

临床荟萃 ›› 2024, Vol. 39 ›› Issue (7): 612-619.doi: 10.3969/j.issn.1004-583X.2024.07.005
延天美1,3, 吴亚楠2,3, 刘月影1,3, 魏立民3( )
)
收稿日期:2023-12-27
出版日期:2024-07-20
发布日期:2024-08-02
通讯作者:
魏立民
E-mail:15133130672@163.com
基金资助:
Yan Tianmei1,3, Wu Yanan2,3, Liu Yueying1,3, Wei Limin3( )
)
Received:2023-12-27
Online:2024-07-20
Published:2024-08-02
Contact:
Wei Limin
E-mail:15133130672@163.com
摘要:
目的 本研究旨在探讨甘油三酯葡萄糖指数(triglycerides-glucose index,TyG)及TyG联合肥胖指标与2型糖尿病(type 2 diabetes mellitus,T2DM)患者视网膜病变(diabetic retinopathy,DR)的相关性。分析TyG指数及TyG联合肥胖指标对DR的预测价值。方法 本研究为回顾性研究,依据纳入标准以及排除标准,共收集了2018年9月至2021年5月于河北省人民医院内分泌科住院治疗的373名T2DM患者资料,依据是否合并DR,将其分为T2DM未合并DR组及合并DR组。收集患者临床资料,计算指标TyG、甘油三酯葡萄糖-腰围指数(triglyceride-glucose-waist circumference index,TyG-WC)、甘油三酯葡萄糖-体重指数(triglyceride-glucose-body mass index,TyG-BMI)、甘油三酯葡萄糖-腰臀比指数(tyG-waist-to-hip ratio,TyG-WHR)、甘油三酯葡萄糖-腰围身高比指数(tyG-waist-to-height ratio,TyG-WHtR)。采用二元Logistic回归分析其危险因素,绘制ROC曲线来评估TyG、TyG-WC、TyG-BMI、TyG-WHR、TyG-WHtR对DR的预测价值。结果 ①T2DM合并DR组的年龄、糖尿病病程、腰围、WHR、WHtR、甘油三酯、肌酐、尿素氮、空腹血糖、糖化血红蛋白、TyG、TyG-WC、TyG-BMI、TyG-WHR、TyG-WHtR均高于未合并DR组,肾小球滤过率低于未合并DR组。② DR与年龄、糖尿病病程、腰围、WHR、WHtR、甘油三酯、肌酐、尿素氮、空腹血糖、糖化血红蛋白、TyG、TyG-WC、TyG-BMI、TyG-WHR、TyG-WHtR呈正相关,与肾小球滤过率呈负相关。③TyG、TyG-WC、TyG-BMI、TyG-WHR、TyG-WHtR均是DR的独立危险因素。④ROC分析显示,TyG、TyG-WC、TyG-BMI、TyG-WHR、TyG-WHtR均对DR有预测价值,且TyG-WHR的AUC(0.623)最大。结论 TyG-WHR与DR密切相关,有望成为早期识别DR风险的一种新的临床有效标志物。
中图分类号:
延天美, 吴亚楠, 刘月影, 魏立民. 甘油三酯葡萄糖指数联合肥胖指标与糖尿病视网膜病变的相关性[J]. 临床荟萃, 2024, 39(7): 612-619.
Yan Tianmei, Wu Yanan, Liu Yueying, Wei Limin. Correlation of triglyceride-glucose index combined with obesity indicators with diabetic retinopathy[J]. Clinical Focus, 2024, 39(7): 612-619.
