Clinical Focus ›› 2025, Vol. 40 ›› Issue (1): 14-20.doi: 10.3969/j.issn.1004-583X.2025.01.002
Previous Articles Next Articles
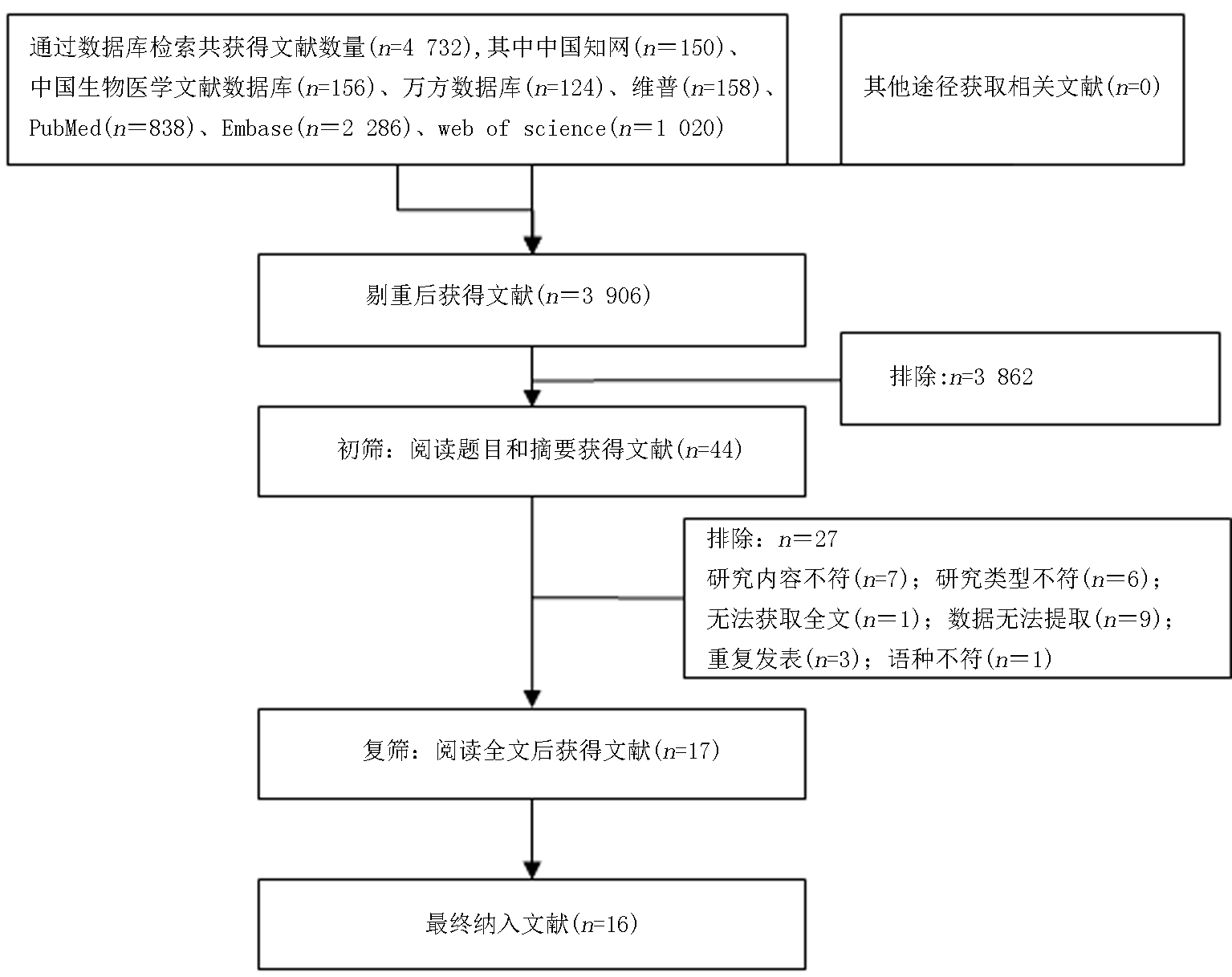
Epidemiological characteristics of hospital-acquired infections in pediatric patients supported by extracorporeal membrane oxygenation: A meta-analysis
Wang Ying1a, Zhong Bohua1a( ), Wang Lifang1b, Lang Qiuyan1a, Luo Haibin1a, Wang Shulin1a, Li Chunpeng2, Liao Min3
), Wang Lifang1b, Lang Qiuyan1a, Luo Haibin1a, Wang Shulin1a, Li Chunpeng2, Liao Min3
- 1a. No.1 Critical Care Unit; b. Pediatric Intensive Care Unit, the First Affiliated Hospital of Guangxi Medical University,Nanning 530021,China
2. No.5 Critical Care Unit,Henan Provincial People's Hospital, Zhengzhou 450000,China
3. Department of Emergency,the First Affiliated Hospital of Guangxi University of Chinese Medicine,Nanning 530023,China
-
Received:2024-10-08Online:2025-01-20Published:2025-01-17 -
Contact:Zhong Bohua,Email: 2601924118@qq.com
CLC Number:
Cite this article
Wang Ying, Zhong Bohua, Wang Lifang, Lang Qiuyan, Luo Haibin, Wang Shulin, Li Chunpeng, Liao Min. Epidemiological characteristics of hospital-acquired infections in pediatric patients supported by extracorporeal membrane oxygenation: A meta-analysis[J]. Clinical Focus, 2025, 40(1): 14-20.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2025.01.002
| #1 | adolescent* |
|---|---|
| #2 | child* |
| #3 | infant* |
| #4 | pediatric* |
| #5 | new born* |
| #6 | babi* |
| #7 | youth* |
| #8 | teen* |
| #9 | toddler* |
