Clinical Focus ›› 2023, Vol. 38 ›› Issue (5): 405-411.doi: 10.3969/j.issn.1004-583X.2023.05.003
Previous Articles Next Articles
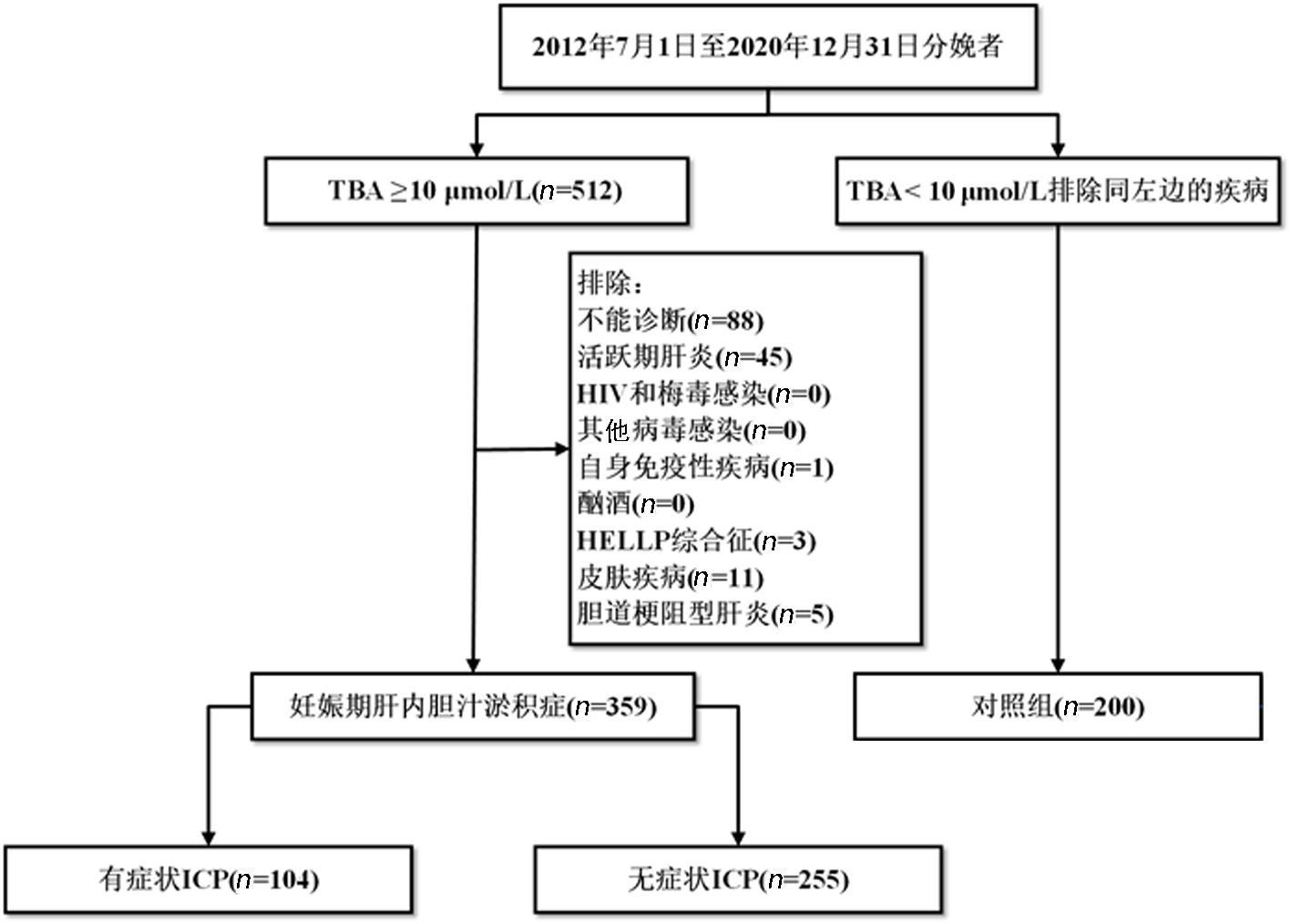
Correlation between pruritus and the prognosis of intrahepatic cholestasis of pregnancy and prediction of its risks
Zhang Yuan, Zhou Juan, Li Wenxiang, Liu Jinxiang, Tang Xiaomei, Luo Huijuan( )
)
- Department of Obstetrics and Gynecology,the First Affiliated Hospital of Jinan University,Guangzhou 510630,China
-
Received:2022-11-21Online:2023-05-20Published:2023-07-20 -
Contact:Luo Huijuan, Email:feelluo@126.com
CLC Number:
Cite this article
Zhang Yuan, Zhou Juan, Li Wenxiang, Liu Jinxiang, Tang Xiaomei, Luo Huijuan. Correlation between pruritus and the prognosis of intrahepatic cholestasis of pregnancy and prediction of its risks[J]. Clinical Focus, 2023, 38(5): 405-411.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2023.05.003
| 项目 | 对照组 (n=200) | 有症状ICP组 (n=104) | 无症状ICP组 (n=255) | P值 |
|---|---|---|---|---|
| 年龄(岁) | 30.0(27.0, 33.0) | 29.0(27.0, 33.7) | 30.0(27.0, 33.0) | 0.887 |
| 孕次(次) | 2.0(1.0, 2.0) | 2.0(1.0, 3.0) | 2.0(1.0, 3.0)* | 0.035 |
| 分娩次数(次) | 1.0(1.0, 2.0) | 1.0(1.0, 2.0) | 2.0(1.0, 2.0)* | 0.013 |
| BMI(kg/m2) | 26.2(24.1, 28.1) | 25.1(23.3, 27.6)* | 25.7(23.5, 27.2) | 0.025 |
| 胆汁酸异常时胎龄(周) | - | 34.3(30.0, 37.0) | 33.0(24.4, 37.3) | 0.254 |
| TBA(μmol/L) | 3.8(2.7, 4.5) | 23.8(15.0, 43.2)* | 21.4(14.5, 31.3)* | <0.01 |
| ALT(IU/L) | 12.5(9.0, 14.0) | 46.5(15.3, 159.3)* | 14.0(10.0, 16.0)*# | <0.01 |
| AST(IU/L) | 18.0(15.0, 20.0) | 50.5(21.3, 104.3)* | 18.0(15.0, 20.0)# | <0.01 |
