Clinical Focus ›› 2024, Vol. 39 ›› Issue (6): 542-547.doi: 10.3969/j.issn.1004-583X.2024.06.010
Previous Articles Next Articles
Cerebellar ataxia associated with antibodies against GAD65: A case report and literature review
Zhang Li1, Fu Qingxi2a, Su Mingzhao2b, Su Quanping2b( )
)
- 1. Postgraduate Training Base, Linyi People's Hospital, Jinzhou Medical University, Jinzhou 121000, China
2a. Department of Epilepsy and Sleep; b.Central Laboratory, Linyi People's Hospital, Linyi 276000, China
-
Received:2024-02-26Online:2024-06-20Published:2024-07-18 -
Contact:Su Quanping, Email:suquanping@163.com
CLC Number:
Cite this article
Zhang Li, Fu Qingxi, Su Mingzhao, Su Quanping. Cerebellar ataxia associated with antibodies against GAD65: A case report and literature review[J]. Clinical Focus, 2024, 39(6): 542-547.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.06.010
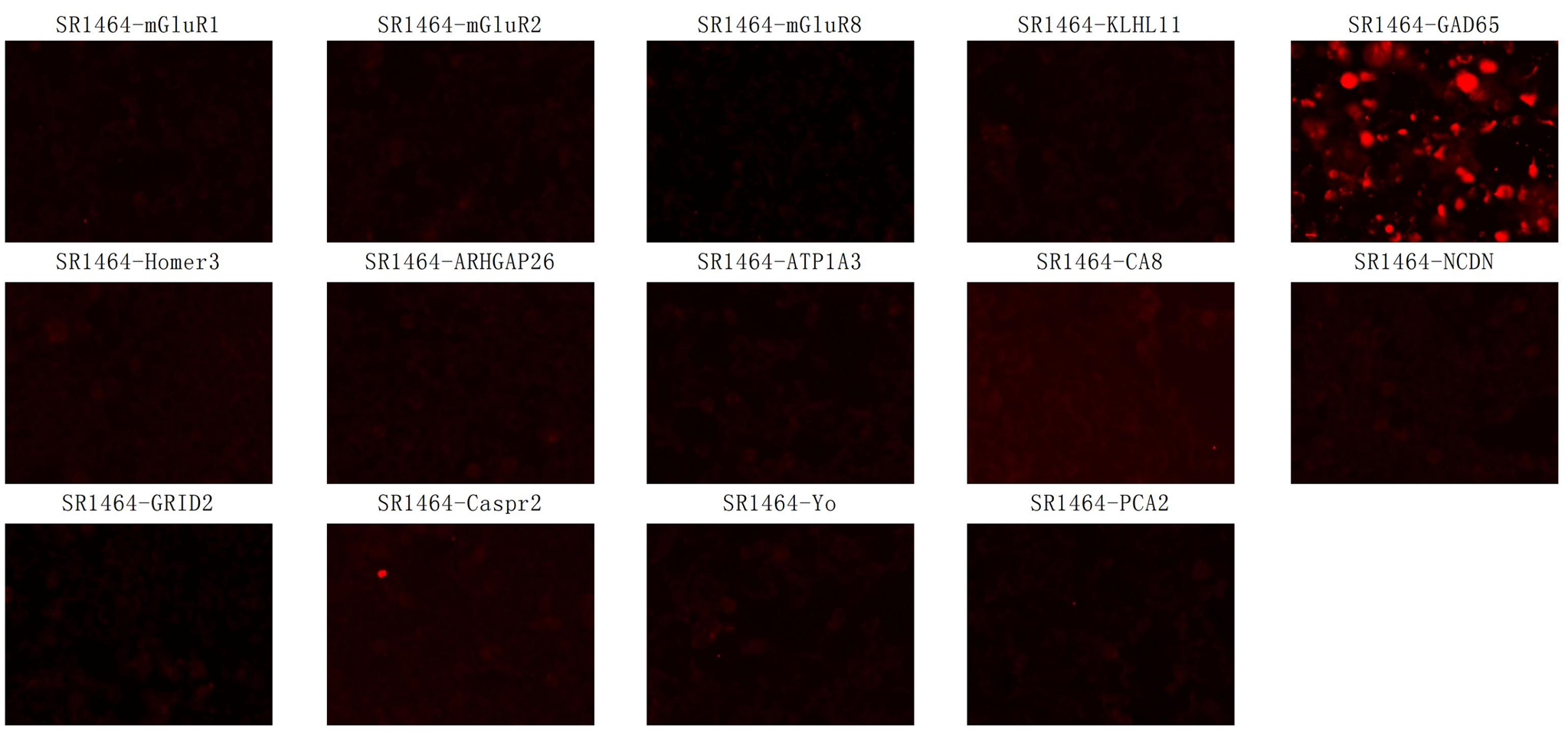
Fig. 1 Red channel detection map of 14 antibodies for autoimmune cerebellar ataxia Serum antibody detection was detected by indirect immunofluorescence using transfected cells, anti- GAD65 antibody positive was seen with significant red fluorescence
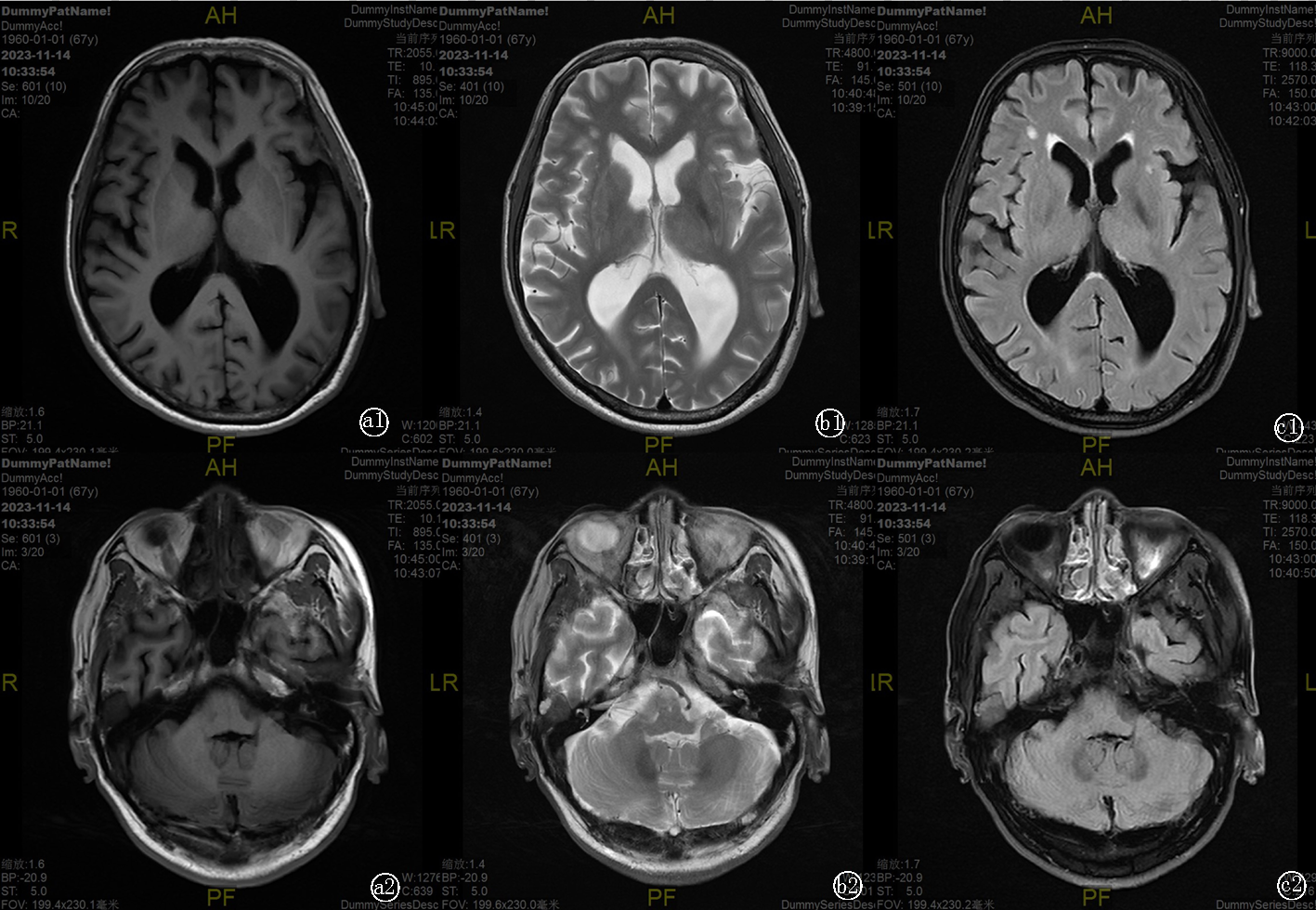