| 组别 | 例数 | 性别(男) [例(%)] | 吸烟史 [例(%)] | 饮酒史 [例(%)] | 年龄 (岁) | 糖尿病病程 (月) | 身高 (cm) | 体重 (kg) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非DR组 | 261 | 156(59.8) | 68(26.1) | 64(24.5) | 56(46,66) | 60(12,132) | 168(160,174.25) | 73±13.54 | |||||||
| DR组 | 112 | 63(56.3) | 32(28.6) | 28(25.0) | 61(50,67) | 144(84,240) | 168(159,172) | 74(66,82) | |||||||
| χ2/ | 0.401 | 1.256 | 0.443 | -2.300 | -7.065 | -0.856 | -0.990 | ||||||||
| P值 | 0.527 | 0.262 | 0.506 | 0.021 | <0.001 | 0.392 | 0.322 | ||||||||
| 组别 | BMI (kg/m2) | WC (cm) | 臀围 (cm) | WHR | WHtR | SBP (mmHg) | DBP (mmHg) | ||||||||
| 非DR组 | 25.95±3.54 | 92(86,100) | 100.36±9.22 | 0.93(0.88,0.96) | 0.55±0.06 | 132(121,146) | 83.07±12.39 | ||||||||
| DR组 | 26.37(24.58,28.73) | 95(88,101) | 100(96,105) | 0.94±0.07 | 0.56(0.53,0.61) | 136(121,150) | 81.39±11.66 | ||||||||
| -1.683 | -2.093 | -0.335 | -2.435 | -2.405 | -1.775 | 1.497 | |||||||||
| P值 | 0.092 | 0.036 | 0.738 | 0.015 | 0.016 | 0.076 | 0.135 | ||||||||
表1 两组一般资料比较
Tab.1 General data between groups
| 组别 | 例数 | 性别(男) [例(%)] | 吸烟史 [例(%)] | 饮酒史 [例(%)] | 年龄 (岁) | 糖尿病病程 (月) | 身高 (cm) | 体重 (kg) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非DR组 | 261 | 156(59.8) | 68(26.1) | 64(24.5) | 56(46,66) | 60(12,132) | 168(160,174.25) | 73±13.54 | |||||||
| DR组 | 112 | 63(56.3) | 32(28.6) | 28(25.0) | 61(50,67) | 144(84,240) | 168(159,172) | 74(66,82) | |||||||
| χ2/ | 0.401 | 1.256 | 0.443 | -2.300 | -7.065 | -0.856 | -0.990 | ||||||||
| P值 | 0.527 | 0.262 | 0.506 | 0.021 | <0.001 | 0.392 | 0.322 | ||||||||
| 组别 | BMI (kg/m2) | WC (cm) | 臀围 (cm) | WHR | WHtR | SBP (mmHg) | DBP (mmHg) | ||||||||
| 非DR组 | 25.95±3.54 | 92(86,100) | 100.36±9.22 | 0.93(0.88,0.96) | 0.55±0.06 | 132(121,146) | 83.07±12.39 | ||||||||
| DR组 | 26.37(24.58,28.73) | 95(88,101) | 100(96,105) | 0.94±0.07 | 0.56(0.53,0.61) | 136(121,150) | 81.39±11.66 | ||||||||
| -1.683 | -2.093 | -0.335 | -2.435 | -2.405 | -1.775 | 1.497 | |||||||||
| P值 | 0.092 | 0.036 | 0.738 | 0.015 | 0.016 | 0.076 | 0.135 | ||||||||
| 组别 | 例数 | TC(mmol/L) | TG(mmol/L) | LDL-C(mmol/L) | HDL-C(mmol/L) | SCr(mmol/L) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 非DR组 | 261 | 4.785(4.04, 5.53) | 1.44(0.99, 2.02) | 3.105(2.54, 3.68) | 1.1(0.99, 1.28) | 67.9(59.18, 74.1) | ||||