| TBIL(μmol/L) | 8.2(6.5, 9.0) | 12.3(7.7, 15.5)* | 8.5(7.0, 8.6)*# | <0.01 |
| GC(μmol/L) | 2.8(2.2, 3.7) | 18.2(7.9, 35.8)* | 13.2(7.7, 22.6)* | <0.01 |
| GDM[例(%)] | 23(11.5) | 26(25.0)* | 58(22.8)* | 0.002 |
| 脐血流量 | ||||
| S/D | 2.1(1.9, 2.3) | 2.4(2.1, 2.7)* | 2.2(2.0, 2.5)*# | <0.01 |
| PI | 0.7(0.7, 0.9) | 0.8(0.7, 1.0)* | 0.8(0.7, 0.9)# | 0.002 |
| RI | 0.5(0.5, 0.6) | 0.6(0.5, 0.6)* | 0.6(0.5, 0.6) | 0.012 |
| 早产[例(%)] | 6(3.0) | 30(28.8)* | 47(18.4)*# | <0.01 |
| 医源性早产 | 0 | 15(14.4)* | 16 (6.3)*# | <0.01 |
| 自发性早产 | 6(3.0) | 15(14.4)* | 31(12.2)* | 0.001 |
| 分娩时胎龄(周) | 39.4(38.6, 40.2) | 37.6(36.4, 38.5)* | 38.3(37.2, 39.1)*# | <0.01 |
| 分娩方式[例(%)] | ||||
| 剖宫产 | 40(20.0) | 71(68.3)* | 123 (48.2)*# | <0.01 |
| 阴道助产 | 8(4.0) | 2(1.9) | 6(2.4) | 0.912 |
| 正常分娩 | 152(76.0) | 31(29.8)* | 126 (49.4)*# | <0.01 |
| 新生儿体重(g) | 3250(2950, 3450) | 3000(2650, 3200)* | 3000(2700, 3300)* | <0.01 |
| 新生儿性别(女)[例(%)] | 96(48.0) | 45(43.3) | 124(48.6) | 0.639 |
| 胎儿宫内窘迫[例(%)] | 31(15.5) | 18(17.3) | 44(17.2) | 0.853 |
| 羊水异常[例(%)] | 14(7.0) | 21(20.2)* | 26(10.2)# | 0.002 |
| MSAF | 11(5.5) | 17(16.4)* | 24(9.4) | 0.008 |
| 羊水过少 | 3(1.5) | 4(3.8) | 2(0.8) | 0.110 |
| 新生儿窒息[例(%)] | 3(1.5) | 4(3.8) | 12(4.7) | 0.164 |
Tab.1 Comparison of general data among the three groups
| 项目 | 对照组 (n=200) | 有症状ICP组 (n=104) | 无症状ICP组 (n=255) | P值 |
|---|---|---|---|---|
| 年龄(岁) | 30.0(27.0, 33.0) | 29.0(27.0, 33.7) | 30.0(27.0, 33.0) | 0.887 |
| 孕次(次) | 2.0(1.0, 2.0) | 2.0(1.0, 3.0) | 2.0(1.0, 3.0)* | 0.035 |
| 分娩次数(次) | 1.0(1.0, 2.0) | 1.0(1.0, 2.0) | 2.0(1.0, 2.0)* | 0.013 |
