Clinical Focus ›› 2024, Vol. 39 ›› Issue (1): 5-11.doi: 10.3969/j.issn.1004-583X.2024.01.001
Previous Articles Next Articles
Meta-analysis of the incidence of extracorporeal membrane oxygenation combined with incident thrombosis
Peng Yimeng, Yao Yang, Li Siyu, Ding Ge, Sun Yanan, Wang Shengyu( )
)
- Department of Pulmonary and Critical Medicine, the First Affiliated Hospital of Xi'an Medical University, Xi'an 710077, China
-
Received:2023-01-11Online:2024-01-20Published:2024-03-22
CLC Number:
Cite this article
Peng Yimeng, Yao Yang, Li Siyu, Ding Ge, Sun Yanan, Wang Shengyu. Meta-analysis of the incidence of extracorporeal membrane oxygenation combined with incident thrombosis[J]. Clinical Focus, 2024, 39(1): 5-11.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.01.001
| 纳入研究 | 年份 | 国家/地区 | 年龄 (岁) | 男性 [例(%)] | 病例 总数 | 研究类型 | V-V | V-A | VA-V | 持续时间 (d) | 血栓 例数 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Parzy[ | 2020 | France | 48.0±16.0 | 71(67.6) | 105 | 回顾性研究 | 105 | 0 | 0 | 10(6,16) | 75 |
| Weber[ | 2018 | Germany | 59.1±14.4 | 216(76.9) | 281 | 回顾性研究 | 281 | 0 | 0 | 99(28,75) | 11 |
| Cartwright[ | 2021 | Australia | 46.7(41.1, 63.7) | 23(59.0) | 39 | 回顾性研究 | 17 | 22 | 0 | VA:3(2,5); VV:10(6,13) | 26 |
| Chandel[ | 2021 | USA | 46(37, 53) | 4(16.7) | 24 | 回顾性研究 | 24 | 0 | 0 | 13(9, 21) | 12 |
| Ripoll[ | 2022 | UK | 45(39, 56) | 24(80.0) | 30 | 回顾性研究 | 30 | 0 | 0 | 4(1, 5) | 13 |
| Moussa[ | 2021 | France | 55±14 | 183(69.1) | 265 | 回顾性研究 | 265 | 0 | 0 | 7(3,11) | 87 |
| Salas De Armas[ | 2022 | USA | 30.6±12.6 | 14(93.3) | 15 | 回顾性研究 | 15 | 0 | 0 | 11.0(7.5,20.0) | 1 |
| Kohs[ | 2022 | USA | 51.1±15.9 | 44(65.7) | 67 | 回顾性研究 | 23 | 44 | 0 | 7.0±5.0 | 16 |
| Zhang[ | 2021 | China | 47(25,73) | 11(73.3) | 15 | 回顾性研究 | 5 | 10 | 0 | 15.0±18.0 | 4 |
| Beyls[ | 2020 | France | 62(56,66) | 10(83.3) | 12 | 回顾性研究 | 12 | 0 | 0 | 4.0(1.5,7.5) | 11 |
| Riera[ | 2020 | Spain | 50.5(31.0,64.0) | 16(84.2) | 19 | 回顾性研究 | 19 | 0 | 0 | 8.6(0,17.0) | 9 |
| Fong[ | 2021 | Hong Kong | 55.0(41.3,62.0) | 85(65.4) | 130 | 回顾性研究 | 79 | 51 | 0 | 5.9(3.6,7.9) | 37 |