| #10 | preschool* |
| #11 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 |
| #12 | Extracorporeal Membrane Oxygenation |
| #13 | ECMO |
| #14 | Heart-Lung Machine |
| #15 | #11 OR #12 OR #13 |
| #16 | cross infection |
| #17 | infect* |
| #18 | #16 OR #17 |
| #19 | #11 OR #15 OR #18 |
| #1 | adolescent* |
|---|---|
| #2 | child* |
| #3 | infant* |
| #4 | pediatric* |
| #5 | new born* |
| #6 | babi* |
| #7 | youth* |
| #8 | teen* |
| #9 | toddler* |
| #10 | preschool* |
| #11 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 |
| #12 | Extracorporeal Membrane Oxygenation |
| #13 | ECMO |
| #14 | Heart-Lung Machine |
| #15 | #11 OR #12 OR #13 |
| #16 | cross infection |
| #17 | infect* |
| #18 | #16 OR #17 |
| #19 | #11 OR #15 OR #18 |
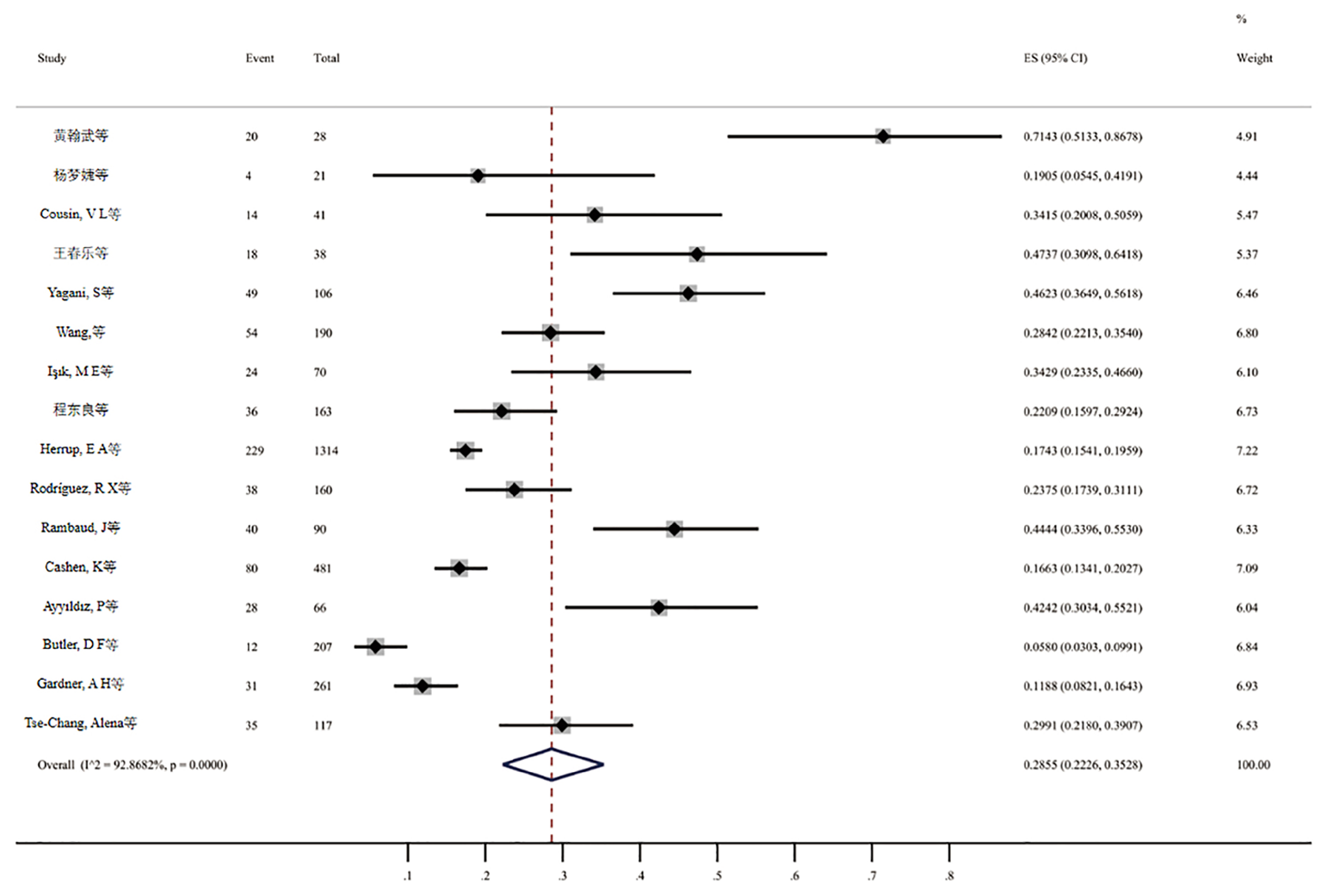
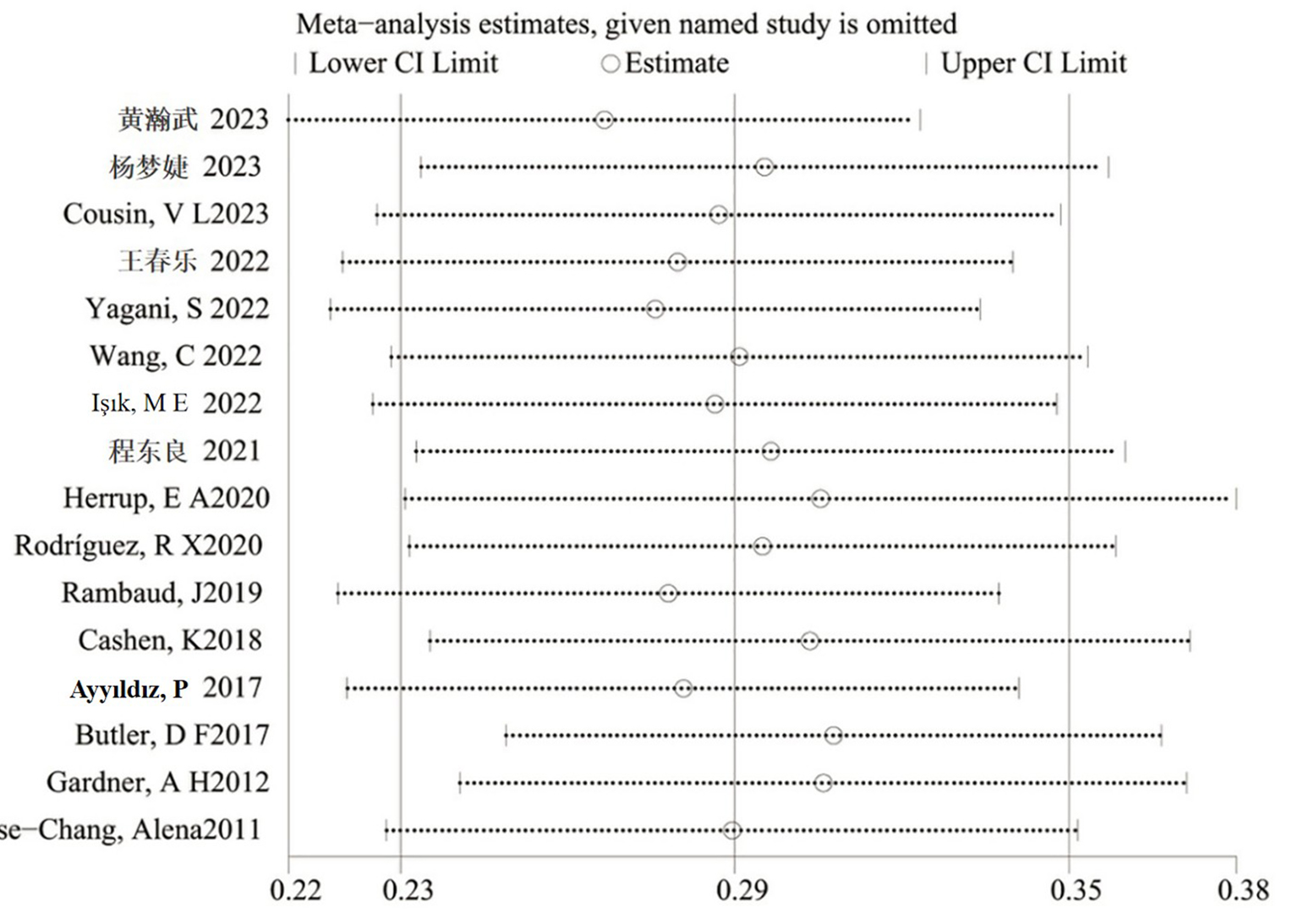
| 纳入研究 | 发表时间 | 国家/组织 | 研究类型 | 研究时限 | 样本量 | 感染组 (例) | 非感染组 (例) | 文献质量评分 (分) |
|---|---|---|---|---|---|---|---|---|
| 黄翰武等[ | 2023 | 中国 | 回顾性 | 2019.01-2023.06 | 28 | 20 | 8 | |
| 杨梦婕等[ | 2023 | 中国 | 回顾性 | 2017.12-2021.11 | 21 | 4 | 17 | |
| Cousin等[ | 2023 | 瑞士 | 回顾性 | 2008.01-2014.12 | 41 | 14 | 27 | |
| 王春乐等[ | 2022 | 中国 | 回顾性 | 2015.07- 2021.03 | 38 | 18 | 20 | |
| Işık等[ | 2022 | 土耳其 | 回顾性 | 2010.01-2020.12 | 70 | 24 | 46 | |
| Wang等[ | 2022 | 中国 | 回顾性 | 2012.09-2019.12 | 190 | 54 | 136 | |
| Yagani等[ | 2022 | 印度 | 回顾性 | 2016.01-2020.12 | 106 | 49 | 57 | |
| 程东良等[ | 2021 | 中国 | 回顾性 | 2012.09-2020.02 | 163 | 36 | 127 | |
| Rodríguez等[ | 2020 | 智利 | 回顾性 | 2003.01-2016.12 | 160 | 38 | 122 | |
