Clinical Focus ›› 2024, Vol. 39 ›› Issue (2): 149-154.doi: 10.3969/j.issn.1004-583X.2024.02.010
Previous Articles Next Articles
Intracranial infection of varicella zoster virus in adults: Clinical analysis of 5 cases
Liu Wanqi1, Fan Shuqin2a, Zhuang Ruixue3, He Feng2b, Liu Zhenchuan2b, Xie Zhongxiang2b( )
)
- 1. Jinzhou Medical University, Jinzhou 121000, China
2. Department of Nursing; b.Department of Neurological Intensive Care Unit, Linyi People's Hospital, Linyi 276000, China
3. School of Clinical Medicine, Shandong Second Medical University, Weifang 261000, China
-
Received:2023-10-19Online:2024-02-20Published:2024-04-18 -
Contact:Xie Zhongxiang E-mail:xiezhongxiang8607@163.com
CLC Number:
Cite this article
Liu Wanqi, Fan Shuqin, Zhuang Ruixue, He Feng, Liu Zhenchuan, Xie Zhongxiang. Intracranial infection of varicella zoster virus in adults: Clinical analysis of 5 cases[J]. Clinical Focus, 2024, 39(2): 149-154.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.02.010
| 评分 | 描述 |
|---|---|
| 0 | 完全无症状 |
| 1 | 尽管有症状,但无明显功能障碍,能完成所有日常工作和生活 |
| 2 | 轻度残疾,不能完成病前所有活动,但不需帮助能照料自己的日常事务 |
| 3 | 中度残疾,需部分帮助,但能独立行走 |
| 4 | 中重度残疾,不能独立行走,日常生活需别人帮助 |
| 5 | 重度残疾,卧床,二便失禁,日常生活完全依赖他人 |
| 6 | 死亡 |
Tab.1 Modified Rankin Scale
| 评分 | 描述 |
|---|---|
| 0 | 完全无症状 |
| 1 | 尽管有症状,但无明显功能障碍,能完成所有日常工作和生活 |
| 2 | 轻度残疾,不能完成病前所有活动,但不需帮助能照料自己的日常事务 |
| 3 | 中度残疾,需部分帮助,但能独立行走 |
| 4 | 中重度残疾,不能独立行走,日常生活需别人帮助 |
| 5 | 重度残疾,卧床,二便失禁,日常生活完全依赖他人 |
| 6 | 死亡 |
| 一般临床资料 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 性别 | 男 | 女 | 女 | 男 | 男 |
| 年龄(岁) | 60 | 67 | 47 | 36 | 58 |
| 前驱感染 | + | + | + | + | + |
| 既往史 | - | - | 佝偻病史 | - | - |
| 居住环境 | - | - | 家中养猪、牛 | - | 家中养猪、牛 |
Tab.2 General clinical data of 5 patients with intracranial infection of VZV
| 一般临床资料 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 性别 | 男 | 女 | 女 | 男 | 男 |
| 年龄(岁) | 60 | 67 | 47 | 36 | 58 |
| 前驱感染 | + | + | + | + | + |
| 既往史 | - | - | 佝偻病史 | - | - |
| 居住环境 | - | - | 家中养猪、牛 | - | 家中养猪、牛 |
| 临床表现 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 发热最高体温 | 39.4℃ | 38.6℃ | 38.2℃ | 39.0℃ | 38.5℃ |
| 头痛 | + | + | + | + | + |
| 恶心、呕吐 | - | + | - | + | + |
| 颈部僵硬 | + | + | + | + | + |
| 皮肤带状疱疹 | - | - | - | - | + |
| 眼痛、眼睑下垂 | + | - | - | - | - |
| 精神状态改变 | - | + | - | - | - |
| 癫痫发作 | - | - | + | - | - |
| 视物模糊 | - | - | - | + | - |
| 肢体活动不灵 | - | + | + | - | - |
Tab.3 Clinical manifestations of 5 patients with intracranial infection of VZV
| 临床表现 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 发热最高体温 | 39.4℃ | 38.6℃ | 38.2℃ | 39.0℃ | 38.5℃ |