| BMI(kg/m2) | 26.2(24.1, 28.1) | 25.1(23.3, 27.6)* | 25.7(23.5, 27.2) | 0.025 |
| 胆汁酸异常时胎龄(周) | - | 34.3(30.0, 37.0) | 33.0(24.4, 37.3) | 0.254 |
| TBA(μmol/L) | 3.8(2.7, 4.5) | 23.8(15.0, 43.2)* | 21.4(14.5, 31.3)* | <0.01 |
| ALT(IU/L) | 12.5(9.0, 14.0) | 46.5(15.3, 159.3)* | 14.0(10.0, 16.0)*# | <0.01 |
| AST(IU/L) | 18.0(15.0, 20.0) | 50.5(21.3, 104.3)* | 18.0(15.0, 20.0)# | <0.01 |
| TBIL(μmol/L) | 8.2(6.5, 9.0) | 12.3(7.7, 15.5)* | 8.5(7.0, 8.6)*# | <0.01 |
| GC(μmol/L) | 2.8(2.2, 3.7) | 18.2(7.9, 35.8)* | 13.2(7.7, 22.6)* | <0.01 |
| GDM[例(%)] | 23(11.5) | 26(25.0)* | 58(22.8)* | 0.002 |
| 脐血流量 | ||||
| S/D | 2.1(1.9, 2.3) | 2.4(2.1, 2.7)* | 2.2(2.0, 2.5)*# | <0.01 |
| PI | 0.7(0.7, 0.9) | 0.8(0.7, 1.0)* | 0.8(0.7, 0.9)# | 0.002 |
| RI | 0.5(0.5, 0.6) | 0.6(0.5, 0.6)* | 0.6(0.5, 0.6) | 0.012 |
| 早产[例(%)] | 6(3.0) | 30(28.8)* | 47(18.4)*# | <0.01 |
| 医源性早产 | 0 | 15(14.4)* | 16 (6.3)*# | <0.01 |
| 自发性早产 | 6(3.0) | 15(14.4)* | 31(12.2)* | 0.001 |
| 分娩时胎龄(周) | 39.4(38.6, 40.2) | 37.6(36.4, 38.5)* | 38.3(37.2, 39.1)*# | <0.01 |
| 分娩方式[例(%)] | ||||
| 剖宫产 | 40(20.0) | 71(68.3)* | 123 (48.2)*# | <0.01 |
| 阴道助产 | 8(4.0) | 2(1.9) | 6(2.4) | 0.912 |
| 正常分娩 | 152(76.0) | 31(29.8)* | 126 (49.4)*# | <0.01 |
| 新生儿体重(g) | 3250(2950, 3450) | 3000(2650, 3200)* | 3000(2700, 3300)* | <0.01 |
| 新生儿性别(女)[例(%)] | 96(48.0) | 45(43.3) | 124(48.6) | 0.639 |
| 胎儿宫内窘迫[例(%)] | 31(15.5) | 18(17.3) | 44(17.2) | 0.853 |
| 羊水异常[例(%)] | 14(7.0) | 21(20.2)* | 26(10.2)# | 0.002 |
| MSAF | 11(5.5) | 17(16.4)* | 24(9.4) | 0.008 |
| 羊水过少 | 3(1.5) | 4(3.8) | 2(0.8) | 0.110 |