| Agerstrand[ | 2016 | New York | 32.6(26.0,39.0) | 0 | 18 | 回顾性研究 | 14 | 1 | 3 | 6.6(6.0,17.8) | 5 |
| Trudzinski[ | 2016 | Germany | 46.0±14.4 | 37(58.7) | 63 | 回顾性研究 | 63 | 0 | 0 | 22.4±17.0 | 29 |
| Agerstrand[ | 2015 | New York | 33(24,53) | 24(63.2) | 38 | 回顾性研究 | 34 | 2 | 1 | 9.0(7.0,11.5) | 8 |
| Roussel[ | 2012 | France | 52(22, 86) | 7(46.7) | 15 | 回顾性研究 | 0 | 15 | 0 | 4.9(1.0,12.0) | 1 |
Tab.1 Basic characteristics of included literature
| 纳入研究 | 年份 | 国家/地区 | 年龄 (岁) | 男性 [例(%)] | 病例 总数 | 研究类型 | V-V | V-A | VA-V | 持续时间 (d) | 血栓 例数 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Parzy[ | 2020 | France | 48.0±16.0 | 71(67.6) | 105 | 回顾性研究 | 105 | 0 | 0 | 10(6,16) | 75 |
| Weber[ | 2018 | Germany | 59.1±14.4 | 216(76.9) | 281 | 回顾性研究 | 281 | 0 | 0 | 99(28,75) | 11 |
| Cartwright[ | 2021 | Australia | 46.7(41.1, 63.7) | 23(59.0) | 39 | 回顾性研究 | 17 | 22 | 0 | VA:3(2,5); VV:10(6,13) | 26 |
| Chandel[ | 2021 | USA | 46(37, 53) | 4(16.7) | 24 | 回顾性研究 | 24 | 0 | 0 | 13(9, 21) | 12 |
| Ripoll[ | 2022 | UK | 45(39, 56) | 24(80.0) | 30 | 回顾性研究 | 30 | 0 | 0 | 4(1, 5) | 13 |
| Moussa[ | 2021 | France | 55±14 | 183(69.1) | 265 | 回顾性研究 | 265 | 0 | 0 | 7(3,11) | 87 |
| Salas De Armas[ | 2022 | USA | 30.6±12.6 | 14(93.3) | 15 | 回顾性研究 | 15 | 0 | 0 | 11.0(7.5,20.0) | 1 |
| Kohs[ | 2022 | USA | 51.1±15.9 | 44(65.7) | 67 | 回顾性研究 | 23 | 44 | 0 | 7.0±5.0 | 16 |
| Zhang[ | 2021 | China | 47(25,73) | 11(73.3) | 15 | 回顾性研究 | 5 | 10 | 0 | 15.0±18.0 | 4 |
| Beyls[ | 2020 | France | 62(56,66) | 10(83.3) | 12 | 回顾性研究 | 12 | 0 | 0 | 4.0(1.5,7.5) | 11 |
| Riera[ | 2020 | Spain | 50.5(31.0,64.0) | 16(84.2) | 19 | 回顾性研究 | 19 | 0 | 0 | 8.6(0,17.0) | 9 |
| Fong[ | 2021 | Hong Kong | 55.0(41.3,62.0) | 85(65.4) | 130 | 回顾性研究 | 79 | 51 | 0 | 5.9(3.6,7.9) | 37 |
| Agerstrand[ | 2016 | New York | 32.6(26.0,39.0) | 0 | 18 | 回顾性研究 | 14 | 1 | 3 | 6.6(6.0,17.8) | 5 |
| Trudzinski[ | 2016 | Germany | 46.0±14.4 | 37(58.7) | 63 | 回顾性研究 | 63 | 0 | 0 | 22.4±17.0 | 29 |