| Herrup等[ | 2020 | 美国 | 回顾性 | 2013.01-2015.12 | 1 314 | 229 | 1 085 | |
| Rambaud等[ | 2019 | 法国 | 回顾性 | 2010.01-2015.06 | 90 | 40 | 50 | |
| Cashen等[ | 2018 | 美国 | 前瞻性 | 2012.12-2014.09 | 481 | 80 | 401 | |
| Ayyıldız等[ | 2017 | 土耳其 | 回顾性 | 2011.01-2014.06 | 66 | 28 | 38 | |
| Butler等[ | 2017 | 美国 | 回顾性 | 2018.01-2013.10 | 207 | 12 | 195 | |
| Gardner等[ | 2012 | 美国 | 回顾性 | 1989.01-2008.12 | 261 | 31 | 230 | |
| Tse-Chang等[ | 2011 | 加拿大 | 回顾性 | 1997.05-2007.05 | 117 | 35 | 82 |
Tab.1 Basic characteristics and quality assessment of included literatures
| 纳入研究 | 发表时间 | 国家/组织 | 研究类型 | 研究时限 | 样本量 | 感染组 (例) | 非感染组 (例) | 文献质量评分 (分) |
|---|---|---|---|---|---|---|---|---|
| 黄翰武等[ | 2023 | 中国 | 回顾性 | 2019.01-2023.06 | 28 | 20 | 8 | |
| 杨梦婕等[ | 2023 | 中国 | 回顾性 | 2017.12-2021.11 | 21 | 4 | 17 | |
| Cousin等[ | 2023 | 瑞士 | 回顾性 | 2008.01-2014.12 | 41 | 14 | 27 | |
| 王春乐等[ | 2022 | 中国 | 回顾性 | 2015.07- 2021.03 | 38 | 18 | 20 | |
| Işık等[ | 2022 | 土耳其 | 回顾性 | 2010.01-2020.12 | 70 | 24 | 46 | |
| Wang等[ | 2022 | 中国 | 回顾性 | 2012.09-2019.12 | 190 | 54 | 136 | |
| Yagani等[ | 2022 | 印度 | 回顾性 | 2016.01-2020.12 | 106 | 49 | 57 | |
| 程东良等[ | 2021 | 中国 | 回顾性 | 2012.09-2020.02 | 163 | 36 | 127 | |
| Rodríguez等[ | 2020 | 智利 | 回顾性 | 2003.01-2016.12 | 160 | 38 | 122 | |
| Herrup等[ | 2020 | 美国 | 回顾性 | 2013.01-2015.12 | 1 314 | 229 | 1 085 | |
| Rambaud等[ | 2019 | 法国 | 回顾性 | 2010.01-2015.06 | 90 | 40 | 50 | |
| Cashen等[ | 2018 | 美国 | 前瞻性 | 2012.12-2014.09 | 481 | 80 | 401 | |
| Ayyıldız等[ | 2017 | 土耳其 | 回顾性 | 2011.01-2014.06 | 66 | 28 | 38 | |
