Clinical Focus ›› 2022, Vol. 37 ›› Issue (10): 905-911.doi: 10.3969/j.issn.1004-583X.2022.10.004
Previous Articles Next Articles
Effect of subclinical hypothyroidism on prognosis of patients with chronic systolic heart failure: A meta-analysis
Zuo Xiuxiu1,2, Hou Tianhua2( ), Wang Hongxiang1,2
), Wang Hongxiang1,2
- 1. Chengde Medical University, Chengde 067000, China
2. Department of Cardiology, Chengde Central Hospital, Chengde 067000, China
-
Received:2022-06-17Online:2022-10-20Published:2022-11-26 -
Contact:Hou Tianhua E-mail:houtianhua-00@163.com
CLC Number:
Cite this article
Zuo Xiuxiu, Hou Tianhua, Wang Hongxiang. Effect of subclinical hypothyroidism on prognosis of patients with chronic systolic heart failure: A meta-analysis[J]. Clinical Focus, 2022, 37(10): 905-911.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2022.10.004
| 作者 | 年份 | 国家 | 总人数/甲状腺正常人数/亚临床甲减人数 | TSH界值(mIU/L) | 随访时间(月) | 平均年龄(岁) | 男性占比(%) | 结局 | 调整因素 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 对照组 | 试验组 | |||||||||
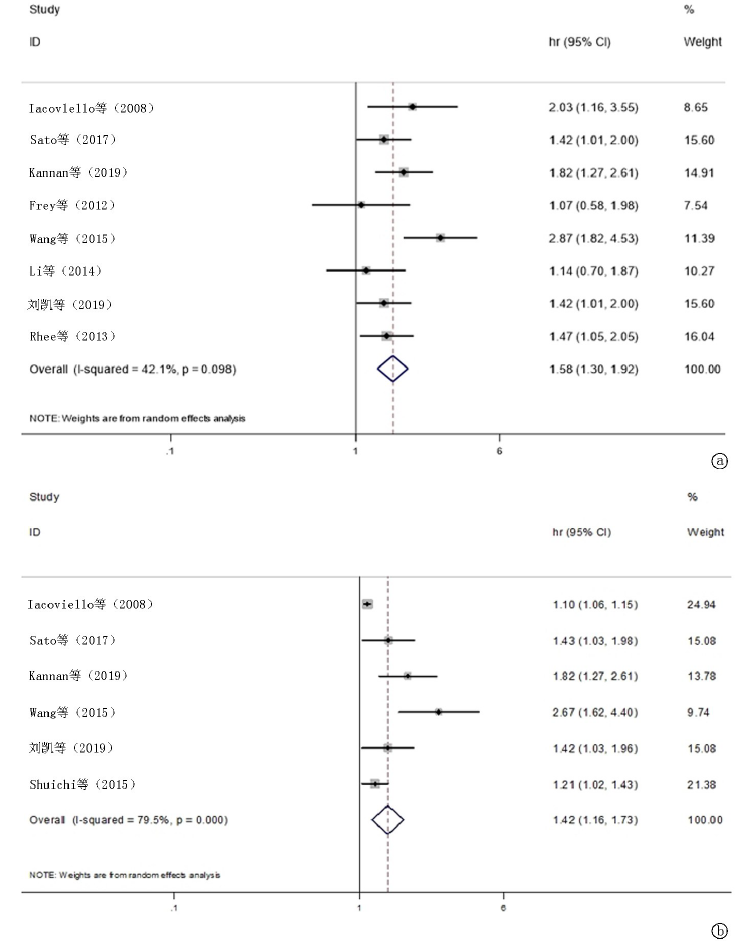
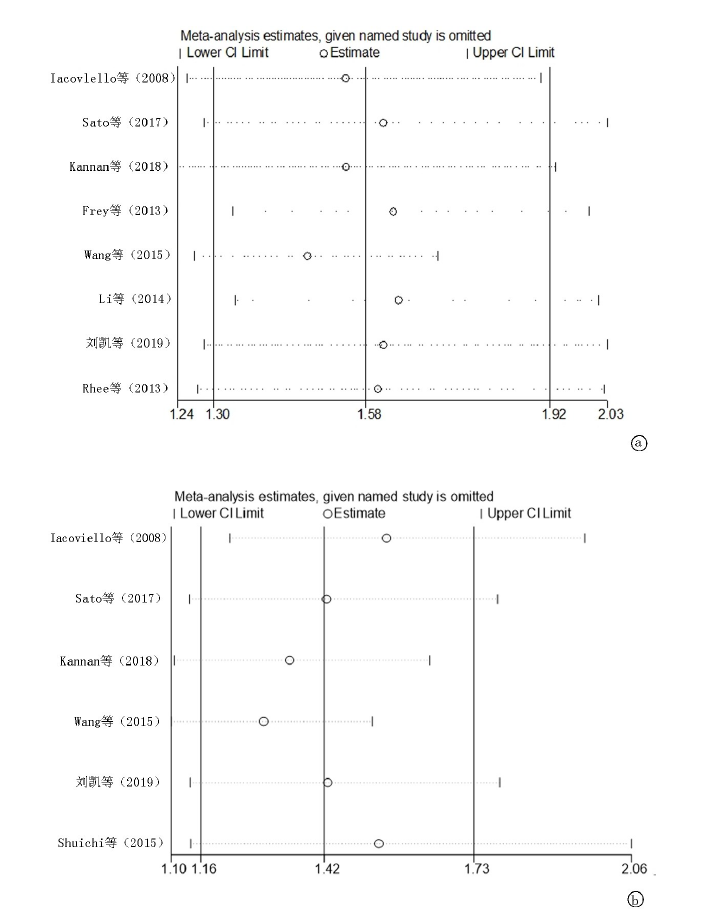
| Iacoviello等[ | 2008 | 意大利 | 338/304/34 | >0.35 | >5.5 | 16 | 64 | 77 | 心脏事件 全因死亡 住院率 | 年龄,糖尿病,NYHA分级,平均动脉压,心率,心房颤动,左室射血分数,左室舒张末期内径、心肌梗死、肾小球滤过率,血红蛋白,钠离子,NT-proBNP、ACEI或ARB药物的缺乏治疗 |
| Sato等[ | 2018 | 日本 | 1100/911/132 | >0.4 | >4 | 36 | 67 | 73 | 心脏事件 全因死亡 | 年龄,性别,体重指数,收缩压,心率,NYHA分级,是否有缺血性因素,高血压、糖尿病、慢性肾脏病,贫血,心房颤动,吸烟史,钠离子,C反应蛋白,BNP,左室射血分数 |
| Kannan等[ | 2018 | 美国 | 1365/1006/74 | >0.45 | >4.51 | 50 | 56.6 | 65 | 心脏事件 全因死亡 | 年龄,性别,种族,体重指数,缺血性病因,胺碘酮的使用,甲状腺药物使用 |
| Frey等[ | 2013 | 德国 | 758/628/34 | >0.3 | >4.0 | 37 | 68 | 71 | 全因死亡 | 年龄 |
| Wang等[ | 2015 | 中国 | 458/353/41 | >0.55 | >4.78 | 17 | 51 | 71 | 住院率 心脏事件 全因死亡 | 年龄,性别,贫血,肾脏功能障碍,高脂血症,吸烟,糖尿病 |
