| [1] |
Peng WS, Yang J, Liu EM. Analysis of 170 cases of congenital TB reported in the literature between 1946 and 2009[J]. Pediatr Pulmonol, 2011, 46(12):1215-1224.
|
| [2] |
Cantwell MF, Shehab ZM, Costello AM, et al. Brief report: Congenital tuberculosis[J]. N Engl J Med, 1994, 330(15):1051-1054.
|
| [3] |
卢伟能, 周伟, 赖剑蒲, 等. 先天性结核2例[J]. 中国当代儿科杂志, 2005, 7(4):389-390.
|
| [4] |
Schaaf HS, Collins A, Bekker A, et al. Tuberculosis at extremes of age[J]. Respirology, 2010, 15(5):747-763.
doi: 10.1111/j.1440-1843.2010.01784.x
pmid: 20546192
|
| [5] |
Şen V, Şen HS, Aktar F, et al. Congenital tuberculosis: Presentation of a rare case[J]. Arch Argent Pediatr, 2015, 113(2):e101-e105.
|
| [6] |
岳英, 黄婷婷, 任斐, 等. 先天性耐药结核病一例并文献复习[J]. 中国防痨杂志, 2022, 44(3):252-257.
|
| [7] |
Zhang X, Zhu XR, Xu F, et al. Congenital tuberculosis after in vitro fertilization: Suggestion for tuberculosis tests in infertile women in developing countries[J]. J Int Med Res, 2018, 46(12):5316-5321.
doi: 10.1177/0300060518808179
pmid: 30453806
|
| [8] |
王立伟, 王子珍. 耐多药肺结核病患者应用化疗方案的疗效分析[J]. 临床荟萃, 2014, 29(6):605-607.
|
