Clinical Focus ›› 2022, Vol. 37 ›› Issue (5): 406-411.doi: 10.3969/j.issn.1004-583X.2022.05.003
Previous Articles Next Articles
Efficacy and safety of anticoagulant therapy for patients with heart failure in sinus rhythm
Li Heng, Li Yonghui, Sun Xiaoqiang, Wang Lin, He Feng( )
)
- Department of Cardiology, Tianjin Fourth Central Hospital, Tianjin 300140, China
-
Received:2021-08-18Online:2022-05-20Published:2022-06-22 -
Contact:He Feng E-mail:abianyu1129@sina.com
CLC Number:
Cite this article
Li Heng, Li Yonghui, Sun Xiaoqiang, Wang Lin, He Feng. Efficacy and safety of anticoagulant therapy for patients with heart failure in sinus rhythm[J]. Clinical Focus, 2022, 37(5): 406-411.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2022.05.003
| 研究/时间 | 设计 类型 | 样本量 (例) | LVEF (%) | 平均年龄 (岁) | 性别 (男/女,例) | 随访时间 | 抗凝与抗血小板措施 | 终点事件 | Jadad质量 评分(分) |
|---|---|---|---|---|---|---|---|---|---|
| COMPASS-HF[ | RCT | 5 903 | ≤35 | 65.5±9.0 | 3 955/1 948 | 36个月 | 利伐沙班/利伐沙班+ASA vs ASA | 主要:心血管死亡、卒中、心肌梗死 安全性:主要出血事件 | 7 |
| WASH[ | RCT | 279 | ≤35 | 63.5 | 209/67 | (27±1)个月 | 华法林(INR2-3)vs阿司匹林(300 mg,1次/d)vs安慰剂 | 主要:全因死亡、非致死性心肌梗死、非致死性卒中 次要:死亡、心因性再入院(主要出血、心力衰竭再入院、卒中、血栓) | 5 |
| HELAS[ | RCT | 197 | ≤35, 缺血性心脏病 | 61.6 | 175/22 | 19.5个月 | 华法林(INR2-3) vs阿司匹林(325 mg,1次/d) vs安慰剂 | 主要:非致死性卒中、血栓、心肌梗死、再入院、心力衰竭加重、死亡 次要:主要出血事件 | 4 |
| ADHERE[ | R | 13 217 | ≤35 | 78 | 7 137/6 080 | 1年 | 华法林vs非华法林 | 全因死亡、血栓事件、主要心血管事件(包括主要出血),心力衰竭再入院 | 5 |
| WARCEF[ | RCT | 2 305 | ≤35 | 61 | 1 844/461 | (3.5±1.8)年 | 华法林(INR2-3.5) vs阿司匹林(325 mg,1次/d) | 主要:缺血性卒中、颅内出血、死亡 次要:心肌梗死、再入院 | 4 |
| ATLAS-HF[ | RCT | 1 694 | >30~≤40 | 63.7±9.9 | 1 118/576 | 13~31个月 | 利伐沙班(2.5/5 mg, 2次/d) vs安慰剂 | 主要:心血管死亡、心肌梗死、卒中 次要:全因死亡、心肌梗死、卒中,安全性:主要出血事件 | 6 |