| Li等[ | 2014 | 中国 | 963/816/79 | >0.35 | >5.5 | 42 | 52.1 | 73.7 | 全因死亡 | 年龄,性别,高血压史,心房颤动,室性心动过速,饮酒吸烟,左室直径,左房直径,左室射血分数,FT3,T3,T4,亚临床甲亢,亚临床甲减 |
| 刘凯等[ | 2019 | 中国 | 1100/911/132 | >0.4 | >4 | 36.6 | 71.3 | 55.8 | 心脏事件 全因死亡 | 年龄、性别、体重指数、收缩压,心率,NYHA分级,缺血性心脏病,高血压,糖尿病,血脂水平,慢性肾病,贫血,心房颤动,吸烟史,血钠,C-反应蛋白、BNP和左室射血分数 |
| Rhee等[ | 2013 | 美国 | 15570/14130/691 | >0.39 | >4.6 | 429 | 46.7 | 46.5 | 全因死亡 | 年龄,性别,种族,糖尿病,吸烟,高血压,高胆固醇血症,BMI,既往脑卒中,心肌梗死 |
| Shuichi等[ | 2015 | 日本 | 71/61/8 | >0.35 | >5.5 | 无 | 无 | 无 | 住院率 | 无 |
| 作者 | 年份 | 国家 | 总人数/甲状腺正常人数/亚临床甲减人数 | TSH界值(mIU/L) | 随访时间(月) | 平均年龄(岁) | 男性占比(%) | 结局 | 调整因素 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 对照组 | 试验组 | |||||||||
| Iacoviello等[ | 2008 | 意大利 | 338/304/34 | >0.35 | >5.5 | 16 | 64 | 77 | 心脏事件 全因死亡 住院率 | 年龄,糖尿病,NYHA分级,平均动脉压,心率,心房颤动,左室射血分数,左室舒张末期内径、心肌梗死、肾小球滤过率,血红蛋白,钠离子,NT-proBNP、ACEI或ARB药物的缺乏治疗 |
| Sato等[ | 2018 | 日本 | 1100/911/132 | >0.4 | >4 | 36 | 67 | 73 | 心脏事件 全因死亡 | 年龄,性别,体重指数,收缩压,心率,NYHA分级,是否有缺血性因素,高血压、糖尿病、慢性肾脏病,贫血,心房颤动,吸烟史,钠离子,C反应蛋白,BNP,左室射血分数 |
| Kannan等[ | 2018 | 美国 | 1365/1006/74 | >0.45 | >4.51 | 50 | 56.6 | 65 | 心脏事件 全因死亡 | 年龄,性别,种族,体重指数,缺血性病因,胺碘酮的使用,甲状腺药物使用 |
| Frey等[ | 2013 | 德国 | 758/628/34 | >0.3 | >4.0 | 37 | 68 | 71 | 全因死亡 | 年龄 |
| Wang等[ | 2015 | 中国 | 458/353/41 | >0.55 | >4.78 | 17 | 51 | 71 | 住院率 心脏事件 全因死亡 | 年龄,性别,贫血,肾脏功能障碍,高脂血症,吸烟,糖尿病 |
| Li等[ | 2014 | 中国 | 963/816/79 | >0.35 | >5.5 | 42 | 52.1 | 73.7 | 全因死亡 | 年龄,性别,高血压史,心房颤动,室性心动过速,饮酒吸烟,左室直径,左房直径,左室射血分数,FT3,T3,T4,亚临床甲亢,亚临床甲减 |
| 刘凯等[ | 2019 | 中国 | 1100/911/132 | >0.4 | >4 | 36.6 | 71.3 | 55.8 | 心脏事件 全因死亡 | 年龄、性别、体重指数、收缩压,心率,NYHA分级,缺血性心脏病,高血压,糖尿病,血脂水平,慢性肾病,贫血,心房颤动,吸烟史,血钠,C-反应蛋白、BNP和左室射血分数 |
| Rhee等[ | 2013 | 美国 | 15570/14130/691 | >0.39 | >4.6 | 429 | 46.7 | 46.5 | 全因死亡 | 年龄,性别,种族,糖尿病,吸烟,高血压,高胆固醇血症,BMI,既往脑卒中,心肌梗死 |
| Shuichi等[ | 2015 | 日本 | 71/61/8 | >0.35 | >5.5 | 无 | 无 | 无 | 住院率 | 无 |