Fig. 2 The patient's head MRI images a. T1-weighted images; b. T2-weighted images; c. T2-weighted fluid-attenuated inversion recovery (FLAIR) brain images; a1, b1, and c1 showed that dilatation of lateral ventricles, widening of cerebral sulci and narrowing of the gyri; a2, b2 and c2 showed insignificant cerebellar atrophy
| 文献 | 性别 | 年龄 (岁) | 病程 (月) | 临床症状 | 体征 | 共病 |
|---|---|---|---|---|---|---|
| 刘峥等[ | 女 | 45 | 42 | 眩晕,视物成双,右侧肢体活动不协调,行走不稳 | 右眼睑下垂,双眼上视受限,下视出现垂直眼震(右>左);右下肢肌力5-级,右侧肢体共济失调,不能直线行走 | 无 |
| 刘静等[ | 女 | 62 | 9 | 头晕,左侧肢体活动不灵,行走不稳 | 双眼左视水平凝视眼震;左侧肢体共济失调,步基宽,吟诗样语言,闭目难立征阳性,双下肢腱反射减退,双滑征阳性 | 自身免疫相关性糖尿病并发周围神经损害 |
| 朱丽平等[ | 男 | 62 | 6 | 复视,构音不清,行走不稳 | 双眼上视受限,各方向复视,构音欠清,双侧肢体共济失调 | 无 |
| 杨桦等[ | 女 | 59 | 3 | 头晕,视物模糊,行走不稳 | 双眼水平旋转粗大眼震,小脑步态,双下肢共济失调,闭目难立征阳性,右侧病理征可疑阳性 | 无 |
| 高颖等[ | 女 | 61 | 12 | 视物重影,行走不稳 | 左眼睑下垂,双眼水平眼震;步基宽,不能直线行走,左侧肢体共济失调,右侧霍夫曼征阳性,闭目难立征阳性,右侧Chaddock征阳性 | 无 |
| 任若琳等[ | 女 | 53 | 18 | 双足趾屈曲痉挛疼痛,大汗,气促,行走不稳 | 步基宽,不能直线行走,闭目难立征阳性 | 僵人综合征;亚临床甲状腺功能减退,自身免疫性甲状腺炎 |
| 刘芳芳等[ | 女 | 65 | 12 | 头晕,视物晃动,行走不稳 | 垂直下跳性眼震;不能直线行走,闭目难立征阳性 | 无 |
| 本例 | 男 | 67 | 1.5 | 言语含糊,双下肢无力,不能独立行走 | 构音欠清,双下肢肌力5-级,双下肢腱反射减退,双侧肢体共济失调,不能直线行走,闭目难立征阳性,双侧病理征阳性 | 甲状腺功能减退症 |
Tab. 1 General information and clinical characteristics of cases with GAD65 antibody-associated cerebellar ataxia reported in China
