLT3突变 | ||||||
| 有 无 | 19(11.7) 144(88.3) | 0.587 | 0.444 | 0.392 | 0.531 | |
| 危险分层 | ||||||
| 低危 | 38(23.3) | |||||
| 中危 | 74(45.4) | 2.554 | 0.279 | 2.655 | 0.265 | |
| 高危 | 51(31.3) | |||||
| 治疗方案 | ||||||
| 不联合化疗 联合化疗 | 85(52.1) 78(47.9) | 3.738 | 0.053 | 5.355 | 0.021 | |
| [1] |
Kayser S, Levis M J. Clinical implications of molecular markers in acute myeloid leukemia[J]. Eur J Haematol, 2019, 102(1): 20-35.
doi: 10.1111/ejh.13172 pmid: 30203623 |
| [2] |
Stahl M, Tallman M S. Acute promyelocytic leukemia (APL): Remaining challenges towards a cure for all[J]. Leuk Lymphoma, 2019, 60(13): 3107-3115.
doi: 10.1080/10428194.2019.1613540 URL |
| [3] |
Norgaard JM, Friis LS, Kristensen J S, et al. Addressing the room for improvement in management of acute promyelocytic leukemia[J]. Eur J Haematol, 2019, 102(6): 479-485.
doi: 10.1111/ejh.13229 pmid: 30887583 |
| [4] |
Akcay OF, Yeter HH, Buyukasik Y. Real-life outcomes of unselected acute promyelocytic leukemia patients: A single-center 14-year experience[J]. Rom J Intern Med, 2020, 58(3): 138-145.
doi: 10.2478/rjim-2020-0011 pmid: 32452194 |
| [5] | 中华医学会血液学分会, 中国医师协会血液科医师分会.中国急性早幼粒细胞白血病诊疗指南(2018年版)[J]. 中华血液学杂志, 2018, 39(3): 179-183. |
| [6] |
Sanz M, Fenaux P, Tallman M, et al. Management of acute promyelocytic leukemia: Updated recommendations from an expert panel of the European LeukemiaNet[J]. Blood, 2019, 133(15):1630-1643.
doi: 10.1182/blood-2019-01-894980 pmid: 30803991 |
| [7] |
Stahl M, Tallman MS. Differentiation syndrome in acute promyelocytic leukaemia[J]. Br J Haematol, 2019, 187(2):157-162.
doi: 10.1111/bjh.v187.2 URL |
| [8] |
Cicconi L, Platzbecker U, Avvisati G, et al. Longterm results of all-trans retinoic acid and arsenic trioxide in non-high-risk acute promyelocytic leukemia: Update of the APL0406 Italian-German randomized trial[J]. Leukemia, 2020, 34(3):914-918.
doi: 10.1038/s41375-019-0589-3 pmid: 31611624 |
| [9] |
Lancet JE, Moseley AB, Coutre SE, et al. A phase 2 study of ATRA, arsenic trioxide, and gemtuzumab ozogamicin in patients with high-risk APL (SWOG 0535)[J]. Blood Adv, 2020, 4(8):1683-1689.
doi: 10.1182/bloodadvances.2019001278 URL |
| [10] |
Zhang X, Sun J, Yu W, et al. Current views on the genetic landscape and management of variant acute promyelocytic leukemia[J]. Biomark Res, 2021, 9(1):33.
doi: 10.1186/s40364-021-00284-x pmid: 33957999 |
| [11] |
Baysal M, Gursoy V, Hunutlu FC, et al. The evaluation of risk factors leading to early deaths in patients with acute promyelocytic leukemia: A retrospective study[J]. Ann Hematol, 2022, 101(5): 1049-1057.
doi: 10.1007/s00277-022-04798-8 pmid: 35190843 |
| [12] |
Daver N, Schlenk RF, Russell NH. Targeting FLT3 mutations in AML: Review of current knowledge and evidence[J]. Leukemia, 2019, 33(2):299-312.
doi: 10.1038/s41375-018-0357-9 pmid: 30651634 |
| [13] |
Esnault C, Rahme R, Rice K, et al. FLT3-ITD impedes retinoic acid, but not arsenic, responses in murine acute promyelocytic leukemias[J]. Blood, 2019, 133(13): 1495-506.
