

临床荟萃 ›› 2024, Vol. 39 ›› Issue (2): 101-107.doi: 10.3969/j.issn.1004-583X.2024.02.001
• 循证研究 • 下一篇
收稿日期:2023-06-12
出版日期:2024-02-20
发布日期:2024-04-18
通讯作者:
游川
E-mail:2164@nsmc.edu.cn
基金资助:
Gong Caifang1, Zhao Junyu1, You Chuan2( )
)
Received:2023-06-12
Online:2024-02-20
Published:2024-04-18
Contact:
You Chuan
E-mail:2164@nsmc.edu.cn
摘要:
目的 系统评价接纳与承诺疗法(acceptance and commitment therapy,ACT)对癌症患者心理健康和生活质量的影响。方法 检索建库至2022年11月在CBM、万方、知网、维普、PubMed、Cochrane Library、Web of Science、EMbase数据库发表的有关ACT对癌症患者心理健康和生活质量影响的随机对照试验。由2名研究者根据纳入及排除标准独立筛选文献、质量评价并提取数据,采用RevMan 5.4进行meta分析。结果 共纳入14篇文献,1 063例癌症患者。Meta分析结果显示,ACT在改善癌症患者的焦虑[SMD=-1.04,95%CI (-1.19,-0.89),P<0.01]、抑郁情绪[SMD=-0.73,95%CI(-0.88,-0.59),P<0.01], 提升心理灵活性[MD=-2.17,95%CI (-2.77,-1.57),P<0.01]及生活质量[MD=5.27,95%CI(3.57,6.98),P<0.01]方面差异具有统计学意义。结论 ACT有助于缓解癌症患者的焦虑及抑郁情绪, 提升心理灵活性及生活质量, 对促进癌症患者的心理健康和生活质量具有积极作用。
中图分类号:
龚财芳, 赵俊宇, 游川. 接纳与承诺疗法对癌症患者心理健康和生活质量影响的meta分析[J]. 临床荟萃, 2024, 39(2): 101-107.
Gong Caifang, Zhao Junyu, You Chuan. Effect of acceptance and commitment therapy on mental health and quality of life in cancer patients: A meta-analysis[J]. Clinical Focus, 2024, 39(2): 101-107.
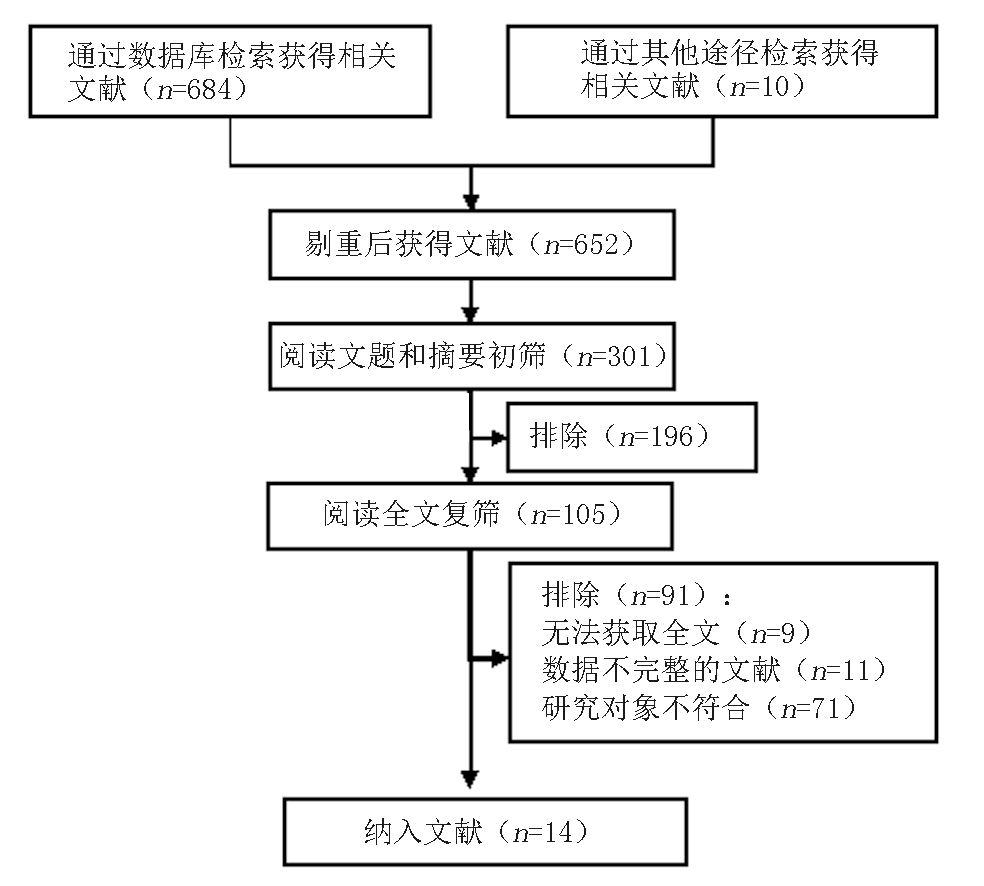
图1 文献筛选流程图 注:所检索的数据库及检出文献数具体如下:CBM(n=92)、WanFang Data(n=121)、CNKI(n=84)、VIP(n=68)、PubMed(n=132)、The Cochrane Library(n=93)、Web of Science(n=61)、Embase(n=43)
Fig. 1 Flow chart of literature screening
| 纳入文献 | 年份 (年) | 癌症 类型 | 样本量(例) | 干预措施 | 干预时间及方式 | 结局指标 | 测量工具 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 观察组 | 对照组 | 观察组 | 对照组 | ||||||||
| Shari等[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 12周,1次/3周,1 h/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Serfaty等[ | 2018 | 各种类型 | 20 | 22 | ACT+TC | TC | 3月,8次/周,1 h/次,面对面 | ③④ | HADS、FACT | ||