| 文献 | 性别 | 年龄 (岁) | 病程 (月) | 临床症状 | 体征 | 共病 |
|---|---|---|---|---|---|---|
| 刘峥等[ | 女 | 45 | 42 | 眩晕,视物成双,右侧肢体活动不协调,行走不稳 | 右眼睑下垂,双眼上视受限,下视出现垂直眼震(右>左);右下肢肌力5-级,右侧肢体共济失调,不能直线行走 | 无 |
| 刘静等[ | 女 | 62 | 9 | 头晕,左侧肢体活动不灵,行走不稳 | 双眼左视水平凝视眼震;左侧肢体共济失调,步基宽,吟诗样语言,闭目难立征阳性,双下肢腱反射减退,双滑征阳性 | 自身免疫相关性糖尿病并发周围神经损害 |
| 朱丽平等[ | 男 | 62 | 6 | 复视,构音不清,行走不稳 | 双眼上视受限,各方向复视,构音欠清,双侧肢体共济失调 | 无 |
| 杨桦等[ | 女 | 59 | 3 | 头晕,视物模糊,行走不稳 | 双眼水平旋转粗大眼震,小脑步态,双下肢共济失调,闭目难立征阳性,右侧病理征可疑阳性 | 无 |
| 高颖等[ | 女 | 61 | 12 | 视物重影,行走不稳 | 左眼睑下垂,双眼水平眼震;步基宽,不能直线行走,左侧肢体共济失调,右侧霍夫曼征阳性,闭目难立征阳性,右侧Chaddock征阳性 | 无 |
| 任若琳等[ | 女 | 53 | 18 | 双足趾屈曲痉挛疼痛,大汗,气促,行走不稳 | 步基宽,不能直线行走,闭目难立征阳性 | 僵人综合征;亚临床甲状腺功能减退,自身免疫性甲状腺炎 |
| 刘芳芳等[ | 女 | 65 | 12 | 头晕,视物晃动,行走不稳 | 垂直下跳性眼震;不能直线行走,闭目难立征阳性 | 无 |
| 本例 | 男 | 67 | 1.5 | 言语含糊,双下肢无力,不能独立行走 | 构音欠清,双下肢肌力5-级,双下肢腱反射减退,双侧肢体共济失调,不能直线行走,闭目难立征阳性,双侧病理征阳性 | 甲状腺功能减退症 |
| 文献 | GAD65 抗体 | 脑脊液 OCB | 副肿瘤综 合征抗体 | 颅脑MRI | 治疗 | 预后 |
|---|---|---|---|---|---|---|
| 刘峥等[ | 血清1∶100,CSF 1∶100 | 阳性 | 血清SOX1弱阳性 | 右侧小脑蚓部轻度萎缩逐渐加重 | 甲强龙1 g/d×5 d,之后口服泼尼松60 mg/d | 1周后症状均有减轻,但仍有双眼上视受限 |
| 刘静等[ | 血清1∶100,CSF 1:320 | 阳性 | 阴性 | 未见明显异常 | 口服泼尼松1 mg/kg/d,每周减2.5 mg | 病情趋于稳定 |
| 朱丽平等[ | 血清弱阳性,CSF强阳性 | 阳性 | 未查 | 未见明显异常 | 甲强龙1 g/d,每3天减量一半,之后口服泼尼松1 mg/kg | 3 d后症状明显减轻,2周后在搀扶下能行走 |
