Clinical Focus ›› 2021, Vol. 36 ›› Issue (5): 402-407.doi: 10.3969/j.issn.1004-583X.2021.05.003
Previous Articles Next Articles
Influencing factors of myocardial microcirculation perfusion disorder after percutaneous coronary intervention in acute myocardial infarction and relationship with lactic acid
Shi Jun, Liu Xinbing, Bai Yanyan, Yue Dandan, Wang Xiaoqing, Liu Tianhua, Feng Liuliu( )
)
- Department of Cardiology, Shidong Hospital, Yangpu District, Shanghai 200438, China
-
Received:2021-03-01Online:2021-05-20Published:2021-06-09 -
Contact:Feng Liuliu E-mail:llf20170101@126.com
CLC Number:
Cite this article
Shi Jun, Liu Xinbing, Bai Yanyan, Yue Dandan, Wang Xiaoqing, Liu Tianhua, Feng Liuliu. Influencing factors of myocardial microcirculation perfusion disorder after percutaneous coronary intervention in acute myocardial infarction and relationship with lactic acid[J]. Clinical Focus, 2021, 36(5): 402-407.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2021.05.003
| 项目 | 观察组 (n=56) | 对照组 (n=76) | χ2值 | P值 |
|---|---|---|---|---|
| 性别 | ||||
| 男性 女性 | 31(55.36) 25(44.64) | 40(52.63) 36(47.37) | 0.096 | 0.756 |
| 年龄 | ||||
| ≥60岁 <60岁 | 35(62.50) 21(37.50) | 46(60.53) 30(39.47) | 0.053 | 0.818 |
| Killip分级 | ||||
| Ⅰ级 | 17(30.36) | 24(31.58) | ||
| Ⅱ级 | 26(46.43) | 34(44.74) | 0.039 | 0.844 |
| Ⅲ级 | 13(23.21) | 18(23.68) | ||
| FMC-H时间 | ||||
| ≤4 h >4 h | 8(14.29) 48(85.71) | 58(76.32) 18(23.68) | 49.624 | <0.01 |
| 症状-FMC时间 | ||||
| ≤4 h >4 h | 10(17.86) 46(82.14) | 56(73.68) 20(26.32) | 40.195 | <0.01 |
| 术后TIMI血流 | ||||
| 0级 | 3(5.36) | 0(0.00) | ||
| 1级 | 10(17.86) | 0(0.00) | 50.750 | <0.01 |
| 2级 | 30(53.57) | 13(17.11) | ||
| 3级 | 13(23.21) | 63(82.89) | ||
| 病变分支 | ||||
| 单支病变 多支病变 | 37(66.07) 19(33.93) | 48(63.16) 28(36.84) | 0.119 | 0.730 |
| MACEs | ||||