| 新生儿窒息[例(%)] | 3(1.5) | 4(3.8) | 12(4.7) | 0.164 |
| 项目 | 有症状ICP组 | 无症状ICP组 | P值 | ||
|---|---|---|---|---|---|
| 轻度(n=67) | 重度(n =37) | 轻度(n=196) | 重度(n=59) | ||
| 早发型 | 12(17.9) | 7(18.9) | 45(23.0) | 29(49.2)*#△ | <0.01 |
| 迟发型 | 55(82.1) | 30(81.1) | 151(76.3) | 30(50.9) | |
| 分娩方式 | |||||
| 剖宫产 | 46(68.7) | 27(75.7) | 89(45.4)*# | 39(66.1)△ | <0.01 |
| 阴道分娩 | 21(31.3) | 10(27.0) | 107(54.6) | 20(33.9) | |
| 早产 | 15(22.4) | 16(43.2)* | 25(12.8)# | 21(35.6)△ | <0.01 |
| 医源性早产 | 6(9.0) | 10(27.0)* | 6(3.1)# | 10(17.0)△ | <0.01 |
| 自发性早产 | 9(13.4) | 6(16.2) | 19(9.7) | 11(18.6) | 0.266 |
| 胎儿宫内死亡 | 0 | 1(2.7) | 1(0.5) | 0 | 0.285 |
| 胎儿窘迫 | 13(5.2) | 4(10.8) | 35(17.9) | 6(10.2) | 0.350 |
| 羊水异常 | 12(17.9) | 10(27.0) | 20(10.2)# | 6(10.2)# | 0.025 |
| MSAF | 9(13.4) | 8(21.6) | 19(9.7) | 5(8.5) | 0.161 |
| 羊水过少 | 3(4.5) | 2(5.4) | 1(0.5) | 1(1.7) | 0.082 |
| 新生儿窒息 | 4(6.0) | 0 | 8(4.1) | 4(6.8) | 0.400 |
| 胎儿宫内死亡 | 0 | 1(2.7) | 1(0.5) | 0 | 0.285 |
Tab.2 Comparison of clinical data between symptomatic ICP group and asymptomatic ICP group (n,%)
| 项目 | 有症状ICP组 | 无症状ICP组 | P值 | ||
|---|---|---|---|---|---|
| 轻度(n=67) | 重度(n =37) | 轻度(n=196) | 重度(n=59) | ||
| 早发型 | 12(17.9) | 7(18.9) | 45(23.0) | 29(49.2)*#△ | <0.01 |
| 迟发型 | 55(82.1) | 30(81.1) | 151(76.3) | 30(50.9) | |
| 分娩方式 | |||||
| 剖宫产 | 46(68.7) | 27(75.7) | 89(45.4)*# | 39(66.1)△ | <0.01 |
| 阴道分娩 | 21(31.3) | 10(27.0) | 107(54.6) | 20(33.9) | |
| 早产 | 15(22.4) | 16(43.2)* | 25(12.8)# | 21(35.6)△ | <0.01 |
| 医源性早产 | 6(9.0) | 10(27.0)* | 6(3.1)# | 10(17.0)△ | <0.01 |
| 自发性早产 | 9(13.4) | 6(16.2) | 19(9.7) | 11(18.6) | 0.266 |