| Agerstrand[ | 2015 | New York | 33(24,53) | 24(63.2) | 38 | 回顾性研究 | 34 | 2 | 1 | 9.0(7.0,11.5) | 8 |
| Roussel[ | 2012 | France | 52(22, 86) | 7(46.7) | 15 | 回顾性研究 | 0 | 15 | 0 | 4.9(1.0,12.0) | 1 |
| 纳入研究 | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | | 总分 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parzy[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 7 |
| Weber[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 7 |
| Cartwright[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 8 |
| Chandel[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Ripoll[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 8 |
| Moussa[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Salas De Armas[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 9 |
| Kohs[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 8 |
| Zhang[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 8 |
| Beyls[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 8 |
| Riera[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 8 |
| Fong[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 9 |
| Agerstrand[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| Trudzinski[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Agerstrand[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Roussel[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
Tab.2 Quality evaluation of included literature
| 纳入研究 | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | | 总分 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parzy[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 7 |
| Weber[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 7 |
| Cartwright[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 8 |
| Chandel[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Ripoll[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 8 |
| Moussa[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Salas De Armas[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 9 |
| Kohs[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 8 |
| Zhang[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 8 |
| Beyls[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 8 |
| Riera[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 8 |
| Fong[ | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 9 |
| Agerstrand[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| Trudzinski[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Agerstrand[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 9 |
| Roussel[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
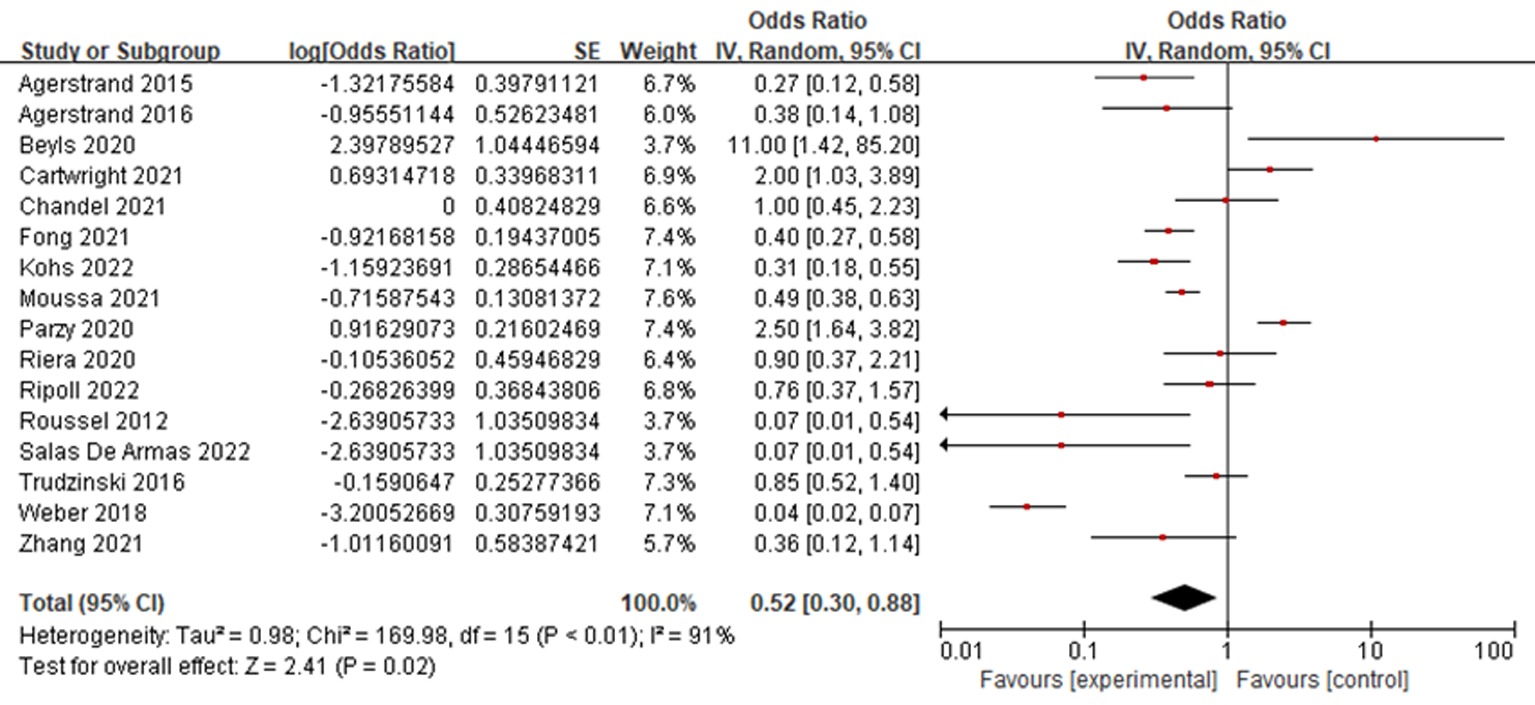
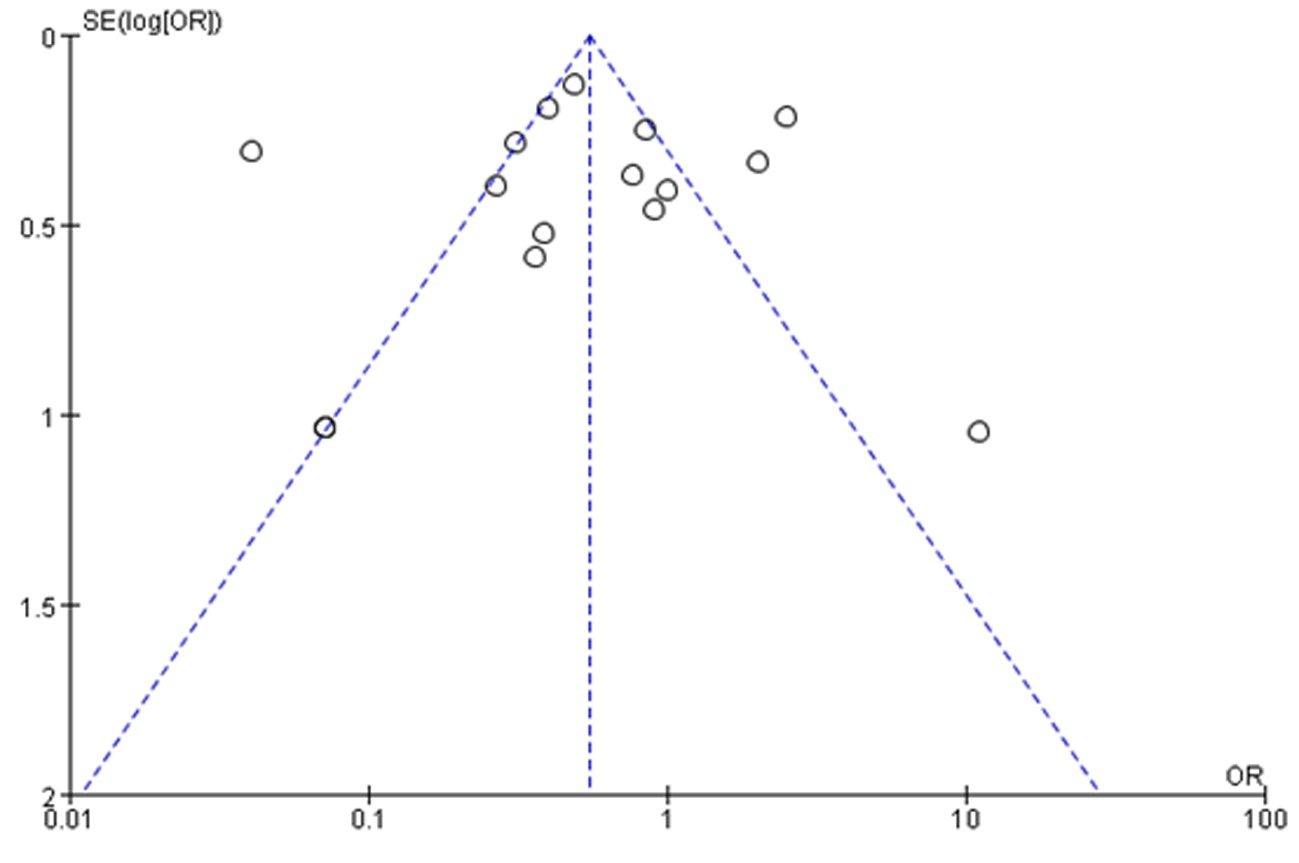
| 亚组 | 纳入研究数 | 异质性检验结果 | 效应模型 | 患病率(95% | |
|---|---|---|---|---|---|
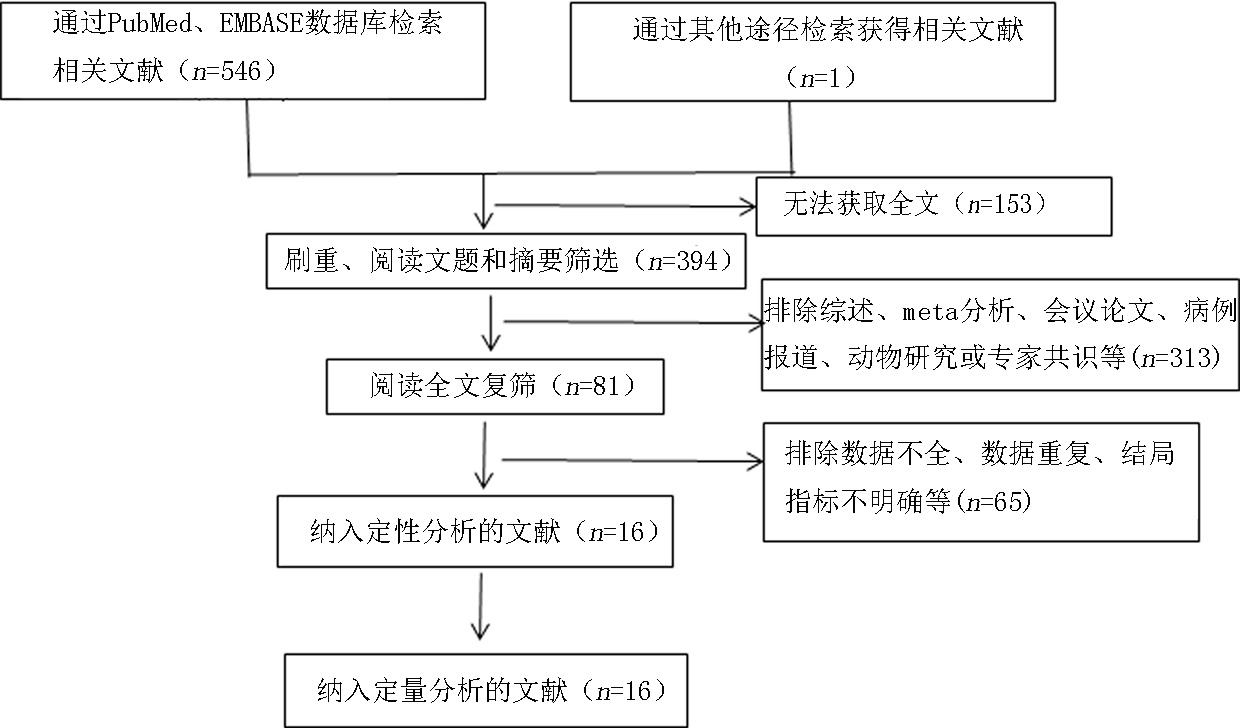
| 总发生率 | 16[ | <0.01 | 91% | 随机 | 52.0%(95% |
| 年龄(岁) | |||||
| <45岁 | 3[ | 0.35 | 5% | 随机 | 27.0%(95% |
| 45~59岁 | 12[ | <0.01 | 93% | 随机 | 53.0%(95% |
| ECMO时间(d) | |||||
| ≤10 | 8[ | 0.008 | 63% | 随机 | 50.0%(95% |
| >10 | 7[ | <0.01 | 95% | 随机 | 39.0%(95% |
| BMI( kg/m2) | |||||
| 24~27.9 | 5[ | <0.01 | 97% | 随机 | 27.0%(95% |
| ≥28 | 6[ | 0.0009 | 76% | 随机 | 66.0%(95% |
| 抗凝监测方式 | |||||
| APTT | 8[ | <0.01 | 95% | 随机 | 57.0%(95% |
| ACT | 3[ | <0.01 | 94% | 随机 | 13.0%(95% |
| 抗fxa | 2[ | 0.16 | 50% | 随机 | 46.0%(95% |
Tab.3 Summary table of Meta-analysis results
| 亚组 | 纳入研究数 | 异质性检验结果 | 效应模型 | 患病率(95% | |
|---|---|---|---|---|---|
| 总发生率 | 16[ | <0.01 | 91% | 随机 | 52.0%(95% |
| 年龄(岁) | |||||
| <45岁 | 3[ | 0.35 | 5% | 随机 | 27.0%(95% |
| 45~59岁 | 12[ | <0.01 | 93% | 随机 | 53.0%(95% |
| ECMO时间(d) | |||||
| ≤10 | 8[ | 0.008 | 63% | 随机 | 50.0%(95% |
| >10 | 7[ | <0.01 | 95% | 随机 | 39.0%(95% |
| BMI( kg/m2) | |||||
| 24~27.9 | 5[ | <0.01 | 97% | 随机 | 27.0%(95% |
| ≥28 | 6[ | 0.0009 | 76% | 随机 | 66.0%(95% |
| 抗凝监测方式 | |||||
| APTT | 8[ | <0.01 | 95% | 随机 | 57.0%(95% |
| ACT | 3[ | <0.01 | 94% | 随机 | 13.0%(95% |
| 抗fxa | 2[ | 0.16 | 50% | 随机 | 46.0%(95% |
| 剔除研究 | 95% | Tau2 | |||
|---|---|---|---|---|---|
| Parzy[ | 0.45 | <0.01 | 88% | 0.28~0.75 | 0.74 |
| Weber[ | 0.64 | <0.01 | 85% | 0.41~0.99 | 0.54 |