| DR组 | 112 | 4.9(4.31, 5.86) | 1.56(1.15, 2.44) | 3.15(2.75, 3.86) | 1.08(0.88, 1.24) | 70.3(59.9, 85.7) | ||||
| -1.363 | -2.321 | -1.269 | -1.607 | -3.024 | ||||||
| P值 | 0.173 | 0.020 | 0.204 | 0.108 | 0.002 | |||||
| 组别 | BUN(mmol/L) | UA(mmol/L) | GFR (mL/min) | FBG(mmol/L) | HbA1c(%) | |||||
| 非DR组 | 5.2(4.4, 6) | 304.64(240.75, 356) | 98.79(88.76, 107.3) | 7.61(6.1, 9.485) | 8.3(7.1, 9.9) | |||||
| DR组 | 5.5(4.6, 7.3) | 318.5(260.3, 371.3) | 92.87(70.84, 103.07) | 8.375(6.63, 11.585) | 8.9(7.5, 10.7) | |||||
| -3.197 | -1.436 | -3.924 | -2.845 | -2.810 | ||||||
| P值 | 0.001 | 0.151 | <0.001 | 0.004 | 0.005 | |||||
表2 两组生化指标比较[ M(P25,P75)]
Tab.2 Biochemical indicators between groups[ M(P25,P75)]
| 组别 | 例数 | TC(mmol/L) | TG(mmol/L) | LDL-C(mmol/L) | HDL-C(mmol/L) | SCr(mmol/L) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 非DR组 | 261 | 4.785(4.04, 5.53) | 1.44(0.99, 2.02) | 3.105(2.54, 3.68) | 1.1(0.99, 1.28) | 67.9(59.18, 74.1) | ||||
| DR组 | 112 | 4.9(4.31, 5.86) | 1.56(1.15, 2.44) | 3.15(2.75, 3.86) | 1.08(0.88, 1.24) | 70.3(59.9, 85.7) | ||||
| -1.363 | -2.321 | -1.269 | -1.607 | -3.024 | ||||||
| P值 | 0.173 | 0.020 | 0.204 | 0.108 | 0.002 | |||||
| 组别 | BUN(mmol/L) | UA(mmol/L) | GFR (mL/min) | FBG(mmol/L) | HbA1c(%) | |||||
| 非DR组 | 5.2(4.4, 6) | 304.64(240.75, 356) | 98.79(88.76, 107.3) | 7.61(6.1, 9.485) | 8.3(7.1, 9.9) | |||||
| DR组 | 5.5(4.6, 7.3) | 318.5(260.3, 371.3) | 92.87(70.84, 103.07) | 8.375(6.63, 11.585) | 8.9(7.5, 10.7) | |||||
| -3.197 | -1.436 | -3.924 | -2.845 | -2.810 | ||||||
| P值 | 0.001 | 0.151 | <0.001 | 0.004 | 0.005 | |||||
| 组别 | 例数 | TyG | TyG-WC | TyG-BMI | TyG-WHR | TyG-WHtR |
|---|---|---|---|---|---|---|
| 非DR组 | 261 | 10.26±0.43 | 942.36(878.89, 1016.43) | 266.32±38.74 | 9.48(8.98, 9.98) | 5.63(5.24, 6.05) |
| DR组 | 112 | 10.43±0.44 | 975.19(906.71, 1055.61) | 275.08(251.63, 303.48) | 9.83±0.83 | 5.86(5.43, 6.48) |
| -3.581 | -3.151 | -2.587 | -3.762 | -3.437 | ||
| P值 | <0.001 | 0.002 | 0.010 | <0.001 | 0.001 |
表3 两组TyG及TyG联合肥胖指标比较
Tab.3 TyG and TyG combined with obesity indicators between groups
| 组别 | 例数 | TyG | TyG-WC | TyG-BMI | TyG-WHR | TyG-WHtR |