| 胎儿宫内死亡 | 0 | 1(2.7) | 1(0.5) | 0 | 0.285 |
| 胎儿窘迫 | 13(5.2) | 4(10.8) | 35(17.9) | 6(10.2) | 0.350 |
| 羊水异常 | 12(17.9) | 10(27.0) | 20(10.2)# | 6(10.2)# | 0.025 |
| MSAF | 9(13.4) | 8(21.6) | 19(9.7) | 5(8.5) | 0.161 |
| 羊水过少 | 3(4.5) | 2(5.4) | 1(0.5) | 1(1.7) | 0.082 |
| 新生儿窒息 | 4(6.0) | 0 | 8(4.1) | 4(6.8) | 0.400 |
| 胎儿宫内死亡 | 0 | 1(2.7) | 1(0.5) | 0 | 0.285 |
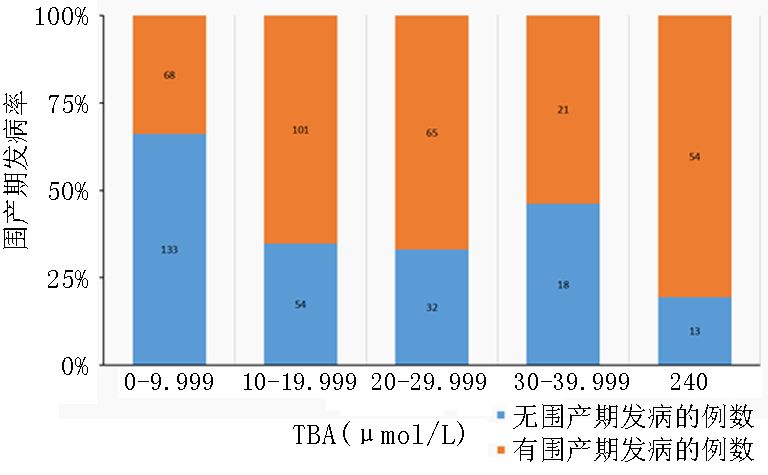
| TBA (μmol/L) | 有症状ICP围产期发病率 | 无症状ICP围产期发病率 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | P值 | 95%CI | OR值 | P值 | 95%CI | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| 10~19.999 | 7.710 | <0.01 | 3.370 | 17.638 | 2.934 | <0.01 | 1.827 | 4.712 |
| 20~29.999 | 4.681 | 0.001 | 1.853 | 11.829 | 3.755 | <0.01 | 2.135 | 6.606 |
| 30~39.999 | 7.710 | 0.11 | 1.594 | 37.303 | 1.589 | 0.249 | 0.723 | 3.495 |
| ≥40 | 12.047 | <0.01 | 4.031 | 36.004 | 6.302 | <0.01 | 2.824 | 14.067 |
Tab.3 Risk factors for perinatal morbidity of ICP
| TBA (μmol/L) | 有症状ICP围产期发病率 | 无症状ICP围产期发病率 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR值 | P值 | 95%CI | OR值 | P值 | 95%CI | |||
| 下限 | 上限 | 下限 | 上限 | |||||
| 10~19.999 | 7.710 | <0.01 | 3.370 | 17.638 | 2.934 | <0.01 | 1.827 | 4.712 |
| 20~29.999 | 4.681 | 0.001 | 1.853 | 11.829 | 3.755 | <0.01 | 2.135 | 6.606 |
| 30~39.999 | 7.710 | 0.11 | 1.594 | 37.303 | 1.589 | 0.249 | 0.723 | 3.495 |
| ≥40 | 12.047 | <0.01 | 4.031 | 36.004 | 6.302 | <0.01 | 2.824 | 14.067 |
| [1] |
Arrese M, Macias RI, Briz O, et al. Molecular pathogenesis of intrahepatic cholestasis of pregnancy[J]. Expert Rev Mol Med, 2008, 10: e9.