| Butler等[ | 2017 | 美国 | 回顾性 | 2018.01-2013.10 | 207 | 12 | 195 | |
| Gardner等[ | 2012 | 美国 | 回顾性 | 1989.01-2008.12 | 261 | 31 | 230 | |
| Tse-Chang等[ | 2011 | 加拿大 | 回顾性 | 1997.05-2007.05 | 117 | 35 | 82 |
| 病原体分类 | 病原微生物 | 例数 | 构成比(%) |
|---|---|---|---|
| 革兰阳性菌 | 106 | 22.13 | |
| 凝固酶阴性葡萄球菌 | 9 | 1.88 | |
| 金黄色葡萄球菌 | 31 | 6.47 | |
| 白色念珠菌 | 30 | 6.26 | |
| 表皮葡萄球菌 | 18 | 3.76 | |
| 肺炎链球菌 | 7 | 1.46 | |
| 粪肠球菌 | 6 | 1.25 | |
| 链球菌 | 1 | 0.21 | |
| 沃氏葡萄球菌 | 2 | 0.42 | |
| 缓症链球菌 | 1 | 0.21 | |
| 芽孢杆菌 | 1 | 0.21 | |
| 革兰阴性菌 | 329 | 68.68 | |
| 鲍曼不动杆菌 | 129 | 26.93 | |
| 铜绿假单胞菌 | 45 | 9.39 | |
| 肺炎克雷伯菌 | 57 | 11.90 | |
| 大肠杆菌 | 37 | 7.72 | |
| 嗜麦芽窄单食胞菌 | 26 | 5.43 | |
| 洋葱伯克霍尔德氏菌 | 8 | 1.67 | |
| 少动假单胞菌 | 5 | 1.04 | |
| 沙雷菌 | 5 | 1.04 | |
| 流感嗜血杆菌 | 4 | 0.84 | |
| 阴沟肠杆菌 | 3 | 0.63 | |
| 支原体 | 2 | 0.42 | |
| 皮氏霍尔德氏菌 | 2 | 0.42 | |
| 大肠埃希菌 | 2 | 0.42 | |
| 嗜肺军团菌 | 1 | 0.21 | |
| 产酸克雷伯氏菌 | 1 | 0.21 | |
| 雷氏普罗威登斯菌 | 1 | 0.21 | |
| 产气肠杆菌 | 1 | 0.21 | |
| 病毒 | 24 | 5.01 | |
| 流感病毒 | 8 | 1.67 | |
| 腺病毒 | 7 | 1.46 | |
| 巨细胞病毒 | 6 | 1.25 | |
| EB病毒 | 1 | 0.21 | |
| 呼吸道合胞病毒 | 1 | 0.21 | |
| 禽流感病毒 | 1 | 0.21 | |
| 真菌 | 20 | 4.18 | |
| 假丝酵母菌 | 15 | 3.13 | |
| 近平滑念珠菌 | 3 | 0.63 | |
| 耶氏肺孢子菌 | 2 | 0.42 | |
| 其他 | 6 | 1.25 |
Tab.2 Etiology distribution
| 病原体分类 | 病原微生物 | 例数 | 构成比(%) |
|---|---|---|---|
| 革兰阳性菌 | 106 | 22.13 | |
| 凝固酶阴性葡萄球菌 | 9 | 1.88 | |
| 金黄色葡萄球菌 | 31 | 6.47 | |
| 白色念珠菌 | 30 | 6.26 | |
| 表皮葡萄球菌 | 18 | 3.76 | |
| 肺炎链球菌 | 7 | 1.46 | |
| 粪肠球菌 | 6 | 1.25 | |
| 链球菌 | 1 | 0.21 | |
| 沃氏葡萄球菌 | 2 | 0.42 | |