| Cartwright[ | 0.47 | <0.01 | 91% | 0.27~0.81 | 0.95 |
| Chandel[ | 0.49 | <0.01 | 92% | 0.28~0.87 | 1.01 |
| Ripoll[ | 0.50 | <0.01 | 92% | 0.28~0.89 | 1.03 |
| Moussa[ | 0.51 | <0.01 | 92% | 0.27~0.98 | 1.36 |
| Salas De Armas[ | 0.56 | <0.01 | 92% | 0.32~0.96 | 0.96 |
| Kohs[ | 0.53 | <0.01 | 92% | 0.30~0.95 | 1.04 |
| Zhang[ | 0.53 | <0.01 | 92% | 0.30~0.92 | 1.00 |
| Beyls[ | 0.46 | <0.01 | 91% | 0.27~0.79 | 0.94 |
| Riera[ | 0.50 | <0.01 | 92% | 0.28~0.87 | 1.01 |
| Fong[ | 0.52 | <0.01 | 92% | 0.29~0.96 | 1.16 |
| Agerstrand[ | 0.52 | <0.01 | 92% | 0.32~0.92 | 1.01 |
| Trudzinski [ | 0.49 | <0.01 | 92% | 0.28~0.89 | 1.08 |
| Agerstrand[ | 0.54 | <0.01 | 92% | 0.31~0.95 | 1.01 |
| Roussel[ | 0.56 | <0.01 | 92% | 0.32~0.96 | 0.96 |
Tab.4 Sensitivity analysis of thrombosis incidence in ECMO patients
| 剔除研究 | 95% | Tau2 | |||
|---|---|---|---|---|---|
| Parzy[ | 0.45 | <0.01 | 88% | 0.28~0.75 | 0.74 |
| Weber[ | 0.64 | <0.01 | 85% | 0.41~0.99 | 0.54 |
| Cartwright[ | 0.47 | <0.01 | 91% | 0.27~0.81 | 0.95 |
| Chandel[ | 0.49 | <0.01 | 92% | 0.28~0.87 | 1.01 |
| Ripoll[ | 0.50 | <0.01 | 92% | 0.28~0.89 | 1.03 |
| Moussa[ | 0.51 | <0.01 | 92% | 0.27~0.98 | 1.36 |
| Salas De Armas[ | 0.56 | <0.01 | 92% | 0.32~0.96 | 0.96 |
| Kohs[ | 0.53 | <0.01 | 92% | 0.30~0.95 | 1.04 |
| Zhang[ | 0.53 | <0.01 | 92% | 0.30~0.92 | 1.00 |
| Beyls[ | 0.46 | <0.01 | 91% | 0.27~0.79 | 0.94 |
| Riera[ | 0.50 | <0.01 | 92% | 0.28~0.87 | 1.01 |
| Fong[ | 0.52 | <0.01 | 92% | 0.29~0.96 | 1.16 |
| Agerstrand[ | 0.52 | <0.01 | 92% | 0.32~0.92 | 1.01 |
| Trudzinski [ | 0.49 | <0.01 | 92% | 0.28~0.89 | 1.08 |
| Agerstrand[ | 0.54 | <0.01 | 92% | 0.31~0.95 | 1.01 |
| Roussel[ | 0.56 | <0.01 | 92% | 0.32~0.96 | 0.96 |
| [1] |
Al-Jazairi A, Raslan S, Al-Mehizia R, et al. Performance assessment of a multifaceted unfractionated heparin dosing protocol in adult patients on extracorporeal membrane oxygenator[J]. Ann Pharmacother, 2021, 55(5):592-604.
doi: 10.1177/1060028020960409 pmid: 32959678 |
| [2] |