doi: 10.1017/S1462399408000628 URL |
| [2] |
Lammert F, Marschall HU, Matern S. Intrahepatic cholestasis of pregnancy[J]. Curr Treat Options Gastroenterol, 2003, 6(2): 123-132.
pmid: 12628071 |
| [3] |
Geenes V, Williamson C. Intrahepatic cholestasis of pregnancy[J]. World J Gastroenterol, 2009, 15(17): 2049-2066.
doi: 10.3748/wjg.15.2049 URL |
| [4] |
Glantz A, Marschall HU, Mattsson LA. Intrahepatic cholestasis of pregnancy: Relationships between bile acid levels and fetal complication rates[J]. Hepatology, 2004, 40(2): 467-474.
doi: 10.1002/hep.20336 pmid: 15368452 |
| [5] |
Pascual MJ, Serrano MA, El-Mir MY, et al. Relationship between asymptomatic hypercholanaemia of pregnancy and progesterone metabolism[J]. Clin Sci (Lond), 2002, 102(5): 587-593.
doi: 10.1042/cs1020587 URL |
| [6] |
Feng D, He W. Asymptomatic elevated total serum bile acids representing an unusual form of intrahepatic cholestasis of pregnancy[J]. Int J Gynaecol Obstet, 2016, 134(3): 343-344.
doi: 10.1016/j.ijgo.2016.04.004 pmid: 27481015 |
| [7] |
Lunzer M, Barnes P, Byth K, et al. Serum bile acid concentrations during pregnancy and their relationship to obstetric cholestasis[J]. Gastroenterology, 1986, 91(4): 825-829.
pmid: 3743960 |
| [8] |
Castaño G, Lucangioli S, Sookoian S, et al. Bile acid profiles by capillary electrophoresis in intrahepatic cholestasis of pregnancy[J]. Clin Sci (Lond), 2006, 110(4): 459-465.
doi: 10.1042/CS20050302 URL |
| [9] | Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Guidelines for diagnosis and treatment of intrahepatic cholestasis of pregnancy (2015)[J]. Zhonghua Fu Chan Ke Za Zhi, 2015, 50(7): 481-485. |
| [10] | Whittington JR, Allen LR, Ennen CS, et al. Relationship between maternal serum bile acid levels and fetal cardiac troponin-I levels in asymptomatic pregnant patients at term: A cross-sectional observational study[J]. Cureus, 2019, 11(8): e5508. |
| [11] |
Alemi F, Kwon E, Poole DP, et al. The TGR5 receptor mediates bile acid-induced itch and analgesia[J]. J Clin Invest, 2013, 123(4): 1513-1530.
doi: 10.1172/JCI64551 pmid: 23524965 |
| [12] |
Kondrackiene J, Beuers U, Zalinkevicius R, et al. Predictors of premature delivery in patients with intrahepatic cholestasis of pregnancy[J]. World J Gastroenterol, 2007, 13(46): 6226-6230.
doi: 10.3748/wjg.v13.i46.6226 URL |
| [13] |
Lee NM, Brady CW. Liver disease in pregnancy[J]. World J Gastroenterol, 2009, 15(8): 897-906.
doi: 10.3748/wjg.15.897 URL |
| [14] |
Mullally BA, Hansen WF. Intrahepatic cholestasis of pregnancy: Review of the literature[J]. Obstet Gynecol Surv, 2002, 57(1): 47-52.
doi: 10.1097/00006254-200201000-00023 pmid: 11773831 |
| [15] |
Hepburn IS, Schade RR. Pregnancy-associated liver disorders[J]. Dig Dis Sci, 2008, 53(9): 2334-2358.