| Fernández-Rodríguez等[ | 2020 | 各种类型 | 12 | 17 | ACT | 常规护理 | 3月,12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| González-Fernández等[ | 2018 | 乳腺癌 | 12 | 23 | ACT | 常规护理 | 12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Johns等[ | 2019 | 乳腺癌 | 31 | 31 | ACT | SE | 6周, 1次/7d, 2 h/次,面对面 | ①② | GAD、PHQ | ||
| Li等[ | 2022 | 肺癌 | 20 | 20 | ACT | 常规护理 | 1次/周,60~90 min/次,面对面+网络视频 | ①②④ | GAD、PHQ | ||
| Mohabbat-Bahar等[ | 2015 | 乳腺癌 | 15 | 15 | ACT | 常规护理 | 4周,2次/周,90 min/次,面对面 | ①② | BAI、BHI | ||
| 周小帅[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 2周,1次/2d,30 min/次,面对面 | ①② | SAS、SDS | ||
| 姚晚侠等[ | 2020 | 乳腺癌 | 140 | 140 | ACT | 常规护理 | 3月,1次/月,面对面+电话+微信 | ①② | SAS、SDS | ||
| 潘虹等[ | 2020 | 胰腺癌 | 37 | 42 | ACT | 常规护理 | 8周,6次/周,90 min/次,面对面 | ①②③ | DASS、AAQ-Ⅱ | ||
| 王婷婷等[ | 2022 | 食管癌 | 50 | 50 | ACT | 常规护理 | 4周,面对面 | ①②③④ | SAS、SDS、AAQ-Ⅱ、QLQ-C30 | ||
| 胡迎冬等[ | 2016 | 乳腺癌 | 41 | 39 | ACT | 常规护理 | 2周,1次/2d,30~40 min/次,面对面 | ①②④ | SAS、SDS、FACT | ||
| 许湘华等[ | 2019 | 喉癌 | 24 | 24 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ③④ | AAQ-Ⅱ、FACT | ||
| 魏慧等[ | 2020 | 直肠癌 | 59 | 59 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ①② | HADS、AAQ-Ⅱ | ||
表1 纳入文献基本特征
Tab.1 Basic information of included studies
| 纳入文献 | 年份 (年) | 癌症 类型 | 样本量(例) | 干预措施 | 干预时间及方式 | 结局指标 | 测量工具 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 观察组 | 对照组 | 观察组 | 对照组 | ||||||||
| Shari等[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 12周,1次/3周,1 h/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Serfaty等[ | 2018 | 各种类型 | 20 | 22 | ACT+TC | TC | 3月,8次/周,1 h/次,面对面 | ③④ | HADS、FACT | ||
| Fernández-Rodríguez等[ | 2020 | 各种类型 | 12 | 17 | ACT | 常规护理 | 3月,12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| González-Fernández等[ | 2018 | 乳腺癌 | 12 | 23 | ACT | 常规护理 | 12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Johns等[ | 2019 | 乳腺癌 | 31 | 31 | ACT | SE | 6周, 1次/7d, 2 h/次,面对面 | ①② | GAD、PHQ | ||