| 作者 | 暴露组代表性 | 非暴露组代表性 | 暴露因素确定 | 研究时没有要观察的结局指标 | 是否控制混杂因素 | 盲法独立 | 随访时间是否足够长 | 随访完整性 | 总分(分) |
|---|---|---|---|---|---|---|---|---|---|
| Iacoviello等[ | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Sato等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Kannan等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Frey等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Wang等[ | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Li等[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| 刘凯等[ | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7 |
| Rhee等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Shuichi等[ | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 5 |
| 作者 | 暴露组代表性 | 非暴露组代表性 | 暴露因素确定 | 研究时没有要观察的结局指标 | 是否控制混杂因素 | 盲法独立 | 随访时间是否足够长 | 随访完整性 | 总分(分) |
|---|---|---|---|---|---|---|---|---|---|
| Iacoviello等[ | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Sato等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Kannan等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Frey等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Wang等[ | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Li等[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| 刘凯等[ | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7 |
| Rhee等[ | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Shuichi等[ | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 5 |
| 亚组 | 全因死亡 | 心脏事件和(或)再住院 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 文章数量 | 异质性检验 | Meta分析 | 文章数量 | 异质性检验 | Meta分析 | ||||||||
| I2(%) | P | HR | 95%CI | I2(%) | P | HR | 95%CI | ||||||
| 种族 | |||||||||||||
| 欧美洲 | 4 | 2.7 | 0.379 | 1.59 | 1.29-1.97 | 2 | 86.5 | 0.006 | 1.11 | 1.06-1.15 | |||
| 亚洲 | 4 | 66.6 | 0.029 | 1.56 | 1.28-1.90 | 3 | 60.3 | 0.081 | 1.59 | 1.29-1.96 | |||
| 年龄 | |||||||||||||