| 缓症链球菌 | 1 | 0.21 | |
| 芽孢杆菌 | 1 | 0.21 | |
| 革兰阴性菌 | 329 | 68.68 | |
| 鲍曼不动杆菌 | 129 | 26.93 | |
| 铜绿假单胞菌 | 45 | 9.39 | |
| 肺炎克雷伯菌 | 57 | 11.90 | |
| 大肠杆菌 | 37 | 7.72 | |
| 嗜麦芽窄单食胞菌 | 26 | 5.43 | |
| 洋葱伯克霍尔德氏菌 | 8 | 1.67 | |
| 少动假单胞菌 | 5 | 1.04 | |
| 沙雷菌 | 5 | 1.04 | |
| 流感嗜血杆菌 | 4 | 0.84 | |
| 阴沟肠杆菌 | 3 | 0.63 | |
| 支原体 | 2 | 0.42 | |
| 皮氏霍尔德氏菌 | 2 | 0.42 | |
| 大肠埃希菌 | 2 | 0.42 | |
| 嗜肺军团菌 | 1 | 0.21 | |
| 产酸克雷伯氏菌 | 1 | 0.21 | |
| 雷氏普罗威登斯菌 | 1 | 0.21 | |
| 产气肠杆菌 | 1 | 0.21 | |
| 病毒 | 24 | 5.01 | |
| 流感病毒 | 8 | 1.67 | |
| 腺病毒 | 7 | 1.46 | |
| 巨细胞病毒 | 6 | 1.25 | |
| EB病毒 | 1 | 0.21 | |
| 呼吸道合胞病毒 | 1 | 0.21 | |
| 禽流感病毒 | 1 | 0.21 | |
| 真菌 | 20 | 4.18 | |
| 假丝酵母菌 | 15 | 3.13 | |
| 近平滑念珠菌 | 3 | 0.63 | |
| 耶氏肺孢子菌 | 2 | 0.42 | |
| 其他 | 6 | 1.25 |
| [1] | 隋明亮, 汤卫兵, 吴长江, 等. 体外膜肺氧合在院内成人心源性休克和心脏骤停中的应用研究[J]. 上海交通大学学报(医学版), 2023, 43(12): 1529-1534. |
| [2] | 刘亮, 张洪鑫, 高恒波, 等. 体外膜肺氧合在急性中毒中的应用进展[J]. 华西医学, 2023, 38(11): 1742-1747. |
| [3] | 王宋, 刘敏, 许红阳. 体外膜肺氧合在肺移植手术中的应用进展[J]. 临床麻醉学杂志, 2023, 39(8): 863-867. |
| [4] | 国家心血管病医疗质量控制中心专家委员会体外循环与体外生命支持专家工作组. 2021年中国体外生命支持医疗质量控制报告[J]. 中国循环杂志, 2022, 37(12): 1195-1201. |
| [5] | 杜彦强, 王义, 洪小杨. 体外膜肺氧合技术在儿科急性呼吸衰竭中的应用进展[J]. 中国临床新医学, 2023, 16(7): 651-655. |
| [6] | 程东良, 史长松. 体外膜肺氧合在儿童脓毒症休克中的临床应用[J]. 中国临床新医学, 2023, 16(7): 673-677. |
| [7] |
Bhatt P, Lekshminarayanan A, Donda K, et al. National trends in neonatal extracorporeal membrane oxygenation in the United States[J]. J Perinatol, 2018, 38(8): 1106-1113.
doi: 10.1038/s41372-018-0129-4 pmid: 29795325 |