doi: 10.1182/blood-2018-07-866095 pmid: 30674471 |
| [14] | Deka R, Naseem S, Bhatia P, et al. FLT3-ITD mutation does not influence survival outcome in adult acute promyelocytic leukemia patients treated with ATO and ATRA-based therapeutic regimen: Experience from a north Indian tertiary care centre[J]. Clin Lymph Myeloma Leuk, 2022, 22(6):416-423. |
| [15] |
Teng-Fei S, Diyaer A, Hong-Ming Z, et al. Evolving of treatment paradigms and challenges in acute promyelocytic leukaemia: A real-world analysis of 1105 patients over the last three decades[J]. Transl Oncol, 2022, 25(11):101522.
doi: 10.1016/j.tranon.2022.101522 URL |
| [16] | Thakur W, Anwar N, Fatima N, et al. Coagulation Abnormalities and Risk Assessment in Acute Promyelocytic Leukemia: An experience from a resource-constraint country[J]. Cureus, 2022, 14(6):e26026. |
| [17] |
Chien N, Varghese C, Green TN, et al. Treatment outcomes of patients with acute promyelocytic leukaemia between 2000 and 2017, a retrospective, single centre experience[J]. Leuk Res, 2020, 93(4): 106358.
doi: 10.1016/j.leukres.2020.106358 URL |
| [18] | Nauffal M, Werner L, Ni J, et al. Rate of differentiation syndrome in patients based on timing of initial all-trans retinoic acid administration[J]. Leuk Res Rep, 2019, 12(11): 100189. |
| [19] |
Salman MY, Ofran Y. Early death in acute promyelocytic leukemia: Time to redefine risk groups[J]. Haematologica, 2022, 107(7):1498-1499.
doi: 10.3324/haematol.2021.280446 URL |
| [20] |
Österroos A, Maia T, Eriksson A, et al. A risk score based on real-world data to predict early death in acute promyelocytic leukemia[J]. Haematologica, 2022, 107(7): 1528-1537.
doi: 10.3324/haematol.2021.280093 URL |
| [21] | 沈子园, 康海全, 桑威, 等. 白血病合并感染患者细菌分布、耐药情况及死亡危险因素分析[J]. 临床荟萃, 2021, 36(12):1092-1096. |
| [22] | Vu MP, Nguyen CN, Vu H, et al. Association between FLT3-ITD and additional chromosomal abnormalities in the prognosis of acute promyelocytic leukemia[J]. J Int Med Res, 2022, 50(12):3000605221138490. |
| [23] |
Deka RR, Naseem S, Bhatia P, et al. FLT3-ITD mutation does not influence survival outcome in adult acute promyelocytic leukemia patients treated with ATO and ATRA-based therapeutic regimen: experience from a north indian tertiary care centre[J]. Clin Lymphoma Myeloma Leuk, 2022, 22(6):416-423.
doi: 10.1016/j.clml.2021.12.007 URL |
| [24] | Vu MP, Nguyen CN, Vu H. Cytogenetic influence on prognosis in acute promyelocytic leukaemia: A cohort study in vietnam[J]. Hematol Oncol Stem Cell Ther, 2022, 15(4):151-153. |
| [25] |
Epstein-Peterson ZD, Derkach A, Geyer S. Effect of additional cytogenetic abnormalities on survival in arsenic trioxide-treated acute promyelocytic leukemia[J]. Blood Adv, 2022, 6(11):3433-3439.
doi: 10.1182/bloodadvances.2021006682 URL |
| [26] | 王佳, 董毅, 陶千山, 等. FLT3-ITD突变与附加染色体核型对急性早幼粒细胞白血病患者预后的影响[J]. 西部医学, 2022, 34(10):1477-1480. |
| [27] |
Wang HY, Gong S, Li GH, et al. An effective and chemotherapy-free strategy of all-trans retinoic acid and arsenic trioxide for acute promyelocytic leukemia in all risk groups (APL15 trial)[J]. Blood Cancer J, 2022, 12(11):158.
doi: 10.1038/s41408-022-00753-y |
| [28] |
Ma YF, Lu Y, Wu Q, et al. Oral arsenic and retinoic acid for high-risk acute promyelocytic leukemia[J]. J Hematol Oncol, 2022, 15(1):148.
doi: 10.1186/s13045-022-01368-3 |
| [29] |
Park YH, Kim DY, Mun YC, et al. Long-term follow-up results of cytarabine-containing chemotherapy for acute promyelocytic leukemia[J]. Korean J Intern Med, 2022, 37(4):841-850.
doi: 10.3904/kjim.2021.468 pmid: 35811370 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||