| 有 无 | 42(75.00) 14(25.00) | 35(46.05) 41(53.95) | 11.116 | 0.001 |
| 糖尿病病史 | ||||
| 有 无 | 41(73.21) 15(26.79) | 37(48.68) 39(51.32) | 8.026 | 0.005 |
| 冠状动脉慢血流 | ||||
| 是 否 | 40(71.43) 16(28.57) | 35(46.05) 41(53.95) | 8.462 | 0.004 |
| 高血压病史 | ||||
| 有 无 | 42(75.00) 14(25.00) | 38(50.00) 38(50.00) | 8.440 | 0.004 |
| 吸烟史 | ||||
| 有 无 | 42(75.00) 14(25.00) | 40(52.63) 36(47.37) | 6.856 | 0.009 |
| 项目 | 观察组 (n=56) | 对照组 (n=76) | χ2值 | P值 |
|---|---|---|---|---|
| 性别 | ||||
| 男性 女性 | 31(55.36) 25(44.64) | 40(52.63) 36(47.37) | 0.096 | 0.756 |
| 年龄 | ||||
| ≥60岁 <60岁 | 35(62.50) 21(37.50) | 46(60.53) 30(39.47) | 0.053 | 0.818 |
| Killip分级 | ||||
| Ⅰ级 | 17(30.36) | 24(31.58) | ||
| Ⅱ级 | 26(46.43) | 34(44.74) | 0.039 | 0.844 |
| Ⅲ级 | 13(23.21) | 18(23.68) | ||
| FMC-H时间 | ||||
| ≤4 h >4 h | 8(14.29) 48(85.71) | 58(76.32) 18(23.68) | 49.624 | <0.01 |
| 症状-FMC时间 | ||||
| ≤4 h >4 h | 10(17.86) 46(82.14) | 56(73.68) 20(26.32) | 40.195 | <0.01 |
| 术后TIMI血流 | ||||
| 0级 | 3(5.36) | 0(0.00) | ||
| 1级 | 10(17.86) | 0(0.00) | 50.750 | <0.01 |
| 2级 | 30(53.57) | 13(17.11) | ||
| 3级 | 13(23.21) | 63(82.89) | ||
| 病变分支 | ||||
| 单支病变 多支病变 | 37(66.07) 19(33.93) | 48(63.16) 28(36.84) | 0.119 | 0.730 |
| MACEs | ||||
| 有 无 | 42(75.00) 14(25.00) | 35(46.05) 41(53.95) | 11.116 | 0.001 |
| 糖尿病病史 | ||||
| 有 无 | 41(73.21) 15(26.79) | 37(48.68) 39(51.32) | 8.026 | 0.005 |
| 冠状动脉慢血流 | ||||
| 是 否 | 40(71.43) 16(28.57) | 35(46.05) 41(53.95) | 8.462 | 0.004 |
| 高血压病史 | ||||
| 有 无 | 42(75.00) 14(25.00) | 38(50.00) 38(50.00) | 8.440 | 0.004 |
| 吸烟史 | ||||
| 有 无 | 42(75.00) 14(25.00) | 40(52.63) 36(47.37) | 6.856 | 0.009 |
| 相关因素 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| FMC-H | 2.987 | 0.555 | 29.003 | 0.000 | 19.834 | 6.687 | 58.827 |
| 症状-FMC | 2.584 | 0.546 | 22.366 | 0.000 | 13.250 | 4.541 | 38.664 |