| [9] |
中国防痨协会. 耐药结核病化学治疗指南(2019年简版)[J]. 中国防痨杂志, 2019, 41(10):1025-1073.
|
| [10] |
Lhadon T, Jullien S. Congenital multidrug-resistant tuberculosis in a neonate: A case report[J]. J Trop Pediatr, 2019, 65(2):188-191.
|
| [11] |
Flibotte JJ, Lee GE, Buser GL, et al. Infertility, in vitro fertilization and congenital tuberculosis[J]. J Perinatol, 2013, 33(7):565-568.
doi: 10.1038/jp.2012.146
pmid: 23803676
|
| [12] |
谢兰品, 董雅坤. 气管支气管结核诊治[J]. 临床荟萃, 2016, 31(10):1058-1062.
|
| [13] |
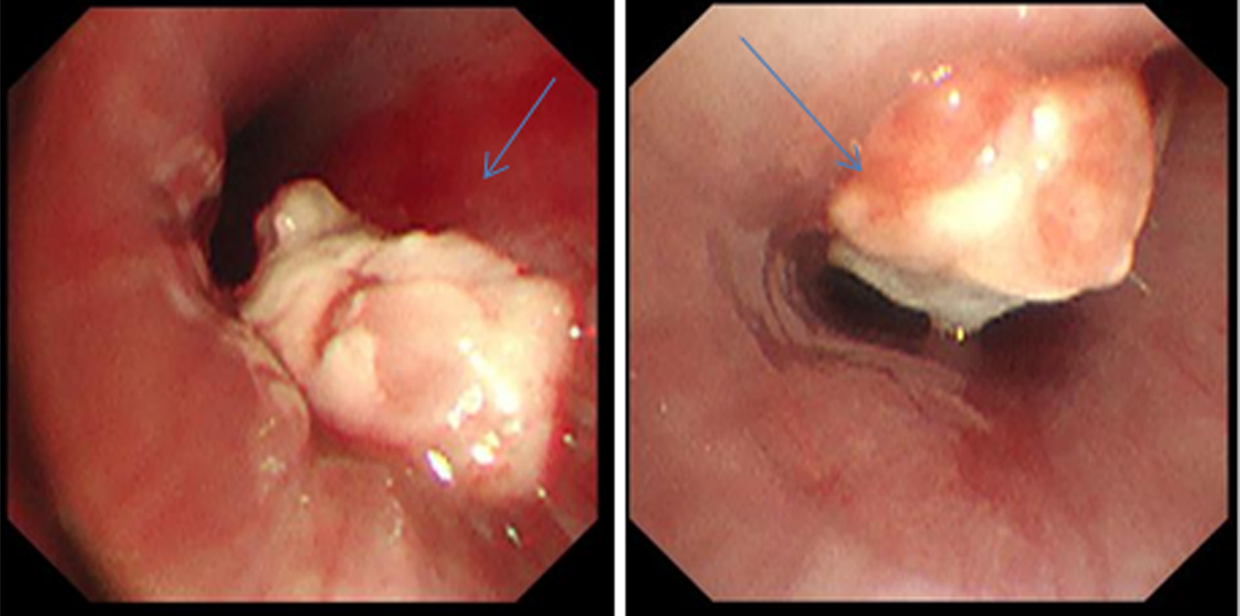
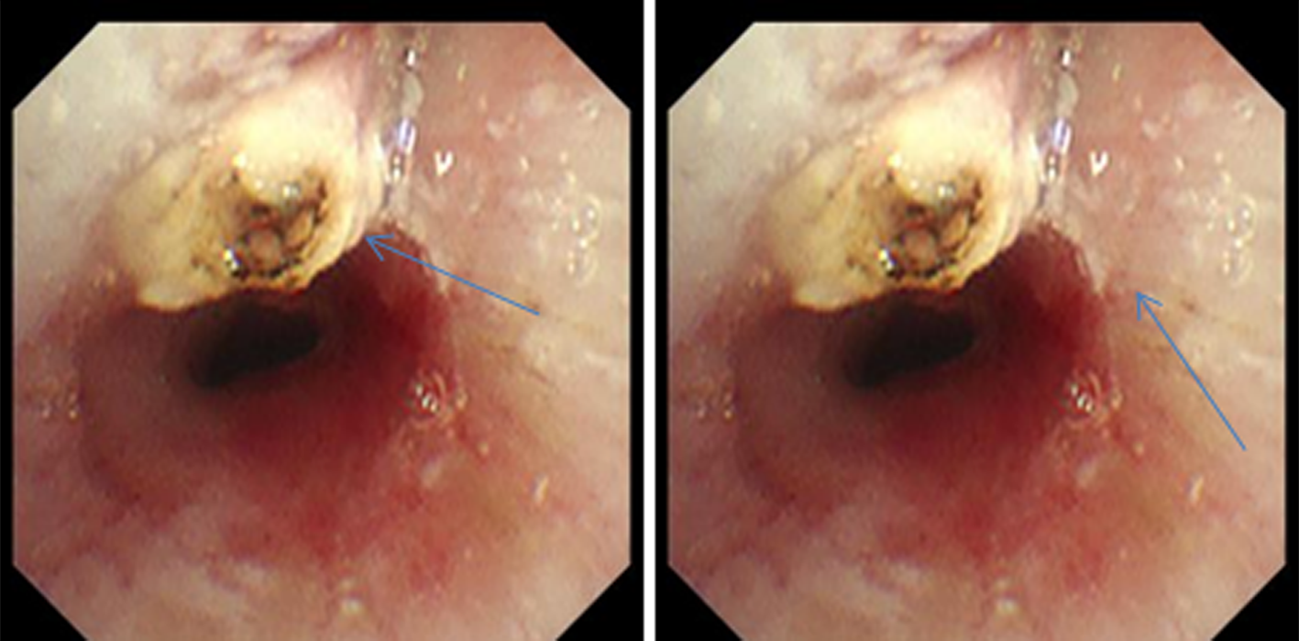
Venturini E, Montagnani C, Boldrini A, et al. Congenital tuberculosis after in vitro fertilization presenting with endobronchial granuloma[J]. Pediatr Neonatol, 2019, 60(1):105-107.
|
| [14] |
秦林, 郭洋, 王文洁, 等. 高频电凝联合冷冻消融治疗肉芽增殖型支气管结核的有效性及安全性[J]. 临床肺科杂志, 2018, 23(11):1950-1954.
|
| [15] |
曾剑锋, 邓群益, 叶涛生. 电子支气管镜下冷冻治疗支气管结核的临床疗效[J]. 中国实用医药, 2015, 10(16):92-93.
|
| [16] |
张慧珊, 陈熙泼, 叶乐平, 等. 经支气管镜冷冻介入在儿童气管支气管结核诊疗中的临床应用[J]. 中华儿科杂志, 2021, 59(11): 963-967.
|
 ), Guo Yongsheng, Zhai Jia, Huang Bing
), Guo Yongsheng, Zhai Jia, Huang Bing