Carter KT, Kutcher ME, Shake JG, et al. Heparin-sparing anticoagulation strategies are viable options for patients on veno-venous ECMO[J]. J Surg Res, 2019, 243:399-409.
doi: S0022-4804(19)30379-8 pmid: 31277018 |
| [3] |
Ki K, Passmore MR, Chan CHH, et al. Low flow rate alters haemostatic parameters in an ex-vivo extracorporeal membrane oxygenation circuit[J]. Intensive Care Med Exp, 2019, 7(1):51.
doi: 10.1186/s40635-019-0264-z pmid: 31432279 |
| [4] |
Mihu MR, Mageka D, Swant LV, et al. Veno-arteriovenous extracorporeal membrane oxygenation-A single center experience[J]. Artif Organs, 2021, 45(12):1554-1561.
doi: 10.1111/aor.v45.12 URL |
| [5] |
Padhya DR, Prutsky GJ, Nemergut ME, et al. Routine laboratory measures of heparin anticoagulation for children on extracorporeal membrane oxygenation: Systematic review and meta-analysis[J]. Thromb Res, 2019, 179:132-139.
doi: S0049-3848(19)30234-8 pmid: 31132667 |
| [6] |
Parzy G, Daviet F, Persico N, et al. Prevalence and risk factors for thrombotic complications following venovenous extracorporeal membrane oxygenation: A CT scan study[J]. Crit Care Med, 2020, 48(2):192-199.
doi: 10.1097/CCM.0000000000004129 pmid: 31939787 |
| [7] |
Weber C, Deppe A, Sabashnikov A, et al. Left ventricular thrombus formation in patients undergoing femoral veno-arterial extracorporeal membrane oxygenation[J]. Perfusion, 2018, 33(4):283-288.
doi: 10.1177/0267659117745369 pmid: 29172999 |
| [8] |
Cartwright B, Bruce HM, Kershaw G, et al. Hemostasis, coagulation and thrombin in venoarterial and venovenous extracorporeal membrane oxygenation: The HECTIC study[J]. Sci Rep, 2021, 11(1):7975.
doi: 10.1038/s41598-021-87026-z pmid: 33846433 |
| [9] |
Chandel A, Patolia S, Looby M, et al. Association of D-dimer and Fibrinogen with hypercoagulability in COVID-19 requiring extracorporeal membrane oxygenation[J]. J Intensive Care Med, 2021, 36(6):689-695.
doi: 10.1177/0885066621997039 URL |
| [10] |
Ripoll B, Rubino A, Besser M, et al. Observational study of thrombosis and bleeding in COVID-19 VV ECMO patients[J]. Int J Artif Organs, 2022, 45(2):239-242.