|---|---|---|---|---|---|---|
| 非DR组 | 261 | 10.26±0.43 | 942.36(878.89, 1016.43) | 266.32±38.74 | 9.48(8.98, 9.98) | 5.63(5.24, 6.05) |
| DR组 | 112 | 10.43±0.44 | 975.19(906.71, 1055.61) | 275.08(251.63, 303.48) | 9.83±0.83 | 5.86(5.43, 6.48) |
| -3.581 | -3.151 | -2.587 | -3.762 | -3.437 | ||
| P值 | <0.001 | 0.002 | 0.010 | <0.001 | 0.001 |
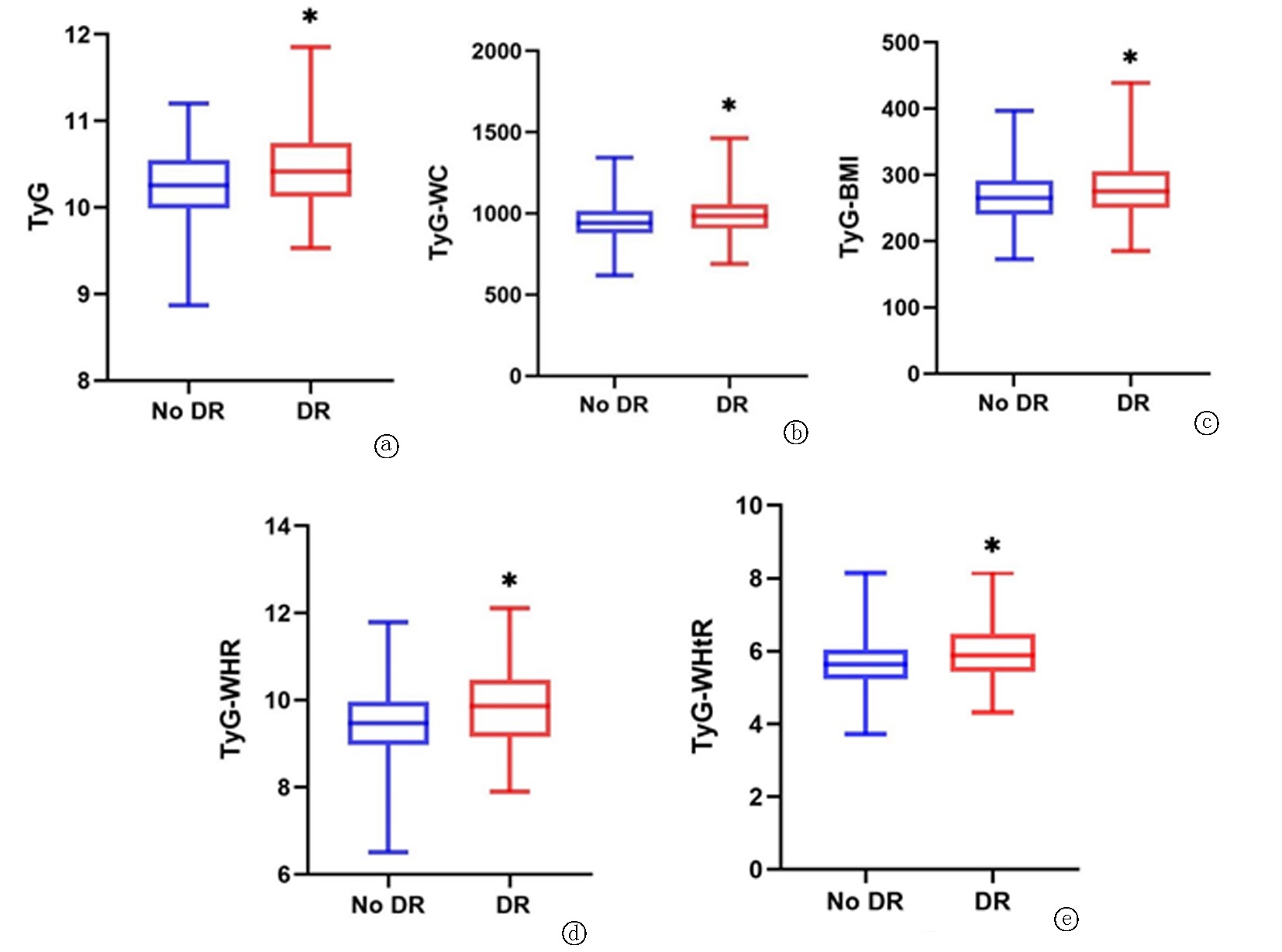
图1 两组TyG及TyG联合肥胖指标的箱式图 a. TyG;b. TyG-WC;c. TyG-BMI;d. TyG-WHR;e. TyG-WHtR。 与非DR组比较,*P<0.05
Fig.1 Box plots of TyG and TyG combined with obesity indicators in the two groups a. TyG; b. TyG-WC; c. TyG-BMI; d. TyG-WHR; e. TyG-WHtR
| T2DM合并DR | ||
|---|---|---|
| P值 | ||
| 年龄(岁) | 0.119 | 0.021 |
| 性别 | 0.033 | 0.528 |
| 糖尿病病程(月) | 0.366 | <0.001 |
| WC(cm) | 0.109 | 0.036 |
| WHR | 0.126 | 0.015 |
| WHtR | 0.125 | 0.016 |
| TC(mmol/L) | 0.071 | 0.173 |
| TG(mmol/L) | 0.120 | 0.020 |
| LDL-C(mmol/L) | 0.066 | 0.205 |
| HDL-C(mmol/L) | -0.083 | 0.108 |
| SCr(mmol/L) | 0.157 | 0.002 |
| BUN(mmol/L) | 0.166 | 0.001 |
| UA(mmol/L) | 0.074 | 0.151 |
| GFR (mL/min) | -0.204 | <0.001 |
| FBG(mmol/L) | 0.148 | 0.004 |
| HbA1c(%) | 0.147 | 0.005 |
| TyG | 0.165 | 0.001 |
| TyG-WC | 0.163 | 0.002 |
| TyG-BMI | 0.134 | 0.010 |
| TyG-WHR | 0.195 | <0.001 |
| TyG-WHtR | 0.178 | 0.001 |
表4 T2DM合并DR与各指标的相关性分析
Tab.4 Correlation analysis between DR and various indicators in T2DM patients
| T2DM合并DR | ||
|---|---|---|
| P值 | ||
| 年龄(岁) | 0.119 | 0.021 |
| 性别 | 0.033 | 0.528 |
| 糖尿病病程(月) | 0.366 | <0.001 |
| WC(cm) | 0.109 | 0.036 |
| WHR | 0.126 | 0.015 |
| WHtR | 0.125 | 0.016 |
| TC(mmol/L) | 0.071 | 0.173 |
| TG(mmol/L) | 0.120 | 0.020 |
| LDL-C(mmol/L) | 0.066 | 0.205 |
| HDL-C(mmol/L) | -0.083 | 0.108 |
| SCr(mmol/L) | 0.157 | 0.002 |
| BUN(mmol/L) | 0.166 | 0.001 |
| UA(mmol/L) | 0.074 | 0.151 |
| GFR (mL/min) | -0.204 | <0.001 |
| FBG(mmol/L) | 0.148 | 0.004 |
| HbA1c(%) | 0.147 | 0.005 |
| TyG | 0.165 | 0.001 |
| TyG-WC | 0.163 | 0.002 |
| TyG-BMI | 0.134 | 0.010 |
| TyG-WHR | 0.195 | <0.001 |
| TyG-WHtR | 0.178 | 0.001 |
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.940 | 0.271 | 12.032 | 0.001 | 2.561 | 1.505 | 4.356 |
| model2 | 1.190 | 0.309 | 14.823 | <0.001 | 3.288 | 1.794 | 6.025 |