| [8] | 罗建宇, 吕光宇, 刘美琼, 等. 体外膜肺氧合并发症发生情况及影响患者预后的因素分析[J]. 广西医学, 2022, 44(7): 700-705. |
| [9] | Pena-Lopez Y, Machado MC, Rello J. Infection in ECMO patients: Changes in epidemiology, diagnosis and prevention[J]. Anaesth Crit Care Pain Med, 2024, 43(1): 101319. |
| [10] | 郭君妍, 麻旭州, 徐鹏飞, 等. 抗凝治疗在体外膜肺氧合中的应用现状与挑战[J]. 血栓与止血学, 2024, 30(2): 89-94. |
| [11] | Thongprayoon C, Cheungpasitporn W, Lertjitbanjong P, et al. Incidence and impact of acute kidney injury in patients receiving extracorporeal membrane oxygenation: A meta-analysis[J]. J Clin Med, 2019, 8(7):981. |
| [12] | Li X, Wang L, Wang H, et al. Outcome and clinical characteristics of nosocomial infection in adult patients undergoing extracorporeal membrane oxygenation: A systematic review and meta-analysis[J]. Front Public Health, 2022, 10: 857873. |
| [13] | 周成斌, 郭予雄, 胡燕. 中国儿科体外膜肺氧合技术的发展现状[J]. 中国临床新医学, 2021, 14(5): 427-431. |
| [14] | 曾宪涛, 刘慧, 陈曦, 等. Meta分析系列之四:观察性研究的质量评价工具[J]. 中国循证心血管医学杂志, 2012, 4(4): 297-299. |
| [15] | Wells GA, Shea BJ, O'Connell D, et al. The newcastle-ottawa scale (NOS) for assessing the quality of non-randomized studies in meta-analysis[J]. Appl Eng Agric, 2002, 18(6): 727-734. |
| [16] | 黄翰武, 梁珍花, 王敏, 等. 急性呼吸衰竭ECMO支持患儿病原学及临床因素对结局的影响分析[J]. 中国临床新医学, 2023, 16(7): 678-683. |
| [17] | 杨梦婕, 黄红娟, 沈啸威, 等. 儿童心胸重症监护室接受体外膜肺氧合治疗患儿的抗感染治疗情况分析[J]. 药学与临床研究, 2023, 31(4): 352-355. |
| [18] |
Cousin VL, Rodriguez-Vigouroux R, Karam O, et al. First nosocomial infections in children supported by veno-arterial extracorporeal membrane oxygenation (VA-ECMO)[J]. BMC Pediatr, 2023, 23(1): 89.