doi: 10.1007/s10620-007-0167-9 URL |
| [16] |
Angueira AR, Ludvik AE, Reddy TE, et al. New insights into gestational glucose metabolism: Lessons learned from 21st century approaches[J]. Diabetes, 2015, 64(2): 327-334.
doi: 10.2337/db14-0877 pmid: 25614666 |
| [17] |
Men·zyk T, Bator M, Derra A, et al. The role of metabolic disorders in the pathogenesis of intrahepatic cholestasis of pregnancy[J]. Clin Exp Hepatol, 2018, 4(4): 217-223.
doi: 10.5114/ceh.2018.80122 URL |
| [18] |
Liu C, Gao J, Liu J, et al. Intrahepatic cholestasis of pregnancy is associated with an increased risk of gestational diabetes and preeclampsia[J]. Ann Transl Med, 2020, 8(23): 1574.
doi: 10.21037/atm-20-4879 pmid: 33437773 |
| [19] |
Jain R, Suri V, Chopra S, et al. Obstetric cholestasis: Outcome with active management[J]. J Obstet Gynaecol Res, 2013, 39(5): 953-959.
doi: 10.1111/jog.12005 URL |
| [20] |
Lo JO, Shaffer BL, Allen AJ, et al. Intrahepatic cholestasis of pregnancy and timing of delivery[J]. J Matern Fetal Neonatal Med, 2015, 28(18): 2254-2258.
doi: 10.3109/14767058.2014.984605 pmid: 25371372 |
| [21] | Puljic A, Kim E, Page J, et al. The risk of infant and fetal death by each additional week of expectant management in intrahepatic cholestasis of pregnancy by gestational age[J]. Am J Obstet Gynecol, 2015, 212(5): 667. |
| [22] |
Arthur C, Mahomed K. Intrahepatic cholestasis of pregnancy: Diagnosis and management; a survey of royal Australian and New Zealand college of obstetrics and gynaecology fellows[J]. Aust N Z J Obstet Gynaecol, 2014, 54(3): 263-267.
doi: 10.1111/ajo.12178 pmid: 24506294 |
| [23] | Nichols AA. Cholestasis of pregnancy: A review of the evidence[J]. J Perinat Neonatal Nurs, 2005, 19(3): 217-225. |
| [24] |
Mays JK. The active management of intrahepatic cholestasis of pregnancy[J]. Curr Opin Obstet Gynecol, 2010, 22(2): 100-103.
doi: 10.1097/GCO.0b013e328337238d URL |
| [25] |
Floreani A, Gervasi MT. New insights on intrahepatic cholestasis of pregnancy[J]. Clin Liver Dis, 2016, 20(1): 177-189.
doi: 10.1016/j.cld.2015.08.010 pmid: 26593298 |
| [26] |
Mozurkewich E, Chilimigras J, Koepke E, et al. Indications for induction of labour: A best-evidence review[J]. BJOG, 2009, 116(5): 626-636.
doi: 10.1111/j.1471-0528.2008.02065.x URL |
| [27] | Menezes EV, Yakoob MY, Soomro T, et al. Reducing stillbirths: Prevention and management of medical disorders and infections during pregnancy[J]. BMC Pregnancy Childbirth, 2009, 9 Suppl 1(Suppl 1): S4. |
| [28] |
Henderson CE, Shah RR, Gottimukkala S, et al. Primum non nocere: How active management became modus operandi for intrahepatic cholestasis of pregnancy[J]. Am J Obstet Gynecol, 2014, 211(3): 189-196.
doi: 10.1016/j.ajog.2014.03.058 pmid: 24704063 |
| [29] |
Girling JC, Dow E, Smith JH. Liver function tests in pre-eclampsia: Importance of comparison with a reference range derived for normal pregnancy[J]. Br J Obstet Gynaecol, 1997, 104(2): 246-250.
pmid: 9070148 |
| [30] |
Zecca E, De Luca D, Baroni S, et al. Bile acid-induced lung injury in newborn infants: A bronchoalveolar lavage fluid study[J]. Pediatrics, 2008, 121(1): e146-149.