| model3 | 0.921 | 0.466 | 3.911 | 0.048 | 2.513 | 1.008 | 6.261 |
表5 T2DM合并DR与TyG的回归分析
Tab.5 Regression analysis of DR and TyG in T2DM patients
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.940 | 0.271 | 12.032 | 0.001 | 2.561 | 1.505 | 4.356 |
| model2 | 1.190 | 0.309 | 14.823 | <0.001 | 3.288 | 1.794 | 6.025 |
| model3 | 0.921 | 0.466 | 3.911 | 0.048 | 2.513 | 1.008 | 6.261 |
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.003 | 0.001 | 11.500 | 0.001 | 1.003 | 1.001 | 1.005 |
| model2 | 0.013 | 0.003 | 15.313 | <0.001 | 1.013 | 1.006 | 1.020 |
| model3 | 0.011 | 0.005 | 4.634 | 0.031 | 1.011 | 1.001 | 1.021 |
表6 T2DM合并DR与TyG-WC的回归分析
Tab.6 Regression analysis of DR and TyG-WC in T2DM patients
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.003 | 0.001 | 11.500 | 0.001 | 1.003 | 1.001 | 1.005 |
| model2 | 0.013 | 0.003 | 15.313 | <0.001 | 1.013 | 1.006 | 1.020 |
| model3 | 0.011 | 0.005 | 4.634 | 0.031 | 1.011 | 1.001 | 1.021 |
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.009 | 0.003 | 10.578 | 0.001 | 1.009 | 1.004 | 1.014 |
| model2 | 0.016 | 0.005 | 11.526 | 0.001 | 1.016 | 1.007 | 1.026 |
| model3 | 0.020 | 0.006 | 11.506 | 0.031 | 1.020 | 1.009 | 1.032 |
表7 T2DM合并DR与TyG-BMI的回归分析
Tab.7 Regression analysis of DR and TyG-BMI in T2DM patients
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.009 | 0.003 | 10.578 | 0.001 | 1.009 | 1.004 | 1.014 |
| model2 | 0.016 | 0.005 | 11.526 | 0.001 | 1.016 | 1.007 | 1.026 |
| model3 | 0.020 | 0.006 | 11.506 | 0.031 | 1.020 | 1.009 | 1.032 |
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.572 | 0.144 | 15.650 | <0.001 | 1.771 | 1.334 | 2.351 |
| model2 | 1.297 | 0.330 | 15.437 | <0.001 | 3.660 | 1.916 | 6.991 |
| model3 | 1.044 | 0.496 | 4.436 | 0.035 | 2.840 | 1.075 | 7.503 |
表8 T2DM合并DR与TyG-WHR的回归分析
Tab.8 Regression analysis of DR and TyG-WHR in T2DM patients
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.572 | 0.144 | 15.650 | <0.001 | 1.771 | 1.334 | 2.351 |
| model2 | 1.297 | 0.330 | 15.437 | <0.001 | 3.660 | 1.916 | 6.991 |
| model3 | 1.044 | 0.496 | 4.436 | 0.035 | 2.840 | 1.075 | 7.503 |
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.594 | 0.162 | 13.374 | <0.001 | 1.811 | 1.317 | 2.490 |