doi: 10.1186/s12887-023-03908-3 pmid: 36823601 |
| [19] | 王春乐, 刘福荣, 杨进福, 等. 儿童心脏术后静脉-动脉体外膜肺氧合相关医院内感染的危险因素[J]. 中南大学学报(医学版), 2022, 47(6): 748-754. |
| [20] | Işık ME, Arslanoˇglu E, Menekşe Ş, et al. Infection profile of patients with extracorporeal membrane oxygenation in paediatric cardiac surgery ICU[J]. Cardiol Young, 2022, 32(11): 1833-1838. |
| [21] | Wang C, Li S, Wang F, et al. Nosocomial infections during extracorporeal membrane oxygenation in pediatric patients: A multicenter retrospective study[J]. Front Pediatr, 2022, 10: 873577. |
| [22] | Yagani S, Singh SP, Sahu MK, et al. Infections acquired during venoarterial extracorporeal membrane oxygenation postcardiac surgery in children: A retrospective observational study[J]. J Cardiac Critical Care, 2022, 6(1): 25-32. |
| [23] | 程东良, 方柯南, 邢燕, 等. 儿科体外膜肺氧合期间院内感染调查分析[J]. 中华实用儿科临床杂志, 2021, 36(18): 1394-1397. |
| [24] | Rodríguez RX, Villarroel LA, Meza RA, et al. Infection profile in neonatal patients during extracorporeal membrane oxygenation[J]. Int J Artif Organs, 2020, 43(11): 719-725. |
| [25] | Herrup EA, Yuerek M, Griffis HM, et al. Hospital-acquired infection in pediatric subjects with congenital heart disease postcardiotomy supported on extracorporeal membrane oxygenation[J]. Pediatr Crit Care Med, 2020, 21(11): E1020-E1025. |
| [26] | Rambaud J, Allioux C, Jean S, et al. Nosocomial infections in neonates supported by extracorporeal membrane oxygenation: First French retrospective study[J]. Indian J Crit Care Med, 2019, 23(9): 392-395. |
| [27] |
Cashen K, Reeder R, Dalton HJ, et al. Acquired infection during neonatal and pediatric extracorporeal membrane oxygenation[J]. Perfusion, 2018, 33(6): 472-482.
doi: 10.1177/0267659118766436 pmid: 29638203 |
| [28] |
Ayyıldız P, Kasar T, Ozturk E, et al. The evaluation of nosocomial infections in pediatric patients with extracorporeal membrane oxygenation support[J]. Braz J Cardiovasc Surg, 2017, 32(6): 468-474.
doi: S0102-76382017000600468 pmid: 29267608 |
| [29] |
Butler DF, Lee B, Molitor-Kirsch E, et al. Extracorporeal membrane oxygenation-associated bloodstream infections in children[J]. Pediatr Infect Dis J, 2017, 36(3): 346-347.
doi: 10.1097/INF.0000000000001431 pmid: 27902647 |
| [30] |
Gardner AH, Prodhan P, Stovall SH, et al. Fungal infections and antifungal prophylaxis in pediatric cardiac extracorporeal life support[J]. J Thorac Cardiovasc Surg, 2012, 143(3): 689-695.
doi: 10.1016/j.jtcvs.2011.12.001 pmid: 22177096 |
| [31] | Tse-Chang A, Midodzi W, Joffe AR, et al. Infections in children receiving extracorporeal life support[J]. Infect Control Hosp Epidemiol, 2011, 32(2): 115-120. |
| [32] |
Lee EH, Lee KH, Lee SJ, et al. Clinical and microbiological characteristics of and risk factors for bloodstream infections among patients with extracorporeal membrane oxygenation: A single-center retrospective cohort study[J]. Sci Rep, 2022, 12(1): 15059.
doi: 10.1038/s41598-022-19405-z pmid: 36064957 |
| [33] |
Wang J, Wang L, Jia M, et al. Extracorporeal membrane oxygenation-related nosocomial infection after cardiac surgery in adult patients[J]. Braz J Cardiovasc Surg, 2021, 36(6): 743-751.
doi: 10.21470/1678-9741-2020-0068 pmid: 33577254 |
| [34] |
Li ZJ, Zhang DF, Zhang WH. Analysis of nosocomial infection and risk factors in patients with ECMO treatment[J]. Infect Drug Resist, 2021, 14: 2403-2410.
doi: 10.2147/IDR.S306209 pmid: 34211285 |
| [35] | Mornese Pinna S, Sousa Casasnovas I, Olmedo M, et al. Nosocomial infections in adult patients supported by extracorporeal membrane oxygenation in a cardiac intensive care unit[J]. Microorganisms, 2023, 11(4): 1079. |
| [36] |
Schmidt M, Bréchot N, Hariri S, et al. Nosocomial infections in adult cardiogenic shock patients supported by venoarterial extracorporeal membrane oxygenation[J]. Clin Infect Dis, 2012, 55(12): 1633-1641.