doi: 10.1542/peds.2007-1220 URL |
| [31] |
Vasavan T, Deepak S, Jayawardane IA, et al. Fetal cardiac dysfunction in intrahepatic cholestasis of pregnancy is associated with elevated serum bile acid concentrations[J]. J Hepatol, 2021, 74(5): 1087-1096.
doi: 10.1016/j.jhep.2020.11.038 URL |
| [32] |
Madazli R, Yuksel MA, Oncul M, et al. Pregnancy outcomes and prognostic factors in patients with intrahepatic cholestasis of pregnancy[J]. J Obstet Gynaecol, 2015, 35(4): 358-361.
doi: 10.3109/01443615.2014.968102 pmid: 25384180 |
| [33] | Estiú MC, Frailuna MA, Otero C, et al. Relationship between early onset severe intrahepatic cholestasis of pregnancy and higher risk of meconium-stained fluid[J]. PLoS One, 2017, 12(4): e0176504. |
| [34] |
Piechota J, Jelski W. Intrahepatic cholestasis in pregnancy: Review of the literature[J]. J Clin Med, 2020, 9(5): 1361.
doi: 10.3390/jcm9051361 URL |
| [35] |
Yule CS, Holcomb DS, Kraus AC, et al. Cholestasis: A prospective study of perinatal outcomes and time to symptom improvement[J]. Am J Perinatol, 2021, 38(5): 414-420.
doi: 10.1055/s-0040-1717076 URL |
| [1] | . [J]. Clinical Focus, 2024, 39(2): 177-182. |
| [2] | . [J]. Clinical Focus, 2024, 39(1): 84-87. |
| [3] | . [J]. Clinical Focus, 2023, 38(10): 935-939. |
| [4] | . [J]. Clinical Focus, 2023, 38(6): 559-563. |
| [5] | . [J]. Clinical Focus, 2023, 38(4): 373-376. |
| [6] | Cao Yumeng, Zhang Haiyan, Liu Lixin. Correlation between pathological changes and serum ferritin and iron levels in nonalcoholic fatty liver disease: A meta-analysis [J]. Clinical Focus, 2023, 38(3): 197-207. |
| [7] | . [J]. Clinical Focus, 2022, 37(9): 846-854. |
| [8] | Zhang Limin, Sun Jun. Predictive value of FIB-4 in patients with metabolic-associated fatty liver disease complicated with colorectal adenomatous polyps [J]. Clinical Focus, 2022, 37(4): 334-338. |
| [9] | Wang Dandan, Zhang Xiaolan, Deng Zhihua. Clinical characteristic of Primary biliary cholangitis complicating Sjögren syndrome [J]. Clinical Focus, 2022, 37(1): 30-34. |
| [10] | Wen Jie. Correlation analysis between atherogenic index of plasma and nonalcoholic fatty liver disease [J]. Clinical Focus, 2022, 37(1): 35-38. |
| [11] | Qu Ying, Liu Zhongyang. Relationship between tuberculin test with serum apolipoprotein A-1 and anti-tuberculosis drug-induced liver injury [J]. Clinical Focus, 2022, 37(1): 39-42. |
| [12] | . [J]. Clinical Focus, 2022, 37(1): 72-76. |
| [13] | Yang Zhibin, Shao Yanfang, Pan Li, Yang Yanxia, Yang Yuxi, Zhao Lihui, Zeng Rongkun, Li Yang, Wang Qiaofeng, Wang Cong, Ma Shiwu. Efficacy of magnesium isoglycyrrhizinate in anti-tuberculosis drug-induced liver injury [J]. Clinical Focus, 2021, 36(11): 972-975. |
| [14] | . [J]. Clinical Focus, 2021, 36(9): 856-860. |
| [15] | Li Guohuan, Xie Xu, Huang Zhixia, Zhang Mingye, Tang Yunyun. Quantitative evaluation of transient elastography and acoustic radiation force pulse imaging for non-alcoholic fatty liver disease [J]. Clinical Focus, 2021, 36(6): 535-539. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||