| ≤65岁 | 5 | 54.4 | 0.076 | 1.74 | 1.44-2.10 | 3 | 89.6 | 0.000 | 1.11 | 1.07-1.16 | |||
| >65岁 | 3 | 0 | 0.703 | 1.37 | 1.09-1.71 | 2 | 0 | 0.976 | 1.42 | 1.13-1.79 | |||
| 随访时间 | |||||||||||||
| ≤24月 | 2 | 0 | 0.347 | 2.50 | 1.76-3.56 | 2 | 91.7 | 0.001 | 1.11 | 1.06-1.15 | |||
| >24月 | 6 | 0 | 0.637 | 1.44 | 1.23-1.69 | 3 | 0 | 0.532 | 1.53 | 1.26-1.86 | |||
| 样本量 | |||||||||||||
| ≤1 000例 | 4 | 70.4 | 0.017 | 1.73 | 1.33-2.24 | 2 | 91.7 | 0.001 | 1.11 | 1.06-1.15 | |||
| >1 000例 | 4 | 0 | 0.729 | 1.52 | 1.28-1.80 | 3 | 0 | 0.532 | 1.53 | 1.26-1.86 | |||
| 亚组 | 全因死亡 | 心脏事件和(或)再住院 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 文章数量 | 异质性检验 | Meta分析 | 文章数量 | 异质性检验 | Meta分析 | ||||||||
| I2(%) | P | HR | 95%CI | I2(%) | P | HR | 95%CI | ||||||
| 种族 | |||||||||||||
| 欧美洲 | 4 | 2.7 | 0.379 | 1.59 | 1.29-1.97 | 2 | 86.5 | 0.006 | 1.11 | 1.06-1.15 | |||
| 亚洲 | 4 | 66.6 | 0.029 | 1.56 | 1.28-1.90 | 3 | 60.3 | 0.081 | 1.59 | 1.29-1.96 | |||
| 年龄 | |||||||||||||
| ≤65岁 | 5 | 54.4 | 0.076 | 1.74 | 1.44-2.10 | 3 | 89.6 | 0.000 | 1.11 | 1.07-1.16 | |||
| >65岁 | 3 | 0 | 0.703 | 1.37 | 1.09-1.71 | 2 | 0 | 0.976 | 1.42 | 1.13-1.79 | |||
| 随访时间 | |||||||||||||
| ≤24月 | 2 | 0 | 0.347 | 2.50 | 1.76-3.56 | 2 | 91.7 | 0.001 | 1.11 | 1.06-1.15 | |||
| >24月 | 6 | 0 | 0.637 | 1.44 | 1.23-1.69 | 3 | 0 | 0.532 | 1.53 | 1.26-1.86 | |||
| 样本量 | |||||||||||||
| ≤1 000例 | 4 | 70.4 | 0.017 | 1.73 | 1.33-2.24 | 2 | 91.7 | 0.001 | 1.11 | 1.06-1.15 | |||
| >1 000例 | 4 | 0 | 0.729 | 1.52 | 1.28-1.80 | 3 | 0 | 0.532 | 1.53 | 1.26-1.86 | |||
| [1] | Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart failure society of America[J]. Circulation, 2017, 136(6):e137-e161. |
| [2] |
Ning N, Gao D, Triggiani V, et al. Prognostic role of hypothyroidism in heart failure: A meta-analysis[J]. Medicine (Baltimore), 2015, 94(30):e1159.