| WATCH[ | RCT | 1 063 | ≤35 | 63 | 904/159 | 1.9年 | 华法林(INR2.5-3.0) vs阿司匹林(162 mg,1次/d) | 主要:全因死亡、非致死性心肌梗死、非致死性卒中、主要出血事件 次要:死亡、非致死性卒中、心力衰竭再入院 | 7 |
| BEST[ | R | 1 642 | 23 | 57±13 | 1 248/394 | 2.1年 | 华法林v s非华法林 | 主要:全因死亡 次要:心血管或心力衰竭死亡,全因死亡及心力衰竭再入院 | 5 |
| COMMAN-DER HF[ | RCT | 5 022 | ≤40 | 66.4±10.2 | 3 867/1 155 | 21.1个月 | 利伐沙班(2.5 mg,2次/d) vs安慰剂 | 主要:死亡、心肌梗死、卒中 次要:致死性或主要出血 | 7 |
| 研究/时间 | 设计 类型 | 样本量 (例) | LVEF (%) | 平均年龄 (岁) | 性别 (男/女,例) | 随访时间 | 抗凝与抗血小板措施 | 终点事件 | Jadad质量 评分(分) |
|---|---|---|---|---|---|---|---|---|---|
| COMPASS-HF[ | RCT | 5 903 | ≤35 | 65.5±9.0 | 3 955/1 948 | 36个月 | 利伐沙班/利伐沙班+ASA vs ASA | 主要:心血管死亡、卒中、心肌梗死 安全性:主要出血事件 | 7 |
| WASH[ | RCT | 279 | ≤35 | 63.5 | 209/67 | (27±1)个月 | 华法林(INR2-3)vs阿司匹林(300 mg,1次/d)vs安慰剂 | 主要:全因死亡、非致死性心肌梗死、非致死性卒中 次要:死亡、心因性再入院(主要出血、心力衰竭再入院、卒中、血栓) | 5 |
| HELAS[ | RCT | 197 | ≤35, 缺血性心脏病 | 61.6 | 175/22 | 19.5个月 | 华法林(INR2-3) vs阿司匹林(325 mg,1次/d) vs安慰剂 | 主要:非致死性卒中、血栓、心肌梗死、再入院、心力衰竭加重、死亡 次要:主要出血事件 | 4 |
| ADHERE[ | R | 13 217 | ≤35 | 78 | 7 137/6 080 | 1年 | 华法林vs非华法林 | 全因死亡、血栓事件、主要心血管事件(包括主要出血),心力衰竭再入院 | 5 |
| WARCEF[ | RCT | 2 305 | ≤35 | 61 | 1 844/461 | (3.5±1.8)年 | 华法林(INR2-3.5) vs阿司匹林(325 mg,1次/d) | 主要:缺血性卒中、颅内出血、死亡 次要:心肌梗死、再入院 | 4 |
| ATLAS-HF[ | RCT | 1 694 | >30~≤40 | 63.7±9.9 | 1 118/576 | 13~31个月 | 利伐沙班(2.5/5 mg, 2次/d) vs安慰剂 | 主要:心血管死亡、心肌梗死、卒中 次要:全因死亡、心肌梗死、卒中,安全性:主要出血事件 | 6 |
| WATCH[ | RCT | 1 063 | ≤35 | 63 | 904/159 | 1.9年 | 华法林(INR2.5-3.0) vs阿司匹林(162 mg,1次/d) | 主要:全因死亡、非致死性心肌梗死、非致死性卒中、主要出血事件 次要:死亡、非致死性卒中、心力衰竭再入院 | 7 |
| BEST[ | R | 1 642 | 23 | 57±13 | 1 248/394 | 2.1年 | 华法林v s非华法林 | 主要:全因死亡 次要:心血管或心力衰竭死亡,全因死亡及心力衰竭再入院 | 5 |