| TIMI血流 | 2.535 | 0.444 | 32.610 | 0.000 | 12.619 | 5.286 | 30.126 |
| MACEs | 1.352 | 0.499 | 7.339 | 0.007 | 3.864 | 1.453 | 10.276 |
| 糖尿病病史 | 1.058 | 0.379 | 7.791 | 0.005 | 2.881 | 1.370 | 6.057 |
| 冠状动脉慢血流 | 1.075 | 0.375 | 8.220 | 0.004 | 2.929 | 1.405 | 6.105 |
| 高血压病史 | 1.099 | 0.385 | 8.162 | 0.004 | 3.000 | 1.412 | 6.374 |
| 吸烟史 | 0.993 | 0.385 | 6.665 | 0.010 | 2.700 | 1.270 | 5.739 |
| 相关因素 | 回归系数 | 标准误 | Wald χ2值 | P值 | OR值 | 95%CI | |
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| FMC-H | 2.987 | 0.555 | 29.003 | 0.000 | 19.834 | 6.687 | 58.827 |
| 症状-FMC | 2.584 | 0.546 | 22.366 | 0.000 | 13.250 | 4.541 | 38.664 |
| TIMI血流 | 2.535 | 0.444 | 32.610 | 0.000 | 12.619 | 5.286 | 30.126 |
| MACEs | 1.352 | 0.499 | 7.339 | 0.007 | 3.864 | 1.453 | 10.276 |
| 糖尿病病史 | 1.058 | 0.379 | 7.791 | 0.005 | 2.881 | 1.370 | 6.057 |
| 冠状动脉慢血流 | 1.075 | 0.375 | 8.220 | 0.004 | 2.929 | 1.405 | 6.105 |
| 高血压病史 | 1.099 | 0.385 | 8.162 | 0.004 | 3.000 | 1.412 | 6.374 |
| 吸烟史 | 0.993 | 0.385 | 6.665 | 0.010 | 2.700 | 1.270 | 5.739 |
| 灌注障碍情况 | 例数 | 乳酸预测 | |
|---|---|---|---|
| 心肌微循环灌注障碍 | 心肌微循环灌注正常 | ||
| 心肌微循环灌注障碍 | 56 | 51(91.1) | 5(8.9) |
| 心肌微循环灌注正常 | 76 | 3(3.9) | 73(96.1) |
| 合计 | 132 | 54 | 78 |
| 灌注障碍情况 | 例数 | 乳酸预测 | |
|---|---|---|---|
| 心肌微循环灌注障碍 | 心肌微循环灌注正常 | ||
| 心肌微循环灌注障碍 | 56 | 51(91.1) | 5(8.9) |
| 心肌微循环灌注正常 | 76 | 3(3.9) | 73(96.1) |
| 合计 | 132 | 54 | 78 |
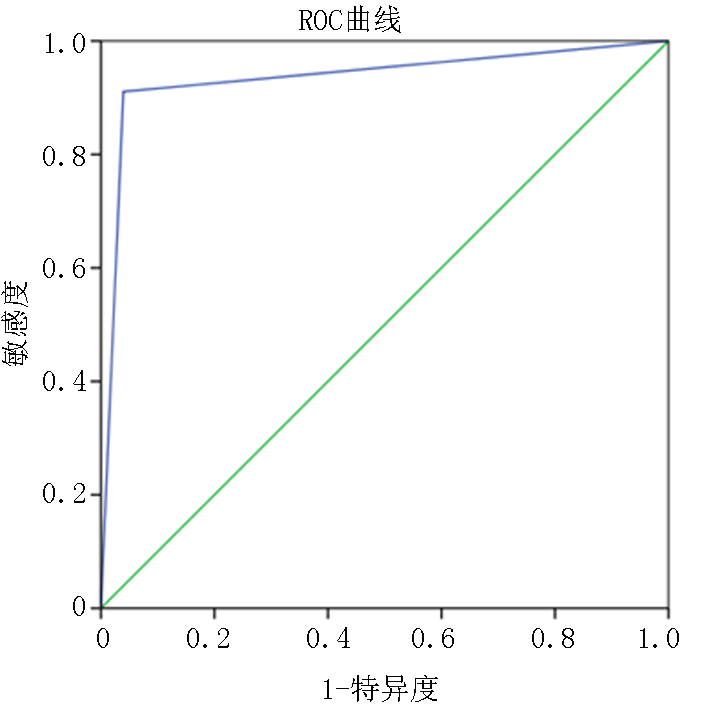
| 预测项目 | AUC | 标准误 | P值 | 95%CI | 敏感度 | 特异度 | 约登指数 | 界值 | |
|---|---|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||||
| 乳酸预测 | 0.936 | 0.026 | 0.000 | 0.885 | 0.986 | 91.10 | 96.10 | 0.872 | 1.50 |
| 预测项目 | AUC | 标准误 | P值 | 95%CI | 敏感度 | 特异度 | 约登指数 | 界值 | |
|---|---|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||||
| 乳酸预测 | 0.936 | 0.026 | 0.000 | 0.885 | 0.986 | 91.10 | 96.10 | 0.872 | 1.50 |