| 头痛 | + | + | + | + | + |
| 恶心、呕吐 | - | + | - | + | + |
| 颈部僵硬 | + | + | + | + | + |
| 皮肤带状疱疹 | - | - | - | - | + |
| 眼痛、眼睑下垂 | + | - | - | - | - |
| 精神状态改变 | - | + | - | - | - |
| 癫痫发作 | - | - | + | - | - |
| 视物模糊 | - | - | - | + | - |
| 肢体活动不灵 | - | + | + | - | - |
| 颅脑影像 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 检查方法 | MRA(含平扫)、MRI(强化)、SWI | CT | CT、MRA(平扫+强化) | CT、MRA(含平扫)、MRV | MRA(含平扫) |
| 病变特点 | MRA(含平扫):双侧额颞叶、双侧桥臂区、脑干区、左侧枕叶多发异常信号;MRI(强化):双侧额颞叶异常强化影;SWI未见明显异常 | - | CT:双侧颞叶、额叶低密度灶;MRA(平扫+强化):基底节区、丘脑、双侧额颞叶区、右侧岛叶、脑干区多发异常信号,双侧颞叶出血 | - | - |
Tab.4 Imaging findings of 5 patients with intracranial infection of VZV
| 颅脑影像 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 检查方法 | MRA(含平扫)、MRI(强化)、SWI | CT | CT、MRA(平扫+强化) | CT、MRA(含平扫)、MRV | MRA(含平扫) |
| 病变特点 | MRA(含平扫):双侧额颞叶、双侧桥臂区、脑干区、左侧枕叶多发异常信号;MRI(强化):双侧额颞叶异常强化影;SWI未见明显异常 | - | CT:双侧颞叶、额叶低密度灶;MRA(平扫+强化):基底节区、丘脑、双侧额颞叶区、右侧岛叶、脑干区多发异常信号,双侧颞叶出血 | - | - |
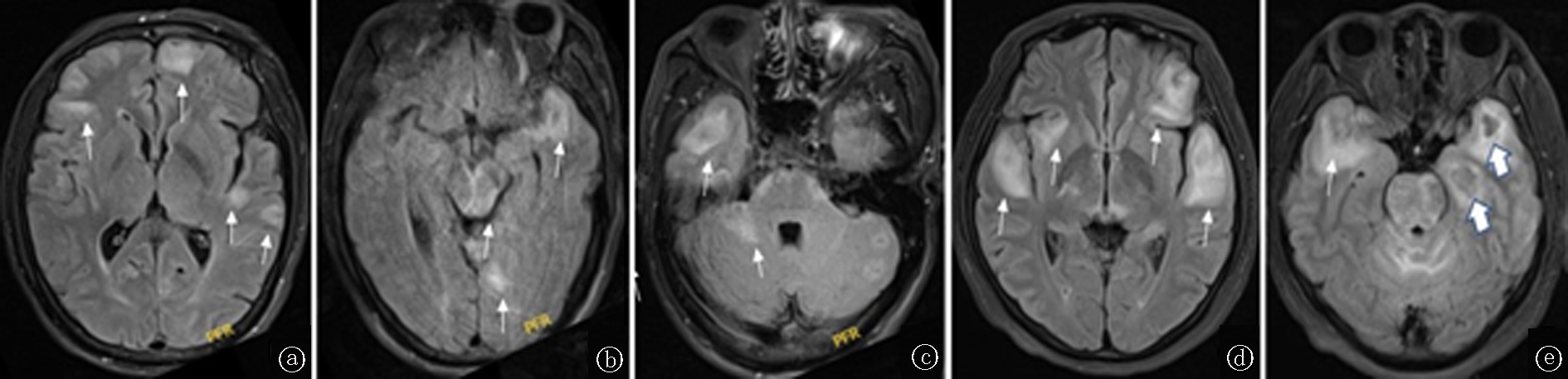
Fig.1 Magnetic resonance imaging of a patient with typical intracranial VZV infection a-c. Cranial T2 FLAIR sequences at different levels show multiple patchy high signals in bilateral frontotemporal lobe, bilateral pontine arm region, brainstem region, left occipital lobe, and cerebellum (example 1). d-e. Cranial T2 FLAIR sequences at different levels show multiple patchy high signals in basal ganglia, thalamus, bilateral frontotemporal lobe region, right insula, and brainstem region, of which the thick arrow on the e figure points to the hemorrhage in temporal lobe (example 3)
| 脑脊液 | 压力(mmHg) | 白细胞(×106/L) | 氯化物(mmol/L) | 蛋白定量(g/L) | 糖(mmol/L) | 脑脊液糖/血糖 |
|---|---|---|---|---|---|---|
| 例1 | 230 | 357 | 105.0 | 4.41 | 3.00 | 0.44 |
| 例2 | 140 | 473 | 98.9 | 1.74 | 4.22 | 0.63 |
| 例3 | 150 | 525 | 127.0 | 1.83 | 5.50 | 0.55 |
| 例4 | 225 | 312 | 118.7 | 1.72 | 3.24 | 0.56 |
| 例5 | 250 | 330 | 108.0 | 4.54 | 3.38 | 0.52 |
| 平均 | 199.00±44.99 | 399.40±84.20 | 111.52±10.05 | 2.85±1.33 | 3.91±1.01 | 0.54±0.06 |
Tab.5 CSF results in 5 patients with intracranial infection of VZV
| 脑脊液 | 压力(mmHg) | 白细胞(×106/L) | 氯化物(mmol/L) | 蛋白定量(g/L) | 糖(mmol/L) | 脑脊液糖/血糖 |
|---|---|---|---|---|---|---|
| 例1 | 230 | 357 | 105.0 | 4.41 | 3.00 | 0.44 |
| 例2 | 140 | 473 | 98.9 | 1.74 | 4.22 | 0.63 |
| 例3 | 150 | 525 | 127.0 | 1.83 | 5.50 | 0.55 |
| 例4 | 225 | 312 | 118.7 | 1.72 | 3.24 | 0.56 |
| 例5 | 250 | 330 | 108.0 | 4.54 | 3.38 | 0.52 |
| 平均 | 199.00±44.99 | 399.40±84.20 | 111.52±10.05 | 2.85±1.33 | 3.91±1.01 | 0.54±0.06 |