| COMMAN-DER HF[ | RCT | 5 022 | ≤40 | 66.4±10.2 | 3 867/1 155 | 21.1个月 | 利伐沙班(2.5 mg,2次/d) vs安慰剂 | 主要:死亡、心肌梗死、卒中 次要:致死性或主要出血 | 7 |
| [1] |
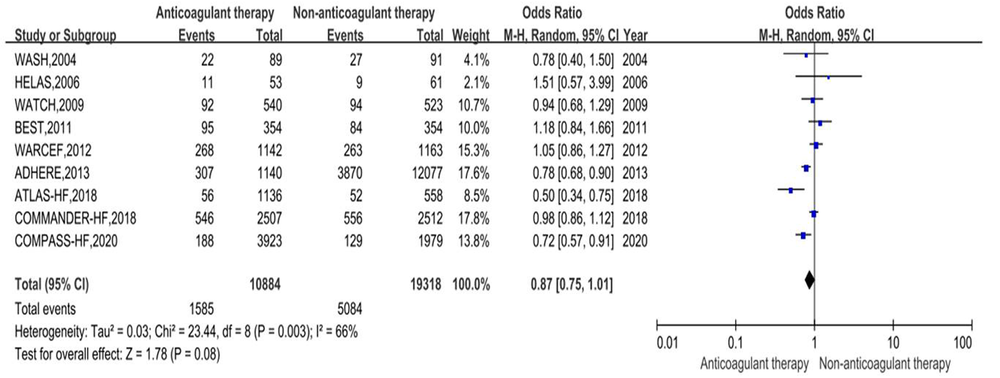
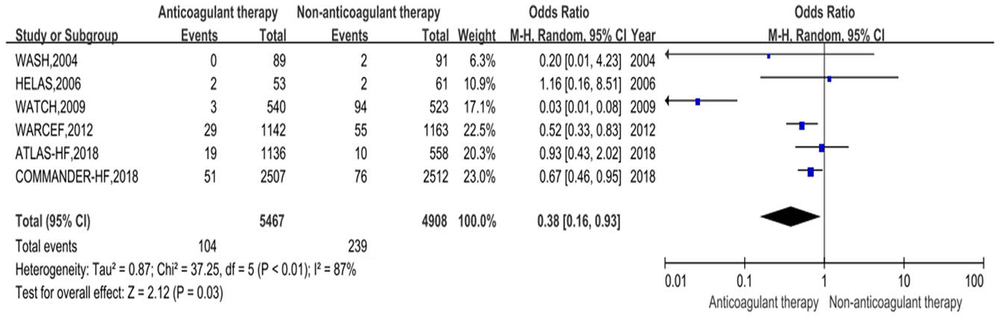
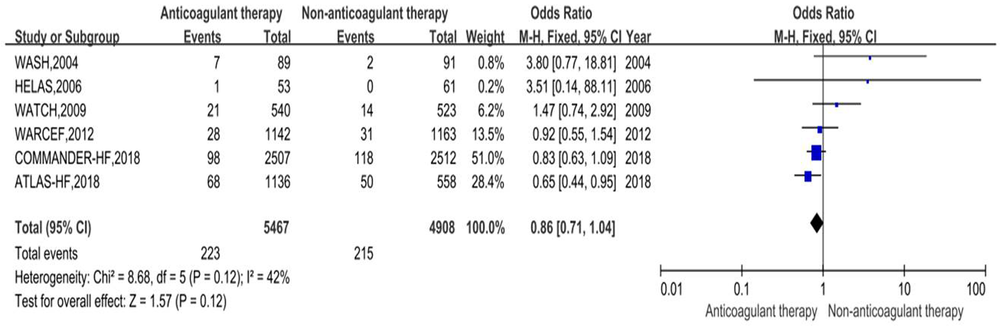
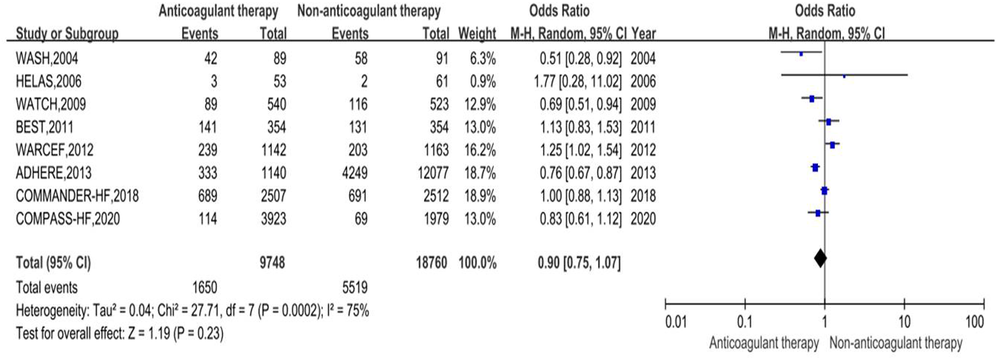
Lin AY, Dinatolo E, Metra M, et al. Thromboembolism in heart failure patients in sinus rhythm: Epidemiology, pathophysiology, clinical trials, and future direction[J]. JACC Heart Fail, 2021, 9(4): 243-253.
doi: 10.1016/j.jchf.2021.01.009 URL |
| [2] |
Shantsila E, Lip GY. Preventing thrombosis to improve outcomes in heart failure patients[J]. Prog Cardiovasc Dis, 2016, 58(4): 386-392.
doi: 10.1016/j.pcad.2015.09.005 pmid: 26433062 |
| [3] |
Jug B, Vene N, Salobir BG, et al. Procoagulant state in heart failure with preserved left ventricular ejection fraction[J]. Int Heart J, 2009, 50(5): 591-600.
doi: 10.1536/ihj.50.591 URL |
| [4] |
Al-khadra AS, Salem DN, Rand WM, et al. Warfarin anticoagulation and survival: A cohort analysis from the studies of left ventricular dysfunction[J]. J Am Coll Cardiol, 1998, 31(4): 749-753.
pmid: 9525542 |
| [5] |
Branch KR, Probstfield JL, Eikelboom JW, et al. Rivaroxaban with or without aspirin in patients with heart failure and chronic coronary or peripheral artery disease[J]. Circulation, 2019, 140(7): 529-537.
doi: 10.1161/CIRCULATIONAHA.119.039609 URL |
| [6] |
Cleland JG, Findlay I, Jafri S, et al. The Warfarin/Aspirin Study in Heart failure (WASH): A randomized trial comparing antithrombotic strategies for patients with heart failure[J]. Am Heart J, 2004, 148(1): 157-164.