| 组别 | 例数 | 乳酸 (mmol/L) | FMC-H 时间(h) | 症状-FMC 时间(h) | TIMI血流 (级) |
|---|---|---|---|---|---|
| 观察组 | 56 | 3.46±1.20 | 5.84±1.13 | 5.29±0.11 | 1.43±0.19 |
| 对照组 | 76 | 1.15±0.13 | 2.59±0.43 | 1.43±0.25 | 2.89±0.21 |
| t值 | 16.672 | 22.945 | 108.013 | 41.085 | |
| P值 | <0.01 | <0.01 | <0.01 | <0.01 |
| 组别 | 例数 | 乳酸 (mmol/L) | FMC-H 时间(h) | 症状-FMC 时间(h) | TIMI血流 (级) |
|---|---|---|---|---|---|
| 观察组 | 56 | 3.46±1.20 | 5.84±1.13 | 5.29±0.11 | 1.43±0.19 |
| 对照组 | 76 | 1.15±0.13 | 2.59±0.43 | 1.43±0.25 | 2.89±0.21 |
| t值 | 16.672 | 22.945 | 108.013 | 41.085 | |
| P值 | <0.01 | <0.01 | <0.01 | <0.01 |
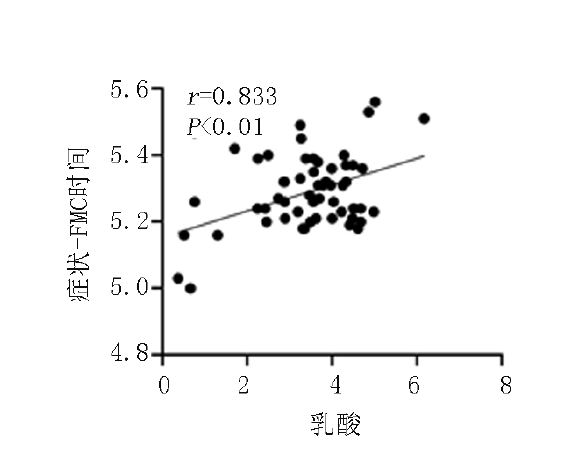
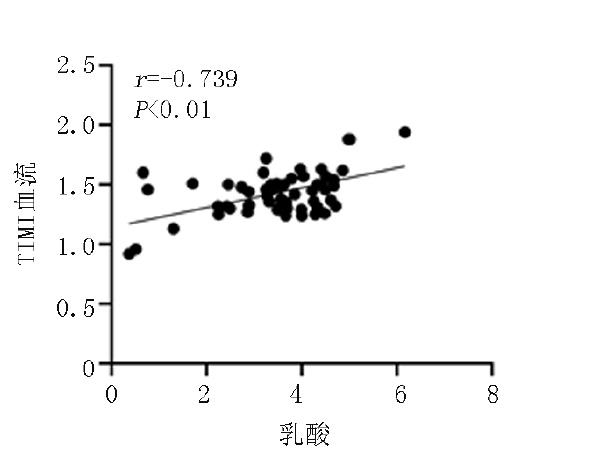
| 指标 | 乳酸 | FMC-H 时间 | 症状- FMC时间 | TIMI血流 | MACEs | 糖尿病 病史 | 冠状动脉 慢血流 | 高血压 病史 | 吸烟史 |
|---|---|---|---|---|---|---|---|---|---|
| 心肌微循环灌注状态 | |||||||||
| r值 | -0.825 | -0.896 | -0.994 | 0.963 | 0.278 | 0.247 | 0.253 | 0.253 | 0.228 |
| P值 | 0.000 | 0.000 | 0.000 | 0.000 | 0.001 | 0.004 | 0.003 | 0.003 | 0.009 |
| 乳酸 | |||||||||
| r值 | - | 0.890 | 0.833 | -0.739 | -0.229 | -0.227 | -0.196 | -0.253 | -0.128 |
| P值 | - | 0.000 | 0.000 | 0.000 | 0.008 | 0.009 | 0.024 | 0.003 | 0.144 |
| 指标 | 乳酸 | FMC-H 时间 | 症状- FMC时间 | TIMI血流 | MACEs | 糖尿病 病史 | 冠状动脉 慢血流 | 高血压 病史 | 吸烟史 |
|---|---|---|---|---|---|---|---|---|---|
| 心肌微循环灌注状态 | |||||||||
| r值 | -0.825 | -0.896 | -0.994 | 0.963 | 0.278 | 0.247 | 0.253 | 0.253 | 0.228 |
| P值 | 0.000 | 0.000 | 0.000 | 0.000 | 0.001 | 0.004 | 0.003 | 0.003 | 0.009 |
| 乳酸 | |||||||||
| r值 | - | 0.890 | 0.833 | -0.739 | -0.229 | -0.227 | -0.196 | -0.253 | -0.128 |
| P值 | - | 0.000 | 0.000 | 0.000 | 0.008 | 0.009 | 0.024 | 0.003 | 0.144 |
| [1] | 潘庆丽, 霍本良, 王立旗. 盐酸替罗非班对ST段抬高型心肌梗死急诊介入治疗后冠状动脉微循环的影响[J]. 岭南心血管病杂志, 2017, 23(6):662-664. |
| [2] | 姜荣泸. 微循环阻力指数对冠状动脉完全闭塞病变患者择期行PCI治疗的预测价值及影响因素分析[J]. 岭南心血管病杂志, 2016, 22(6):645-648, 665. |