doi: 10.1177/0391398821989065 URL |
| [11] |
Moussa MD, Soquet J, Lamer A, et al. Evaluation of anti-activated factor X activity and activated partial thromboplastin time relations and their association with bleeding and thrombosis during Veno-Arterial ECMO support: A retrospective study[J]. J Clin Med, 2021, 10(10):2158.
doi: 10.3390/jcm10102158 URL |
| [12] |
Salas De Armas IA, Akkanti B, et al. Traumatic respiratory failure and veno-venous extracorporeal membrane oxygenation support[J]. Perfusion, 2022, 37(5):477-483.
doi: 10.1177/02676591211012840 URL |
| [13] |
Kohs TCL, Liu P, Raghunathan V, et al. Severe thrombocytopenia in adults undergoing extracorporeal membrane oxygenation is predictive of thrombosis[J]. Platelets, 2022, 33(4):570-576.
doi: 10.1080/09537104.2021.1961707 URL |
| [14] | Zhang Y, Luo M, Wang B, et al. Perioperative,protective use of extracorporeal membrane oxygenation in complex thoracic surgery[J]. Perfusion, 2021, 2676591211011044. |
| [15] | Beyls C, Huette P, Abou-Arab O, et al. Extracorporeal membrane oxygenation for COVID-19-associated severe acute respiratory distress syndrome and risk of thrombosis[J]. Br J Anaesth, 2020, 125(2):e260-e262. |
| [16] |
Riera J, Argudo E, Martínez-Martínez M, et al. Extracorporeal membrane oxygenation retrieval in coronavirus disease 2019: A case-series of 19 patients supported at a high-volume extracorporeal membrane oxygenation center[J]. Crit Care Explor, 2020, 2(10):e0228.
doi: 10.1097/CCE.0000000000000228 pmid: 33063032 |
| [17] |
Fong KM, Au SY, Ng GWY, et al. Bleeding, thrombosis and transfusion in patients on ECMO: A retrospective study in a tertiary center in Hong Kong[J]. Int J Artif Organs, 2021, 44(6):420-425.
doi: 10.1177/0391398820965584 pmid: 33070679 |
| [18] |
Agerstrand C, Abrams D, Biscotti M, et al. Extracorporeal membrane oxygenation for cardiopulmonary failure during pregnancy and postpartum[J]. Ann Thorac Surg, 2016, 102(3):774-779.
doi: S0003-4975(16)30092-3 pmid: 27154158 |
| [19] |
Trudzinski FC, Minko P, Rapp D, et al. Runtime and aPTT predict venous thrombosis and thromboembolism in patients on extracorporeal membrane oxygenation: A retrospective analysis[J]. Ann Intensive Care, 2016, 6(1):66.
doi: 10.1186/s13613-016-0172-2 pmid: 27432243 |
| [20] |
Agerstrand CL, Burkart KM, Abrams DC, et al. Blood conservation in extracorporeal membrane oxygenation for acute respiratory distress syndrome[J]. Ann Thorac Surg, 2015, 99(2):590-595.
doi: 10.1016/j.athoracsur.2014.08.039 pmid: 25499483 |
| [21] | Roussel A, Al-Attar N, Alkhoder S, et al. Outcomes of percutaneous femoral cannulation for venoarterial extracorporeal membrane oxygenation support[J]. Eur Heart J Acute Cardiovasc Care, 2012, 1(2):111-114. |
| [22] |
Rajan S, Wissenberg M, Folke F, et al. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest[J]. Circulation, 2016, 134(25):2095-2104.
pmid: 27881566 |
| [23] |
McMichael ABV, Zimmerman KO, Kumar KR, et al. Evaluation of effect of scheduled fresh frozen plasma on ECMO circuit life: A randomized pilot trial.[J]. Transfusion, 2021, 61(1):42-51.
doi: 10.1111/trf.16164 pmid: 33269487 |
| [24] |
Colman E, Yin EB, Laine G, et al. Evaluation of a heparin monitoring protocol for extracorporeal membrane oxygenation and review of the literature[J]. J Thorac Dis, 2019, 11(8):3325-3335.
doi: 10.21037/jtd.2019.08.44 pmid: 31559035 |
| [25] |
Yaw HP, Van Den Helm S, MacLaren G, et al. Platelet phenotype and function in the setting of pediatric extracorporeal membrane oxygenation (ECMO): A systematic review[J]. Front Cardiovasc Med, 2019, 6:137.