pmid: 15215806 |
| [7] |
Cokkinos DV, Haralabopoulos GC, Kostis JB, et al. Efficacy of antithrombotic therapy in chronic heart failure: The HELAS study[J]. Eur J Heart Fail, 2006, 8(4): 428-432.
pmid: 16737850 |
| [8] |
Hernandez AF, Hammill BG, Kociol RD, et al. Clinical effectiveness of anticoagulation therapy among older patients with heart failure and without atrial fibrillation: Findings from the ADHERE registry linked to Medicare claims[J]. J Card Fail, 2013, 19(6): 401-407.
doi: 10.1016/j.cardfail.2013.04.004 pmid: 23743489 |
| [9] |
Homma S, Thompson JL, Pullicino PM, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm[J]. N Engl J Med, 2012, 366(20): 1859-1869.
doi: 10.1056/NEJMoa1202299 URL |
| [10] |
Korjian S, Braunwald E, Daaboul Y, et al. Usefulness of rivaroxaban for secondary prevention of acute coronary syndrome in patients with history of congestive heart failure (from the ATLAS-ACS-2 TIMI-51 Trial)[J]. Am J Cardiol, 2018, 122(11): 1896-1901.
doi: S0002-9149(18)31733-8 pmid: 30340765 |
| [11] |
Massie BM, Collins JF, Ammon SE, et al. Randomized trial of warfarin, aspirin, and clopidogrel in patients with chronic heart failure: The Warfarin and Antiplatelet Therapy in Chronic Heart Failure (WATCH) trial[J]. Circulation, 2009, 119(12): 1616-1624.
doi: 10.1161/CIRCULATIONAHA.108.801753 pmid: 19289640 |
| [12] |
Mujib M, Rahman AA, Desai RV, et al. Warfarin use and outcomes in patients with advanced chronic systolic heart failure without atrial fibrillation, prior thromboembolic events, or prosthetic valves[J]. Am J Cardiol, 2011, 107(4): 552-557.
doi: 10.1016/j.amjcard.2010.10.012 URL |
| [13] |
Zannad F, Anker SD, Byra WM, et al. Rivaroxaban in patients with heart failure, sinus rhythm, and coronary disease[J]. N Engl J Med, 2018, 379(14): 1332-1342.
doi: 10.1056/NEJMoa1808848 URL |
| [14] |
Vogiatzi G, Pantazis A, Tousoulis D. Antithrombotic treatment in cardiomyopathies[J]. Curr Pharm Des, 2020, 26(23): 2762-2768.
doi: 10.2174/1381612826666200429230726 URL |
| [15] |
Jackson SL, Tong X, King RJ, et al. National burden of heart failure events in the United States, 2006 to 2014[J]. Circ Heart Fail, 2018, 11(12): e004873.
doi: 10.1161/CIRCHEARTFAILURE.117.004873 URL |
| [16] |
Kim W, Kim EJ. Heart failure as a risk factor for stroke[J]. J Stroke, 2018, 20(1): 33-45.
doi: 10.5853/jos.2017.02810 URL |
| [17] |
Nygaard MH, Hvas AM, Grove EL. Efficacy and safety of oral anticoagulants in patients with systolic heart failure in sinus rhythm: A systematic review and meta-analysis of randomized controlled trials and cohort studies[J]. TH Open, 2020, 4(4): e383-e392.
doi: 10.1055/s-0040-1720961 pmid: 33274311 |
| [18] |
Li X, Yang J, Xu D. Anticoagulation in patients with heart failure and sinus rhythm[J]. Int Heart J, 2020, 61(6): 1204-1211.
doi: 10.1536/ihj.20-248 URL |
| [19] |
Sulzgruber P, Wassmann S, Semb AG, et al. Oral anticoagulation in patients with non-valvular atrial fibrillation and a CHA2DS2-VASc score of 1: A current opinion of the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy and European Society of Cardiology Council on Stroke[J]. Eur Heart J Cardiovasc Pharmacother, 2019, 5(3): 171-180.
doi: 10.1093/ehjcvp/pvz016 URL |
| [20] |
Melgaard L, Gorst-rasmussen A, Lane DA, et al. Assessment of the CHA2DS2-VASc Score in predicting ischemic stroke, thromboembolism, and death in patients with heart failure with and without atrial fibrillation[J]. JAMA, 2015, 314(10): 1030-1038.
doi: 10.1001/jama.2015.10725 pmid: 26318604 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||