| Li等[ | 2022 | 肺癌 | 20 | 20 | ACT | 常规护理 | 1次/周,60~90 min/次,面对面+网络视频 | ①②④ | GAD、PHQ | ||
| Mohabbat-Bahar等[ | 2015 | 乳腺癌 | 15 | 15 | ACT | 常规护理 | 4周,2次/周,90 min/次,面对面 | ①② | BAI、BHI | ||
| 周小帅[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 2周,1次/2d,30 min/次,面对面 | ①② | SAS、SDS | ||
| 姚晚侠等[ | 2020 | 乳腺癌 | 140 | 140 | ACT | 常规护理 | 3月,1次/月,面对面+电话+微信 | ①② | SAS、SDS | ||
| 潘虹等[ | 2020 | 胰腺癌 | 37 | 42 | ACT | 常规护理 | 8周,6次/周,90 min/次,面对面 | ①②③ | DASS、AAQ-Ⅱ | ||
| 王婷婷等[ | 2022 | 食管癌 | 50 | 50 | ACT | 常规护理 | 4周,面对面 | ①②③④ | SAS、SDS、AAQ-Ⅱ、QLQ-C30 | ||
| 胡迎冬等[ | 2016 | 乳腺癌 | 41 | 39 | ACT | 常规护理 | 2周,1次/2d,30~40 min/次,面对面 | ①②④ | SAS、SDS、FACT | ||
| 许湘华等[ | 2019 | 喉癌 | 24 | 24 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ③④ | AAQ-Ⅱ、FACT | ||
| 魏慧等[ | 2020 | 直肠癌 | 59 | 59 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ①② | HADS、AAQ-Ⅱ | ||
| 结局指标 | 纳入研究 | 异质性 | 效应模型 | Meta分析结果 | ||||
|---|---|---|---|---|---|---|---|---|
| P值 | I2(%) | SMD/MD | 95%CI | Z值 | P值 | |||
| 焦虑评分 | 11 | 0.36 | 9 | 固定 | -0.99* | [-1.14,-0.85] | 13.62 | <0.01 |
| 抑郁评分 | 10 | 0.29 | 16 | 固定 | -0.68* | [-0.83,-0.54] | 9.42 | <0.01 |
| 心理灵活性 | 6 | 0.95 | 0 | 固定 | -2.17# | [-2.77,-1.57] | 7.11 | <0.01 |
| 生活质量 | 4 | 0.10 | 49 | 固定 | 0.70* | [0.43,0.97] | 5.10 | <0.01 |
表2 敏感性分析结果
Tab.2 Result of sensitivity analysis
| 结局指标 | 纳入研究 | 异质性 | 效应模型 | Meta分析结果 | ||||
|---|---|---|---|---|---|---|---|---|
| P值 | I2(%) | SMD/MD | 95%CI | Z值 | P值 | |||
| 焦虑评分 | 11 | 0.36 | 9 | 固定 | -0.99* | [-1.14,-0.85] | 13.62 | <0.01 |
| 抑郁评分 | 10 | 0.29 | 16 | 固定 | -0.68* | [-0.83,-0.54] | 9.42 | <0.01 |
| 心理灵活性 | 6 | 0.95 | 0 | 固定 | -2.17# | [-2.77,-1.57] | 7.11 | <0.01 |
| 生活质量 | 4 | 0.10 | 49 | 固定 | 0.70* | [0.43,0.97] | 5.10 | <0.01 |
| [1] |
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71 (3): 209-249.