| 杨桦等[ | 血清1:10,CSF 1:320 | 未查 | 阴性 | 未见明显异常 | 注人免疫球蛋白25 g,每日1次,持续1周 | 1周后能独立站立,1个月后无明显变化 |
| 高颖等[ | 血清和CSF强阳性 | 未查 | 未查 | 未见明显异常 | 甲强龙1 g/d,每3天减量一半,之后口服泼尼松1 mg/kg,口服3周 | 3个月后症状改善,仍有行走不稳 |
| 任若琳等[ | 血清63AU(阳性),脑脊液6AU(灰区) | 阴性 | 阴性 | 未见明显异常 | 甲强龙500 mg×5 d,之后口服泼尼松80 mg,每3天减5 mg,口服45 d | 症状改善,日常生活不受影响 |
| 刘芳芳等[ | 血清1∶100,CSF 1∶100 | 阴性 | 未查 | 未见明显异常 | 静脉滴注丙种球蛋白冲击×5 d,之后口服泼尼松30 mg/d,逐渐减量 | 1个月后头晕好转,ICARS国际共济失调评定量表评分18分降低为12分 |
| 本例 | 血清1∶30 | 未查 | 未查 | 脑萎缩 | 甲强龙500 mg/d,每3天减量一半,之后口服泼尼松并口服60 mg每周减量1片,并口服吗替麦考酚酯长期治疗 | 出院时言语不清好转,出院1个月后症状缓解,但仍走路不稳 |
Tab. 2 Examination results, treatment and prognosis of cases with GAD65 antibody-associated cerebellar ataxia reported in China
| 文献 | GAD65 抗体 | 脑脊液 OCB | 副肿瘤综 合征抗体 | 颅脑MRI | 治疗 | 预后 |
|---|---|---|---|---|---|---|
| 刘峥等[ | 血清1∶100,CSF 1∶100 | 阳性 | 血清SOX1弱阳性 | 右侧小脑蚓部轻度萎缩逐渐加重 | 甲强龙1 g/d×5 d,之后口服泼尼松60 mg/d | 1周后症状均有减轻,但仍有双眼上视受限 |
| 刘静等[ | 血清1∶100,CSF 1:320 | 阳性 | 阴性 | 未见明显异常 | 口服泼尼松1 mg/kg/d,每周减2.5 mg | 病情趋于稳定 |
| 朱丽平等[ | 血清弱阳性,CSF强阳性 | 阳性 | 未查 | 未见明显异常 | 甲强龙1 g/d,每3天减量一半,之后口服泼尼松1 mg/kg | 3 d后症状明显减轻,2周后在搀扶下能行走 |
| 杨桦等[ | 血清1:10,CSF 1:320 | 未查 | 阴性 | 未见明显异常 | 注人免疫球蛋白25 g,每日1次,持续1周 | 1周后能独立站立,1个月后无明显变化 |