doi: 10.1093/cid/cis783 pmid: 22990851 |
| [37] | Kim HS, Park S, Ko HH, et al. Different characteristics of bloodstream infection during venoarterial and venovenous extracorporeal membrane oxygenation in adult patients[J]. Sci Rep, 2021, 11(1): 9410-9498. |
| [38] |
Yang L, Li M, Gu S, et al. Risk factors for bloodstream infection (BSI) in patients with severe acute respiratory distress syndrome (ARDS) supported by veno-venous extracorporeal membrane oxygenation (VV-ECMO)[J]. BMC Pulm Med, 2022, 22(1):370.
doi: 10.1186/s12890-022-02164-y pmid: 36171599 |
| [39] | Aubron C, Cheng AC, Pilcher D, et al. Infections acquired by adults who receive extracorporeal membrane oxygenation: Risk factors and outcome[J]. Infect Control Hosp Epidemiol, 2013, 34(1): 24-30. |
| [40] |
Kim GS, Lee KS, Park CK, et al. Nosocomial Infection in Adult Patients Undergoing Veno-Arterial Extracorporeal Membrane Oxygenation[J]. J Korean Med Sci, 2017, 32(4): 593-598.
doi: 10.3346/jkms.2017.32.4.593 pmid: 28244284 |
| [41] |
Juthani BK, Macfarlan J, Wu J, et al. Incidence of nosocomial infections in adult patients undergoing extracorporeal membrane oxygenation[J]. Heart Lung, 2018, 47(6): 626-630.
doi: S0147-9563(18)30162-6 pmid: 30166066 |
| [42] |
Xu W, Fu Y, Yao Y, et al. Nosocomial infections in nonsurgical patients undergoing extracorporeal membrane oxygenation: A retrospective analysis in a chinese hospital[J]. Infect Drug Resist, 2022, 15: 4117-4126.
doi: 10.2147/IDR.S372913 pmid: 35937786 |
| [43] |
Carelli S, Dell'Anna AM, Montini L, et al. Bloodstream infections in COVID-19 patients undergoing extracorporeal membrane oxygenation in ICU: An observational cohort study[J]. Heart Lung, 2023, 62: 193-199.
doi: 10.1016/j.hrtlng.2023.07.012 pmid: 37562337 |
| [44] |
Kim DW, Yeo HJ, Yoon SH, et al. Impact of bloodstream infections on catheter colonization during extracorporeal membrane oxygenation[J]. J Artif Organs, 2016, 19(2): 128-133.
doi: 10.1007/s10047-015-0882-5 pmid: 26721824 |
| [45] | Na SJ, Chung CR, Choi HJ, et al. Blood stream infection in patients on venovenous extracorporeal membrane oxygenation for respiratory failure[J]. Infect Control Hosp Epidemiol, 2018, 39(7): 871-874. |
| [46] | Wang J, Huang J, Hu W, et al. Bloodstream infections in patients undergoing extracorporeal membrane oxygenation[J]. Pak J Med Sci, 2020, 36(6): 1171-1176. |
| [47] |
Yun JH, Hong SB, Jung SH, et al. Epidemiology and clinical characteristics of bloodstream infection in patients under extracorporeal membranous oxygenation[J]. J Intensive Care Med, 2021, 36(9): 1053-1060.
doi: 10.1177/0885066620985538 pmid: 33375874 |
| [48] |
Wang L, Ni K, Wang Y, et al. Nosocomial infections in adult patients receiving extracorporeal membrane oxygenation in China: A retrospective cohort study[J]. Am J Infect Control, 2023, 51(11): 1237-1241.
doi: 10.1016/j.ajic.2023.04.010 pmid: 37059121 |
| [49] | Bizzarro MJ, Conrad SA, Kaufman DA, et al. Infections acquired during extracorporeal membrane oxygenation in neonates, children, and adults[J]. Pediatr Crit Care Med, 2011, 12(3): 277-281. |
| [50] | 姚雨菲, 孙海超, 胡艺. ICU病人多重耐药菌感染危险因素的Meta分析[J]. 循证护理, 2024, 10(15): 2673-2680. |
| [51] | 邹丽婷, 胡怡倩, 卞雯, 等. ICU多药耐药菌感染影响因素及其耐药基因[J]. 中华医院感染学杂志, 2022, 32(11): 1622-1626. |
| [52] | 骆一舟, 赵燕华, 张红钢. 冠心病患者肺部感染的相关因素分析[J]. 中华医院感染学杂志, 2014, 24(13): 3245-3247. |
| [53] | 田稳稳, 王鹏翔, 余卫明, 等. 重症监护室多重耐药菌医院感染的相关危险因素分析[J]. 中国当代医药, 2022, 29(24): 41-45. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||