| 治疗及转归 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 入住ICU | + | + | + | - | - |
| 机械通气 | - | + | - | - | - |
| 抗病毒治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 |
| 免疫治疗 | 甲泼尼龙静脉治疗 | - | 甲泼尼龙静脉治疗 | - | - |
| 神经系统后遗症 | - | 认知功能减退及肢体瘫痪 | 肢体偏瘫 | - | - |
| 随访(发病3个月mRS评分) | 1 | 5 | 3 | 0 | 1 |
Tab.6 Treatment and outcome of 5 patients with intracranial infection of VZV
| 治疗及转归 | 例1 | 例2 | 例3 | 例4 | 例5 |
|---|---|---|---|---|---|
| 入住ICU | + | + | + | - | - |
| 机械通气 | - | + | - | - | - |
| 抗病毒治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 | 更昔洛韦静脉治疗 |
| 免疫治疗 | 甲泼尼龙静脉治疗 | - | 甲泼尼龙静脉治疗 | - | - |
| 神经系统后遗症 | - | 认知功能减退及肢体瘫痪 | 肢体偏瘫 | - | - |
| 随访(发病3个月mRS评分) | 1 | 5 | 3 | 0 | 1 |
| [1] | 中国初级卫生保健基金会病原检测专业委员会, 中国医疗保健国际交流促进会分子诊断学分会, 中国研究型医院学会神经科学专委会脑炎协作组. 病毒性脑(膜)炎病原体诊断技术应用专家共识[J]. 中华医学杂志, 2023, 103(9):648-657. |
| [2] | 关鸿志. 病毒性脑炎的诊治[J]. 中华神经科杂志, 2022, 55(7):747-754. |
| [3] | 中华医学会神经病学分会感染性疾病与脑脊液细胞学学组. 中枢神经系统感染性疾病的脑脊液宏基因组学第二代测序应用专家共识[J]. 中华神经科杂志, 2021, 54(12):1234-1240. |
| [4] |
Haggag H, Hodgson C. Clinimetrics:Modified rankin scale (mRS)[J]. J Physiother, 2022, 68(4):281.
doi: 10.1016/j.jphys.2022.05.017 URL |
| [5] |
Tyler KL. Acute viral encephalitis[J]. N Engl J Med, 2018, 379(6):557-566.
doi: 10.1056/NEJMra1708714 URL |
| [6] |
Gilden DH, Vafai A, Shtram Y, et al. Varicella-zoster virus DNA in human sensory ganglia[J]. Nature, 1983, 306(5942):478-480.
doi: 10.1038/306478a0 |
| [7] |
Gershon M, Gershon A. Varicella-zoster virus and the enteric nervous system[J]. J Infect Dis, 2018, 218(suppl_2):S113-S119.
doi: 10.1093/infdis/jiy407 URL |
| [8] |
Rajbhandari L, Shukla P, Jagdish B, et al. Nectin-1 is an entry mediator for varicella-zoster virus infection of human neurons[J]. J Virol, 2021, 95 (22):e0122721.
doi: 10.1128/JVI.01227-21 URL |
| [9] |
Thomsen MM, Tyrberg T, Skaalum K, et al. Genetic variants and immune responses in a cohort of patients with varicella zoster virus encephalitis[J]. J Infect Dis, 2021, 224(12):2122-2132.
doi: 10.1093/infdis/jiab254 pmid: 33974706 |
| [10] |
Nagel MA, Niemeyer CS, Bubak AN. Central nervous system infections produced bvaricella zoster virus[J]. Curr Opin Infect Dis, 2020, 33(3):273-278.
doi: 10.1097/QCO.0000000000000647 URL |
| [11] |
McCormick GW. Encephalitis associated with herpes zoster[J]. J Pediatr, 1947, 30(4):473.
doi: 10.1016/S0022-3476(47)80091-5 URL |
| [12] |
George BP, Schneider EB, Venkatesan A. Encephalitis hospitalization rates and inpatient mortality in the United States,2000-2010[J]. PLoS One, 2014, 9(9):e104169.