doi: 10.3322/caac.v71.3 URL |
| [2] | 王思颖, 郑幸玲, 覃文新. 癌症患者能否长期生存?[J]. 上海交通大学学报, 2021, 55(z1):49-50. |
| [3] | 贾莉莉, 朱康宁, 张国增, 等. 癌症患者疾病感知的研究进展[J]. 中华护理教育, 2020, 17 (8):765-768. |
| [4] |
Huda N, Shaw MK, Chang HJ. Psychological distress among patients with advanced cancer: A conceptual analysis[J]. Cancer Nurs, 2022, 45 (2):E487-E503.
doi: 10.1097/NCC.0000000000000940 URL |
| [5] |
Burhan HŞ, Karadere E. Effectiveness of acceptance and commitment therapy for patients with psychosis being monitored at a community mental health center: A six-month follow-up study[J]. Alpha Psychiatry, 2021, 22 (4): 206-211.
doi: 10.5455/apd.93130 pmid: 36424936 |
| [6] |
Esmali A, Alizadeh M. The effectiveness of group psychotherapy based on acceptance and commitment on increasing of mental health and the quality of women’s life with breast cancer[J]. Biosci Biotechnol Res Asia, 2015, 12 (3): 2253-2260.
doi: 10.13005/bbra/ URL |
| [7] |
Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: Model, processes and outcomes[J]. Behav Res Ther, 2006, 44 (1): 1-25.
doi: 10.1016/j.brat.2005.06.006 pmid: 16300724 |
| [8] | Yıldız E. The effects of acceptance and commitment therapy in psychosis treatment: A systematic review of randomized controlled trials[J]. Perspect Psychiatr C, 2019, 56 (1):149-167. |
| [9] |
Sakamoto R, Ohtake Y, Kataoka Y, et al. Efficacy of acceptance and commitment therapy for people with type 2 diabetes: Systematic review and meta-analysis[J]. J Diabetes Invest, 2021, 13 (2): 262-270.
doi: 10.1111/jdi.13658 pmid: 34486816 |
| [10] |
Ghorbani V, Zanjani Z, Omidi A, et al. Efficacy of acceptance and commitment therapy (ACT) on depression, pain acceptance, and psychological flexibility in married women with breast cancer: A pre- and post-test clinical trial[J]. Trends Psychiatry Psychother, 2021, 43(2):126-133.
doi: 10.47626/2237-6089-2020-0022 pmid: 34392667 |
| [11] |
Shari NI, Zainal NZ, Ng CG. Effects of brief acceptance and commitment therapy (ACT) on subjective cognitive impairment in breast cancer patients undergoing chemotherapy[J]. J Psychosoc Oncol, 2020, 39 (6):695-714.
doi: 10.1080/07347332.2020.1856283 URL |
| [12] |
Serfaty M, Armstrong M, Vickerstaff V, et al. Acceptance and commitment therapy for adults with advanced cancer (CanACT): A feasibility randomised controlled trial[J]. Psycho Oncology, 2018, 28 (3):488-496.
doi: 10.1002/pon.v28.3 URL |
| [13] | Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version5.1.0[M]. London: The Cochrane Collaboration, 2011:150-151. |
| [14] |
Fernández-Rodríguez C, González-Fernández S, Coto-lesmes R, et al. Behavioral activation and acceptance and commitment therapy in the treatment of anxiety and depression in cancer survivors: A randomized clinical trial[J]. Behav Modif, 2020, 45 (5):822-859.
doi: 10.1177/0145445520916441 URL |
| [15] |
González-Fernández S, Fernández-Rodríguez C, Paz-Caballero M, et al. Treating anxiety and depression of cancer survivors: Behavioral activation versus acceptance and commitment therapy[J]. Psicothema, 2018, 30 (1):14-20.