doi: 10.3389/fcvm.2019.00137 pmid: 31620448 |
| [26] |
Panigada M, E Iapichino G, Brioni M, et al. Thromboelastography-based anticoagulation management during extracorporeal membrane oxygenation: A safety and feasibility pilot study[J]. Ann Intensive Care, 2018, 8(1):7.
doi: 10.1186/s13613-017-0352-8 pmid: 29340875 |
| [27] | Qiu C, Li T, Wei G, et al. Hemorrhage and venous thromboembolism in critically ill patients with COVID-19[J]. SAGE Open Med, 2021, 9:20503121211020167. |
| [28] |
Glorion M, Mercier O, Mitilian D, et al. Central versus peripheral cannulation of extracorporeal membrane oxygenation support during double lung transplant for pulmonary hypertension[J]. Eur J Cardiothorac Surg, 2018, 54(2):341-347.
doi: 10.1093/ejcts/ezy089 pmid: 29528384 |
| [1] | Liu Xiangdong, Cai Yandong, Qin Yanjun, Li Yunsong, Li Liang, Gao Ruijiao, Ren Lei, Zhang Yanrong. Exertional rhabdomyolysis complicated with acute renal insufficiency and catheter-related thrombosis: One case and literature review [J]. Clinical Focus, 2022, 37(9): 831-833. |
| [2] | Chang Yajun, Guo Weina, Guo Qiaozhen, Wang Tianjun. Literature review on one case of cerebral venous sinus thrombosis mainly featured with isolated headache [J]. Clinical Focus, 2022, 37(3): 271-274. |
| [3] | Zhang Xiaole, Cai Zhaoxu, Zhang Heqiong, Wang Yangyang, Lu Shaoyun, Yang Chunwan. Clinical application of thromboelastogram in patients with primary acute myocardial infarction [J]. Clinical Focus, 2021, 36(2): 125-128. |
| [4] | Yin Yuanyuan, Ren Huiling. Cerebral venous sinus thrombosis as the first manifestation of Neuro-Behcet's disease: one case report and literature review [J]. Clinical Focus, 2021, 36(2): 162-167. |
| [5] | Yin Yuanyuan, Ren Huiling. Retrospective analysis of of thrombotic antiphospholipid syndrome: in 7 cases [J]. Clinical Focus, 2021, 36(12): 1123-1127. |
| [6] | Chen Xianrui, Huang Jianqi, Guo Biyun, Wen Hong, Bai Haitao, Xu Jinping. Report of a case of acute monocyac leukemia with the first performance of intracranial venous sinus thrombosis and literature review [J]. Clinical Focus, 2020, 35(1): 76-79. |
| [7] | Shi Zhimin, Zhang Tongqiang, Guo Wei, Ren Lixin, Meng Zhaowei, Xu Yongsheng. A case report of mycoplasma pneumoniacombined pulmonary thromboembolism in child [J]. Clinical Focus, 2019, 34(8): 748-751. |
| [8] | Niu Shaoqian1, Zhang Xiaoqing1, Tian Yingping2a, Fu Xianghua2b. Three cases of patients with cardiac arrest under ECMO and literature review [J]. Clinical Focus, 2019, 34(12): 1115-1118. |
| [9] | Yang Xincheng, Jin Xiaoxu, Yao Jinfeng. Research advances of portal vein thrombosis in liver cirrhosis [J]. Clinical Focus, 2018, 33(11): 947-949,955. |
| [10] | Wu Yuhuai1a, Liu Jianwei2, Liu Jianping1b, Yang Yaopeng1c. Peripherally inserted central catheters and centralvenous catheters related vein thrombosis: a metaanalysis [J]. Clinical Focus, 2017, 32(2): 167-171. |
| [11] | Lu Hua, Huo Pengfei, Liu Qian, Liu Jing, Guo Gengxin. Application of fourstep massage method in maintenance hemodialysis patients with thrombosis of arteriovenous fistula [J]. Clinical Focus, 2016, 31(5): 524-527,531. |
| [12] | Xiao Pengfei,Li Guangping,Ye Lan,Xu Gang,Liu Xia. Influencing factor analysis of left atrial thrombus or spontaneous echo contrast in patients with nonvalvular atrial fibrillation [J]. Clinical Focus, 2016, 31(5): 516-519,523. |
| [13] | Li Hongwei, Wu Qi. Focus on venous thromboembolism during pregnancy [J]. Clinical Focus, 2016, 31(4): 359-362. |
| [14] | Yang Yuanhua, Yang Suqiao,Zhang Mingyuan. New anticoagulants and clinical application of venous thromboembolism [J]. Clinical Focus, 2016, 31(4): 352-354. |
| [15] | Cui Wei. The Year in cardiology 2015 [J]. Clinical Focus, 2016, 31(2): 123-130. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||