doi: 10.1371/journal.pone.0104169 URL |
| [13] |
Hong HL, Lee EM, Sung H, et al. Clinical features,outcomes,and cerebrospinal fluid findings in adult patients with central nervous system (CNS) infections caused by varicella-zoster virus:comparison with enterovirus CNS infections[J]. J Med Virol, 2014, 86(12):2049-54.
doi: 10.1002/jmv.23902 URL |
| [14] |
Grahn A, Bergström T, Runesson J, et al. Varicella-zoster virus (VZV) DNA in serum of patients with VZV central nervous system infections[J]. J Infect, 2016, 73(3):254-260.
doi: 10.1016/j.jinf.2016.04.035 pmid: 27317379 |
| [15] |
Omland LH, Vestergaard HT, Dessau RB, et al. Characteristics and long-term prognosis of danish patients with varicella zoster virus detected in cerebrospinal fluid compared with the background population[J]. J Infect Dis, 2021, 224(5):850-859.
doi: 10.1093/infdis/jiab013 pmid: 33417703 |
| [16] |
Sonneville R, Jaquet P, Vellieux G, et al. Intensive care management of patients with viral encephalitis[J]. Rev Neurol (Paris), 2022, 178(1-2):48-56.
doi: 10.1016/j.neurol.2021.12.002 URL |
| [17] |
Wu H, Wang R, Li Y, et al. Cerebrovascular complications after adult-onset varicella-zoster virus encephalitis in the central nervous system:A literature review[J]. Neuropsychiatr Dis Treat, 2022, 18:449-462.
doi: 10.2147/NDT.S343846 URL |
| [18] |
Li X, Liu C, Zhu L, et al. The role of high-resolution magnetic resonance imaging in cerebrovascular disease: A narrative review[J]. Brain Sci, 2023, 13(4):677.
doi: 10.3390/brainsci13040677 URL |
| [19] |
Gilden D, Cohrs RJ, Mahalingam R, et al. Varicella zoster virus vasculopathies: diverse clinical manifestations, laboratory features, pathogenesis, and treatment[J]. Lancet Neurol, 2009, 8(8):731-740.
doi: 10.1016/S1474-4422(09)70134-6 pmid: 19608099 |
| [20] |
Li S, Tang M, Zhang D, et al. The prevalence and prognosis of asymptomatic intracranial atherosclerosis in a community-based population:Results based on high-resolution magnetic resonance imaging[J]. Eur J Neurol, 2023, 30(12):3761-3771.
doi: 10.1111/ene.v30.12 URL |
| [21] |
Bertrand A, Leclercq D, Martinez-Almoyna L, et al. MR imaging of adult acute infectious encephalitis[J]. Med Mal Infect, 2017, 47(3):195-205.
doi: 10.1016/j.medmal.2017.01.002 URL |
| [22] | 朱丽平, 刘磊, 王佳伟. 水痘-带状疱疹病毒合并神经系统感染13例临床分析并文献复习[J]. 北京医学, 2020, 42(7):602-606. |
| [23] |
Manyelo CM, Chegou NN, Seddon JA, et al. Serum and cerebrospinal fluid host proteins indicate stroke in children with tuberculous meningitis[J]. PloS one, 2021, 16(4):e0250944.
doi: 10.1371/journal.pone.0250944 URL |
| [24] | Cao D, Wang T, Wang Y, et al. Analysis of cases with cerebrospinal fluid characteristics similar to tuberculous meningitis[J]. Biomed Res Int, 2022, 2022:9692804. |
| [25] |
Edridge AWD, Deijs M, van Zeggeren IE, et al. Viral metagenomics on cerebrospinal fluid[J]. Genes (Basel), 2019, 10(5): 332.
doi: 10.3390/genes10050332 URL |
| [26] | 陈文, 姚利, 陈康, 等. 宏基因组二代测序技术检测脑脊液在结核性脑膜炎诊断中的应用价值的Meta分析[J]. 中国防痨杂志, 2021, 43(10):1066-1072. |
| [27] |
Collet A, Baes D, Mambie A, et al. VZV meningoencephalitis treated witganciclovir[J]. Med Mal Infect, 2020, 50 (5):444-445.
doi: 10.1016/j.medmal.2020.03.001 URL |
| [28] |
Hodzic E, Hasbun R, Granillo A, et al. Steroids for the treatment of viral encephalitis:A systematic literature review and meta-analysis[J]. J Neurol, 2023, 270 (7):3603-3615.
doi: 10.1007/s00415-023-11715-0 |
| [29] |
Mirouse A, Sonneville R, Razazi K, et al. Neurologic outcome of VZV encephalitis one year after ICU admission:A multicenter cohort study[J]. Ann Intensive Care, 2022, 12(1):32.
doi: 10.1186/s13613-022-01002-y pmid: 35380296 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||