| [3] | 段天兵. 急性心肌梗死后冠状动脉微循环障碍发生机制和诊治方法的研究进展[J]. 中国循环杂志, 2019, 34(7):722-725. |
| [4] | 陈宇, 黎荣山, 王勇, 等. 乳酸与急性心肌梗死介入治疗后微循环障碍关系研究[J]. 中国循证心血管医学杂志, 2018, 10(4):432-435. |
| [5] | 陈凤英. 急性ST段抬高心肌梗死的救治及中国经皮冠状动脉介入治疗指南(2016)要点解读[J]. 中华急诊医学杂志, 2016, 25(7):857-861. |
| [6] | 邢晓莲, 刘庆利, 刘连杰, 等. 急性ST段抬高型心肌梗死早期再灌注治疗后微循环灌注状态的研究[J]. 实用医学杂志, 2016, 32(24):4024-4026. |
| [7] | Feng L, Wu B, Zhan L, et al. GW29-e1560 A study on the integration of psychological elasticity and influencing factors in patients with acute myocardial infarction[J]. J Am Coll Cardiol, 2018, 72(16):C224. |
| [8] | 王丽荣, 李萌玫, 王旭. 急性心肌梗死PCI术后围术期心肌梗死影响因素分析及近期预后[J]. 中国临床医学, 2017, 24(4):615-619. |
| [9] | 李晓彤, 张勤, 胡林婕, 等. 前壁心肌梗死急诊介入术后患者微循环障碍的影响因素[J]. 解放军护理杂志, 2018, 35(10):39-42. |
| [10] | 刘兴邦, 牛杰, 王贵松, 等. 非心肌梗死冠心病患者的心肌微循环阻力指数及相关因素分析[J]. 中国循环杂志, 2018, 33(7):637-641. |
| [11] | Cui KY, Yuan F, Liu H, et al. Long-term outcomes of staged recanalization for concurrent chronic total occlusion in patients with ST-segment elevation myocardial infarction after primary percutaneous coronary intervention[J]. J Geriatr Cardiol, 2020, 17(1):16-25. |
| [12] | 李轶男, 王萍, 陈晖. 冠状动脉微循环障碍对心肌纤维化的影响及研究现状[J]. 中国介入心脏病学杂志, 2018, 26(8):53-56. |
| [13] | 高天林, 祝鹏, 袁博, 等. 介入治疗对急性心肌梗死患者心功能及微循环相关指标的影响观察[J]. 实用临床医药杂志, 2017, 21(13):198-199. |
| [14] | 郭刚, 吴先正, 苏立杰. 急诊BNP和乳酸检测对急性心肌梗死病人病情及预后评估的价值[J]. 中西医结合心脑血管病杂志, 2017, 15(1):76-76. |
| [15] | Yang Da-hao, Li Hua-long, Liu Qiang, et al. Relationship between diastolic blood pressure and adverse outcomes in ST-elevation myocardial infarction undergoing percutaneous coronary intervention[J]. Lingnan Journal of Cardiovascular Diseases (English Edition), 2020, 21(1):1-5, 11. |
| [16] | 韦淑婧, 陈宇, 黎荣山, 等. 乳酸与急性ST段抬高型心肌梗死患者介入治疗预后关系[J]. 心肺血管病杂志, 2017, 36(11):883-887. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||