| 高颖等[ | 血清和CSF强阳性 | 未查 | 未查 | 未见明显异常 | 甲强龙1 g/d,每3天减量一半,之后口服泼尼松1 mg/kg,口服3周 | 3个月后症状改善,仍有行走不稳 |
| 任若琳等[ | 血清63AU(阳性),脑脊液6AU(灰区) | 阴性 | 阴性 | 未见明显异常 | 甲强龙500 mg×5 d,之后口服泼尼松80 mg,每3天减5 mg,口服45 d | 症状改善,日常生活不受影响 |
| 刘芳芳等[ | 血清1∶100,CSF 1∶100 | 阴性 | 未查 | 未见明显异常 | 静脉滴注丙种球蛋白冲击×5 d,之后口服泼尼松30 mg/d,逐渐减量 | 1个月后头晕好转,ICARS国际共济失调评定量表评分18分降低为12分 |
| 本例 | 血清1∶30 | 未查 | 未查 | 脑萎缩 | 甲强龙500 mg/d,每3天减量一半,之后口服泼尼松并口服60 mg每周减量1片,并口服吗替麦考酚酯长期治疗 | 出院时言语不清好转,出院1个月后症状缓解,但仍走路不稳 |
| 文献 | 病例数 | 平均年龄 (岁) | 女性 [例(%)] | 神经系统症状 | 鞘内合成 GAD65抗体 | 脑脊液 OCB | 共病 |
|---|---|---|---|---|---|---|---|
| Honnorat et al[ | 14 | 51(20~74) | 13(93%) | 步态共济失调(100%),肢体共济失调(86%),眼球震颤(86%),构音障碍(57%) | 5/6(83%) | 10/14(71%) | T1DM(71%),甲状腺炎(57%),恶性贫血(14%),重症肌无力(7%),肿瘤(14%) |
| Saiz et al[ | 17 | 59(39~77) | 16(94%) | 步态共济失调(100%),肢体共济失调(59%),眼球震颤(65%),构音障碍(65%) | 12/12(100%) | 9/13(69%) | T1DM(53%),甲状腺炎(41%),恶性贫血(12%),白癜风(6%),肿瘤(12%) |
| Arino et al[ | 34 | 58(33~80) | 28/34(82%) | 步态共济失调(91%),肢体共济失调(74%),构音障碍(71%),眼球震颤(59%) | 13/15(87%) | 16/22(73%) | T1DM(38%),甲状腺炎(53%),恶性贫血(21%),白癜风(6%),肿瘤(12%) |
| Budhram et al[ | 55 | 59 (14~83) | 42(76%) | 未记录 | 55/55(100%) | 13/31(42%) | 全身性免疫疾病(65%),T1DM (33%),甲状腺疾病(36%),恶性贫血(20%),其他疾病(13%),肿瘤(13%) |