| model2 | 2.135 | 0.549 | 15.108 | <0.001 | 8.455 | 2.882 | 24.810 |
| model3 | 1.793 | 0.833 | 4.632 | 0.031 | 6.008 | 1.174 | 30.751 |
表9 T2DM合并DR与TyG-WHtR的回归分析
Tab.9 Regression analysis of DR and TyG-WHtR in T2DM patients
| 回归 系数 | 标准误 | wald χ2值 | P值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| model1 | 0.594 | 0.162 | 13.374 | <0.001 | 1.811 | 1.317 | 2.490 |
| model2 | 2.135 | 0.549 | 15.108 | <0.001 | 8.455 | 2.882 | 24.810 |
| model3 | 1.793 | 0.833 | 4.632 | 0.031 | 6.008 | 1.174 | 30.751 |
| AUC | 95% | P值 | 敏感度 | 特异性 | 约登指数 | 界值 | ||
|---|---|---|---|---|---|---|---|---|
| 下限 | 上限 | |||||||
| TyG | 0.604 | 0.541 | 0.667 | 0.001 | 0.670 | 0.525 | 0.195 | 10.2834 |
| TyG-WC | 0.603 | 0.540 | 0.666 | 0.002 | 0.473 | 0.713 | 0.186 | 999.6353 |
| TyG-BMI | 0.584 | 0.521 | 0.428 | 0.010 | 0.696 | 0.441 | 0.137 | 259.0222 |
| TyG-WHR | 0.623 | 0.560 | 0.686 | <0.001 | 0.527 | 0.678 | 0.205 | 9.8027 |
| TyG-WHtR | 0.612 | 0.549 | 0.676 | 0.001 | 0.571 | 0.636 | 0.207 | 5.8247 |
表10 各指标对T2DM合并DR的预测价值
Tab.10 Predictive value of each index for DR in T2DM patients
| AUC | 95% | P值 | 敏感度 | 特异性 | 约登指数 | 界值 | ||
|---|---|---|---|---|---|---|---|---|
| 下限 | 上限 | |||||||
| TyG | 0.604 | 0.541 | 0.667 | 0.001 | 0.670 | 0.525 | 0.195 | 10.2834 |
| TyG-WC | 0.603 | 0.540 | 0.666 | 0.002 | 0.473 | 0.713 | 0.186 | 999.6353 |
| TyG-BMI | 0.584 | 0.521 | 0.428 | 0.010 | 0.696 | 0.441 | 0.137 | 259.0222 |
| TyG-WHR | 0.623 | 0.560 | 0.686 | <0.001 | 0.527 | 0.678 | 0.205 | 9.8027 |
| TyG-WHtR | 0.612 | 0.549 | 0.676 | 0.001 | 0.571 | 0.636 | 0.207 | 5.8247 |
| [1] | Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9(th) edition[J]. Diabetes Res Clin Pract, 2019, 157: 107843. |
| [2] | NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants[J]. Lancet, 2016, 387(10027): 1513-1530. |
| [3] | Lin KY, Hsih WH, Lin YB, et al. Update in the epidemiology, risk factors, screening, and treatment of diabetic retinopathy[J]. J Diabetes Investig, 2021, 12(8): 1322-1325. |
| [4] |
Stumvoll M, Goldstein BJ, Van Haeften TW. Type 2 diabetes: Principles of pathogenesis and therapy[J]. Lancet, 2005, 365(9467): 1333-1346.