doi: 10.7334/psicothema2017.396 pmid: 29363465 |
| [16] | Johns SA, Stutz PV, Talib TL, et al. Acceptance and commitment therapy for breast cancer survivors with fear of cancer recurrence: A 3-arm pilot randomized controlled trial[J]. Cancer Am Cancer Soc, 2019, 126 (1):211-218. |
| [17] | Li H, Jin X, Ng M, et al. Effects of Acceptance and commitment therapy on fatigue interference and health-related quality of life among patients with advanced lung cancer: A pilot randomized controlled trial[J]. Asia Pac J Oncol Nur, 2022, 9 (8):100102. |
| [18] | Mohabbat-Bahar S, Maleki-Rizi F, Akbari ME, et al. Effectiveness of group training based on acceptance and commitment therapy on anxiety and depression of women with breast cancer[J]. Iran J Cancer Prev, 2015, 8 (2):71-6. |
| [19] | 周小帅. 接纳与承诺疗法在乳腺癌根治术后患者护理中的应用效果[J]. 中国民康医学, 2020, 32(11):151-153. |
| [20] | 姚晚侠, 何苗, 李春华, 等. 接纳与承诺疗法在乳腺癌术后化疗患者中的应用及效果观察[J]. 护士进修杂志, 2020, 35(24):2275-2277. |
| [21] | 潘虹, 罗冰, 遆甜, 等. 接受与承诺疗法对晚期胰腺癌病人心理应激的影响[J]. 护理研究, 2020, 34(7):1279-1282. |
| [22] |
王婷婷, 杨孝苹. 接纳与承诺疗法对食管癌术后患者负性情绪及生活质量的影响[J]. 中国临床护理, 2022, 14(2):90-93.
doi: 10.3969/j.issn.1674-3768.2022.02.006 |
| [23] | 胡迎冬, 蒋维连. 接纳与承诺疗法对乳腺癌术后患者焦虑抑郁情绪及生命质量的影响[J]. 中国实用护理杂志, 2016, 32(29):2265-2268. |
| [24] | 许湘华, 欧美军, 谢婵娟, 等. 接纳与承诺疗法在喉癌术后患者中的应用效果[J]. 解放军护理杂志, 2019, 36(5):6-10. |
| [25] | 魏慧, 薛晓红, 刘梅红. 接纳与承诺疗法对直肠癌患者疼痛及负性情绪的影响[J]. 癌症进展, 2020, 18(23):2472-2475. |
| [26] |
Chinh K, Mosher CE, Brown LF, et al. Psychological processes and symptom outcomes in mindfulness-based stress reduction for cancer survivors: A pilot study[J]. Mindfulness, 2020, 11 (4): 905-916.
doi: 10.1007/s12671-019-01299-0 pmid: 33456623 |
| [27] | 陶元玲, 孙丽, 张立力. 晚期癌症患者灵性应对现状及影响因素研究[J]. 护理管理杂志, 2022, 22(2):105-110. |
| [28] |
Mitchell AJ, Ferguson DW, Gill J, et al. Depression and anxiety in long- term cancer survivors compared with spouses and healthy controls: A systematic review and meta-analysis[J]. Lancet Oncol, 2013, 14 (8):721-32.
doi: 10.1016/S1470-2045(13)70244-4 pmid: 23759376 |
| [29] |
Walker J, Magill N, Mulick A, et al. Different independent associations of depression and anxiety with survival in patients with cancer[J]. J Psychosom Res, 2020, 138 110218.
doi: 10.1016/j.jpsychores.2020.110218 URL |
| [30] | Wersebe H, Lieb R, Meyer AH, et al. The link between stress, well-being, and psychological flexibility during an acceptance and commitment therapy self-help intervention[J]. Int J Clin Hlth Psyc, 2017, 18 (1):60-68. |
| [31] |
Lv J, Zhu L, Wu X, et al. Study on the correlation between postoperative mental flexibility, negative emotions, and quality of life in patients with thyroid cancer[J]. Gland Surg, 2021, 10 (8):2471-2476.
doi: 10.21037/gs-21-424 pmid: 34527559 |
| [32] |
Li H, Wu J, Ni Q, et al. Systematic review and meta-analysis of effectiveness of acceptance and commitment therapy in patients with breast cancer[J]. Nurs Res, 2021, 70 (4):E152-E160.
doi: 10.1097/NNR.0000000000000499 pmid: 33492055 |
| [33] |
Twohig MP, Levin ME. Acceptance and commitment therapy as a treatment for anxiety and depression: A review[J]. Psychiat Clin N Am, 2017, 40 (4):751-770.
doi: 10.1016/j.psc.2017.08.009 URL |
| [34] |
Yu L, Mccracken LM. Model and processes of acceptance and commitment therapy (ACT) for chronic pain including a closer look at the self[J]. Curr Pain Headache R, 2016, 20(2):12.
doi: 10.1007/s11916-016-0541-4 pmid: 26803836 |
| [35] |
Coto-Lesmes R, Fernández-Rodríguez C, González-Fernández S. Acceptance and commitment therapy in group format for anxiety and depression: A systematic review[J]. J Affect Disorders, 2019, 263: 107-120.