| Bai et al[ | 11 | 54(43~63) | 9(81.8%) | 步态共济失调(100%),头晕或复视(63.6%),构音障碍(63.4%) | 11/11(100%) | 4/6(66.7%) | 相关自身免疫性疾病(36%),脑炎/癫痫(36%),僵人综合征(9%),肿瘤(9%) |
Tab. 3 Summary of cases with GAD65 antibody-associated cerebellar ataxia reported abroad
| 文献 | 病例数 | 平均年龄 (岁) | 女性 [例(%)] | 神经系统症状 | 鞘内合成 GAD65抗体 | 脑脊液 OCB | 共病 |
|---|---|---|---|---|---|---|---|
| Honnorat et al[ | 14 | 51(20~74) | 13(93%) | 步态共济失调(100%),肢体共济失调(86%),眼球震颤(86%),构音障碍(57%) | 5/6(83%) | 10/14(71%) | T1DM(71%),甲状腺炎(57%),恶性贫血(14%),重症肌无力(7%),肿瘤(14%) |
| Saiz et al[ | 17 | 59(39~77) | 16(94%) | 步态共济失调(100%),肢体共济失调(59%),眼球震颤(65%),构音障碍(65%) | 12/12(100%) | 9/13(69%) | T1DM(53%),甲状腺炎(41%),恶性贫血(12%),白癜风(6%),肿瘤(12%) |
| Arino et al[ | 34 | 58(33~80) | 28/34(82%) | 步态共济失调(91%),肢体共济失调(74%),构音障碍(71%),眼球震颤(59%) | 13/15(87%) | 16/22(73%) | T1DM(38%),甲状腺炎(53%),恶性贫血(21%),白癜风(6%),肿瘤(12%) |
| Budhram et al[ | 55 | 59 (14~83) | 42(76%) | 未记录 | 55/55(100%) | 13/31(42%) | 全身性免疫疾病(65%),T1DM (33%),甲状腺疾病(36%),恶性贫血(20%),其他疾病(13%),肿瘤(13%) |
| Bai et al[ | 11 | 54(43~63) | 9(81.8%) | 步态共济失调(100%),头晕或复视(63.6%),构音障碍(63.4%) | 11/11(100%) | 4/6(66.7%) | 相关自身免疫性疾病(36%),脑炎/癫痫(36%),僵人综合征(9%),肿瘤(9%) |
| [1] |
Mitoma H, Adhikari K, Aeschlimann D, et al. Consensus paper: Neuroimmune mechanisms of cerebellar ataxias[J]. Cerebellum, 2016, 15(2): 213-232.