doi: 10.1097/MD.0000000000001159 URL |
| [3] |
Bielecka-Dabrowa A, Godoy B, Suzuki T, et al. Subclinical hypothyroidism and the development of heart failure: An overview of risk and effects on cardiac function[J]. Clin Res Cardiol, 2019, 108(3):225-233.
doi: 10.1007/s00392-018-1340-1 pmid: 30091084 |
| [4] | 杨宜恒, 郑振中. 亚临床甲状腺功能减退对心力衰竭患者预后影响的Meta分析[J]. 实用心脑肺血管病杂志, 2021, 29(5):70-74. |
| [5] |
Yang G, Wang Y, Ma A, et al. Subclinical thyroid dysfunction is associated with adverse prognosis in heart failure patients with reduced ejection fraction[J]. BMC Cardiovasc Disord, 2019, 19(1):83.
doi: 10.1186/s12872-019-1055-x URL |
| [6] |
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9):603-605.
doi: 10.1007/s10654-010-9491-z pmid: 20652370 |
| [7] |
Iacoviello M, Guida P, Guastamacchia E, et al. Prognostic role of sub-clinical hypothyroidism in chronic heart failure outpatients[J]. Curr Pharm Des, 2008, 14(26):2686-2692.
doi: 10.2174/138161208786264142 URL |
| [8] |
Sato Y, Yoshihisa A, Kimishima Y, et al. Subclinical hypothyroidism is associated with adverse prognosis in heart failure patients[J]. Can J Cardiol, 2018, 34(1):80-87.
doi: S0828-282X(17)31110-8 pmid: 29275887 |
| [9] |
Kannan L, Shaw PA, Morley MP, et al. Thyroid dysfunction in heart failure and cardiovascular outcomes[J]. Circ Heart Fail, 2018, 11(12):e005266.
doi: 10.1161/CIRCHEARTFAILURE.118.005266 URL |
| [10] |
Frey A, Kroiss M, Berliner D, et al. Prognostic impact of subclinical thyroid dysfunction in heart failure[J]. Int J Cardiol, 2013, 168(1):300-305.
doi: 10.1016/j.ijcard.2012.09.064 pmid: 23041000 |
| [11] |
Wang W, Guan H, Gerdes AM, et al. Thyroid status, cardiac function, and mortality in patients with idiopathic dilated cardiomyopathy[J]. J ClinEndocrinol Metab, 2015, 100(8):3210-3218.
doi: 10.1210/jc.2014-4159 URL |
| [12] |
Li X, Yang X, Wang Y, et al. The prevalence and prognostic effects of subclinical thyroid dysfunction in dilated cardiomyopathy patients: A single-center cohort study[J]. J Card Fail, 2014, 20(7):506-512.
doi: 10.1016/j.cardfail.2014.05.002 pmid: 24858054 |
| [13] | 刘凯, 陈英, 郑杨, 等. 亚临床甲状腺功能减退对老年心力衰竭病人预后的影响[J]. 实用老年医学, 2019, 33(11):1108-1112. |
| [14] |
Rhee CM, Curhan GC, Alexander EK, et al. Subclinical hypothyroidism and survival: The effects of heart failure and race[J]. J Clin Endocrinol Metab, 2013, 98(6):2326-2336.
doi: 10.1210/jc.2013-1039 pmid: 23720788 |
| [15] | Shuichi K, Shohei K, Hiroo S, et al. Subclinical hypothyroidism is a useful predictor of adverse events in heart failure patients with reduced left ventricular ejection fraction[J]. J CARD FAIL, 2015, 21(10):S187. |
| [16] |
Tunbridge WM, Evered DC, Hall R, et al. The spectrum of thyroid disease in a community: The Whickham survey[J]. Clin Endocrinol (Oxf), 1977, 7(6):481-493.
doi: 10.1111/j.1365-2265.1977.tb01340.x URL |
| [17] |
Canaris GJ, Manowitz NR, Mayor G, et al. The Colorado thyroid disease prevalence study[J]. Arch Intern Med, 2000, 160(4):526-534.