doi: 10.1016/j.jad.2019.11.154 URL |
| [36] |
Bai Z, Luo S, Zhang L, et al. Acceptance and commitment therapy (ACT) to reduce depression: A systematic review and meta-analysis[J]. J Affect Disorders, 2019, 260:728-737.
doi: 10.1016/j.jad.2019.09.040 URL |
| [37] |
Zhao C, Lai L, Zhang L, et al. The effects of acceptance and commitment therapy on the psychological and physical outcomes among cancer patients: A meta-analysis with trial sequential analysis[J]. J Psychosom Res, 2020, 140 110304.
doi: 10.1016/j.jpsychores.2020.110304 URL |
| [1] | 肖煌怡, 袁建坤, 严梓予, 曾雯姝, 鲁兰莫, 王峻. 认知干预对遗忘型轻度认知障碍老年患者干预效果的meta分析[J]. 临床荟萃, 2024, 39(1): 12-19. |
| [2] | 吕畅, 周利明. TNF-α-308基因多态性与胃癌易感相关性的meta分析[J]. 临床荟萃, 2023, 38(9): 779-787. |
| [3] | 李海, 刘文虎, 彭绍鹏, 王飞. 控制性阶梯式减压术对比快速标准大骨瓣减压术治疗重度颅脑损伤疗效的meta分析[J]. 临床荟萃, 2023, 38(9): 788-795. |
| [4] | 侯有玲, 李奕, 关红玉, 罗红霞. 目标导向液体治疗在脑肿瘤切除术中应用效果的meta分析[J]. 临床荟萃, 2023, 38(8): 686-693. |
| [5] | 肖王静, 李欣梦, 卢松玲, 孙雪华. 重复经颅磁刺激治疗中枢神经源性吞咽障碍疗效及安全性的meta分析[J]. 临床荟萃, 2023, 38(7): 588-599. |
| [6] | 金家辉, 杨阳, 秦铜, 何雨欣, 苏美华. 补充益生菌对2型糖尿病患者糖代谢改善的meta分析[J]. 临床荟萃, 2023, 38(7): 581-587. |
| [7] | 尤奕, 高淑清, 徐浩. 肠内营养对食管癌患者术后临床结局影响的系统综述[J]. 临床荟萃, 2023, 38(6): 485-492. |
| [8] | 倪艺芸, 刘彬, 梁琪, 李晓凤. 白细胞介素6和C反应蛋白预测新型冠状病毒肺炎严重程度的meta分析[J]. 临床荟萃, 2023, 38(6): 493-499. |
| [9] | 沃拉孜汗·玛德尼亚提, 迪力夏提·图尔迪麦麦提, 李梦晨, 拜合提尼沙·吐尔地. 宏基因组二代测序技术在肺结核诊断中应用价值的meta分析[J]. 临床荟萃, 2023, 38(5): 389-398. |
| [10] | 赵哲, 穆培娟, 张冬. 恩度联合顺铂胸腔灌注治疗肺癌合并恶性胸腔积液疗效的meta分析[J]. 临床荟萃, 2023, 38(5): 399-404. |
| [11] | 马明福, 魏志国, 何铁英. 急性胰腺炎并发胰腺假性囊肿危险因素的meta分析[J]. 临床荟萃, 2023, 38(4): 293-301. |
| [12] | 曹宇萌, 张海燕, 刘立新. 非酒精性脂肪性肝病的病理改变与血清铁蛋白和血清铁含量变化关系的meta分析[J]. 临床荟萃, 2023, 38(3): 197-207. |
| [13] | 马宏莉, 陆皓, 王丹, 焦海星, 李一珂, 李思雨, 吕静. 脑卒中患者残疾危险因素的meta分析[J]. 临床荟萃, 2023, 38(2): 111-116. |
| [14] | 陶嘉楠, 李文茜, 马秀雯, 安琪, 王学红. HER-2在肝细胞癌中表达及临床意义的meta分析[J]. 临床荟萃, 2023, 38(12): 1067-1072. |
| [15] | 柯孟婷, 陈慰. 瑞舒伐他汀降压作用的meta分析[J]. 临床荟萃, 2023, 38(11): 965-971. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||