doi: 10.1007/s12311-015-0664-x pmid: 25823827 |
| [2] | Muñoz-Lopetegi A, Boukhrissi S, et al. Neurologic syndromes related to anti-GAD65: Clinical and serologic response to treatment[J]. Neurol Neuroimmunol Neuroinflamm, 2020, 7(3):e696. |
| [3] | Bai L, Ren H, Liang M, et al. Neurological disorders associated with glutamic acid decarboxylase 65 antibodies: Clinical spectrum and prognosis of a cohort from China[J]. Front Neurol, 2022, 13:990553. |
| [4] | 刘峥, 董会卿, 邱占东, 等. GAD-65抗体相关性小脑性共济失调病例报道及文献回顾[J]. 脑与神经疾病杂志, 2017, 25(7):397-401. |
| [5] | 刘静, 樊春秋, 刘爱华, 等. GAD65抗体相关性小脑共济失调临床及眼震电图一例[J]. 脑与神经疾病杂志, 2020, 28(9):574-577. |
| [6] | 朱丽平, 刘磊, 彭静婷, 等. GAD65抗体相关性小脑性共济失调一例报道及文献复习[J]. 中国神经免疫学和神经病学杂志, 2020, 27(01):46-50. |
| [7] | 杨桦, 赵敏, 任雪飞, 等. 抗谷氨酸脱羧酶65抗体相关性小脑性共济失调1例报道[J]. 国际神经病学神经外科学杂志, 2020, 47(1):85-86. |
| [8] | 高颖, 黄瑶, 侯彦波, 等. 抗谷氨酸脱羧酶65抗体阳性相关中枢神经系统病变临床特点分析[J]. 中风与神经疾病杂志, 2022, 39(7): 647-649. |
| [9] | 任若琳, 张哲, 王亚杰, 等. 抗GAD-65抗体相关小脑性共济失调合并僵人综合征1例[J]. 浙江医学, 2022, 44(7): 758-759+766. |
| [10] | 刘芳芳, 黄培生, 陈金梅, 等. GAD65抗体相关性小脑性共济失调(附1例报告及文献复习)[J]. 中国临床神经科学, 2023, 31(01): 75-80. |
| [11] | Honnorat J, Saiz A, Giometto B, et al. Cerebellar ataxia with anti-glutamic acid decarboxylase antibodies: Study of 14 patients[J]. Arch Neurol, 2001, 58(2): 225-230. |
| [12] |
Saiz A, Blanco Y, Sabater L, et al. Spectrum of neurological syndromes associated with glutamic acid decarboxylase antibodies: Diagnostic clues for this association[J]. Brain, 2008, 131(Pt 10): 2553-2563.
doi: 10.1093/brain/awn183 pmid: 18687732 |
| [13] |
Ariño H, Gresa-Arribas N, Blanco Y, et al. Cerebellar ataxia and glutamic acid decarboxylase antibodies: Immunologic profile and long-term effect of immunotherapy[J]. JAMA Neurol, 2014, 71(8): 1009-1016.
doi: 10.1001/jamaneurol.2014.1011 pmid: 24934144 |
| [14] | Budhram A, Sechi E, Flanagan EP, et al. Clinical spectrum of high-titre GAD65 antibodies[J]. J Neurol Neurosurg Psychiatry, 2021, 92(6):645-654. |
| [15] |
Martin DL, Rimvall K. Regulation of gamma-aminobutyric acid synthesis in the brain[J]. J Neurochem, 1993, 60(2): 395-407.
pmid: 8419527 |
| [16] | Kajita Y, Mushiake H. Heterogeneous GAD65 Expression in subtypes of GABAergic neurons across layers of the cerebral cortex and hippocampus[J]. Front Behav Neurosci, 2021, 15:750869. |
| [17] |
McKeon A, Tracy JA. GAD65 neurological autoimmunity[J]. Muscle Nerve, 2017, 56(1):15-27.