doi: 10.1001/archinte.160.4.526 pmid: 10695693 |
| [18] |
Kannan L, Shaw PA, Morley MP, et al. Thyroid dysfunction in heart failure and cardiovascular outcomes[J]. Circ Heart Fail, 2018, 11(12):e005266.
doi: 10.1161/CIRCHEARTFAILURE.118.005266 URL |
| [19] |
Lam CS, Lyass A, Kraigher-Krainer E, et al. Cardiac dysfunction and noncardiac dysfunction as precursors of heart failure with reduced and preserved ejection fraction in the community[J]. Circulation, 2011, 124(1):24-30.
doi: 10.1161/CIRCULATIONAHA.110.979203 pmid: 21670229 |
| [20] |
Biondi B. Mechanisms in endocrinology: Heart failure and thyroid dysfunction[J]. Eur J Endocrinol, 2012, 167(5):609-618.
doi: 10.1530/EJE-12-0627 pmid: 22956554 |
| [21] |
Martínez-Sellés M, García Robles JA, Prieto L, et al. Hospitalized congestive heart failure patients with preserved versus abnormal left ventricular systolic function[J]. Rev Esp Cardiol, 2002, 55(6):579-586.
pmid: 12113716 |
| [22] |
Ilic S, Tadic M, Ivanovic B, et al. Left and right ventricular structure and function in subclinical hypothyroidism: The effects of one-year levothyroxine treatment[J]. Med Sci Monit, 2013, 19:960-968.
doi: 10.12659/MSM.889621 URL |
| [23] |
Tadic M, Ilic S, Kostic N, et al. Subclinical hypothyroidism and left ventricular mechanics: A three-dimensional speckle tracking study[J]. J Clin Endocrinol Metab, 2014, 99(1):307-314.
doi: 10.1210/jc.2013-3107 pmid: 24187401 |
| [24] |
Mousa S, Hemeda A, Ghorab H, et al. Arterial wall stiffness and the risk of atherosclerosis in egyptian patients with overt and subclinical hypothyroidism[J]. Endocr Pract, 2020, 26(2):161-166.
doi: 10.4158/EP-2019-0322 pmid: 31557076 |
| [25] |
Saif A, Mousa S, Assem M, et al. Endothelial dysfunction and the risk of atherosclerosis in overt and subclinical hypothyroidism[J]. Endocr Connect, 2018, 7(10):1075-1080.
doi: 10.1530/EC-18-0194 pmid: 30352390 |
| [26] | Swaid B, Kheiri B, Sundus S, et al. The effect of levothyroxine treatment in individuals with subclinical hypothyroidism on surrogate markers of atherosclerosis: A meta-analysis of randomized controlled trials[J]. J Community Hosp Intern Med Perspect, 2019, 9(4):305-309. |
| [27] |
Sengupta S, Jaseem T, Ambalavanan J, et al. Homeostatic model assessment-insulin resistance (HOMA-IR 2) in mild subclinical hypothyroid subjects[J]. Indian J Clin Biochem, 2018, 33:214-217.
doi: 10.1007/s12291-017-0647-4 URL |
| [28] | Treister-Goltzman Y, Yarza S, Peleg R. Lipid profile in mild subclinical hypothyroidism: Systematic review and meta-analysis[J]. Minerva Endocrinol (Torino), 2021, 46(4):428-440. |
| [29] |
Hueston WJ, Pearson WS. Subclinical hypothyroidism and the risk of hypercholesterolemia[J]. Ann Fam Med, 2004, 2(4):351-355.
pmid: 15335135 |
| [30] |
Jayasingh IA, Puthuran P. Subclinical hypothyroidism and the risk of hypercholesterolemia[J]. J Family Med Prim Care, 2016, 5(4):809-816.
doi: 10.4103/2249-4863.201177 pmid: 28348996 |
| [31] |
Papadopoulou AM, Bakogiannis N, Skrapari I, et al. Thyroid dysfunction and atherosclerosis: A systematic review[J]. In Vivo, 2020, 34(6):3127-3136.
doi: 10.21873/invivo.12147 pmid: 33144416 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||