doi: 10.1002/mus.25565 pmid: 28063151 |
| [18] |
Jazebi N, Rodrigo S, Gogia B, et al. Anti-glutamic acid decarboxylase (GAD) positive cerebellar Ataxia with transitioning to progressive encephalomyelitis with rigidity and myoclonus (PERM), responsive to immunotherapy: A case report and review of literature[J]. J Neuroimmunol, 2019, 332:135-137.
doi: S0165-5728(18)30577-0 pmid: 31015081 |
| [19] | Olberg HK, Eide GE, Vedeler CA. Can serum GAD65 antibody levels predict neurological disease or cancer?[J]. J Neuroimmunol, 2019, 336:577025. |
| [20] | Li TR, Zhang YD, Wang Q, et al. Intravenous methylprednisolone or immunoglobulin for anti-glutamic acid decarboxylase 65 antibody autoimmune encephalitis: Which is better?[J]. BMC Neurosci, 2020, 21(1):13. |
| [21] |
Mitoma H, Manto M, Hampe CS. Immune-mediated cerebellar ataxias: Practical Guidelines and therapeutic challenges[J]. Curr Neuropharmacol, 2019, 17(1):33-58.
doi: 10.2174/1570159X16666180917105033 pmid: 30221603 |
| [1] | Wang Tao, Gao Yuwei, Wang Xinghua, Hu Xiuhong, Cui Hongrui, Xu Baozhen, Yang Hongjuan. Correlation of anti-phospholipase A2 receptor antibody with idiopathic membranous nephropathy [J]. Clinical Focus, 2023, 38(7): 606-612. |
| [2] | Sun Wenjing1, Dai Shipeng1, Gu Qing2, Tian Miaomiao1, Shang Haixia1. Correlation between MRI microcoil and antiCCP antibody and RF level in rheumatoid arthritis [J]. Clinical Focus, 2020, 35(5): 449-452. |
| [3] | Hu Yatinga, Liang Zhipingb, Zhang Junchen, Xu Wuhuaa. One case report and literature review of SSCNS [J]. Clinical Focus, 2020, 35(12): 1116-1119. |
| [4] | Sun Mei1, Hou Xiaoxia2, Jin Shanquan1, Shen Feifei1, Cheng Hong1. LGI1 antibodyrelated limbic encephalitis: a case report and literature review [J]. Clinical Focus, 2019, 34(3): 273-275. |
| [5] | Li Tinga, Xu Qiangb, Xing Guangqunc. Analysis of risk factors of thromboembolism in patients with ANCAassociated vasculitis [J]. Clinical Focus, 2019, 34(12): 1098-1101. |
| [6] | Li Shumin, Li Yao, Lin Jianwen, Ren Yanwei, Song Qisheng, Hao Guohua, Wang Suping. Clinical study on correlation between anti PPD antibody and cerebrospinal fluid cytology in patients with tuberculous meningitis [J]. Clinical Focus, 2018, 33(5): 402-404,408. |
| [7] | Zhang Fengxiao. Treatment of Sjogren syndrome: the old and the new [J]. Clinical Focus, 2016, 31(5): 482-485. |
| [8] | Quan Feng;Fan Xuemei;Fang Wenlong. Clinical study of systemic lupus erythematosus associated pulmonary hypertension [J]. Clinical Focus, 2015, 30(12): 1402-1.40414e+007. |
| [9] | GUO Hong-xian;ZHENG Cheng-zhong;YIN Xiao-mei;LI Jun-mei;ZHANG Xiao-mei;MA Shu-feng;GONG Ming-jing. Nine-item assay for combined detection of nonbacterial pathogens in acute lower respiratory infection among children [J]. Clinical Focus, 2014, 29(8): 847-849. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||