doi: 10.1016/S0140-6736(05)61032-X pmid: 15823385 |
| [5] |
Wang X, Liu J, Cheng Z, et al. Triglyceride glucose-body mass index and the risk of diabetes: A general population-based cohort study[J]. Lipids Health Dis, 2021, 20(1): 99.
doi: 10.1186/s12944-021-01532-7 pmid: 34488806 |
| [6] |
Zeng ZY, Liu SX, Xu H, et al. Association of triglyceride glucose index and its combination of obesity indices with prehypertension in lean individuals: A cross-sectional study of Chinese adults[J]. J Clin Hypertens (Greenwich), 2020, 22(6): 1025-1032.
doi: 10.1111/jch.13878 pmid: 32442359 |
| [7] |
Sheng G, Lu S, Xie Q, et al. The usefulness of obesity and lipid-related indices to predict the presence of Non-alcoholic fatty liver disease[J]. Lipids Health Dis, 2021, 20(1): 134.
doi: 10.1186/s12944-021-01561-2 pmid: 34629059 |
| [8] | Du Z, Xing L, Lin M, et al. Estimate of prevalent ischemic stroke from triglyceride glucose-body mass index in the general population[J]. BMC Cardiovasc Disord, 2020, 20(1): 483. |
| [9] |
Forbes JM, Fotheringham AK. Vascular complications in diabetes: Old messages, new thoughts[J]. Diabetologia, 2017, 60(11): 2129-2138.
doi: 10.1007/s00125-017-4360-x pmid: 28725914 |
| [10] |
Litwak L, Goh SY, Hussein Z, et al. Prevalence of diabetes complications in people with type 2 diabetes mellitus and its association with baseline characteristics in the multinational A1chieve study[J]. Diabetol Metab Syndr, 2013, 5(1): 57.
doi: 10.1186/1758-5996-5-57 pmid: 24228724 |
| [11] |
Simó-Servat O, Hernández C, Simó R. Diabetic retinopathy in the context of patients with diabetes[J]. Ophthalmic Res, 2019, 62(4): 211-217.
doi: 10.1159/000499541 pmid: 31129667 |
| [12] | Parmar MS. Evaluation and care of patients with diabetic retinopathy[J]. N Engl J Med, 2020, 383(5): e31. |
| [13] | Liu Y, Wu N. Progress of nanotechnology in diabetic retinopathy treatment[J]. Int J Nanomedicine, 2021, 16: 1391-1403. |
| [14] |
Teo ZL, Tham YC, Yu M, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: Systematic review and meta-analysis[J]. Ophthalmology, 2021, 128(11): 1580-1591.
doi: 10.1016/j.ophtha.2021.04.027 pmid: 33940045 |
| [15] |
Stitt AW, Curtis TM, Chen M, et al. The progress in understanding and treatment of diabetic retinopathy[J]. Prog Retin Eye Res, 2016, 51: 156-186.
doi: 10.1016/j.preteyeres.2015.08.001 pmid: 26297071 |
| [16] |
Heintz E, Wiréhn AB, Peebo BB, et al. Prevalence and healthcare costs of diabetic retinopathy: A population-based register study in Sweden[J]. Diabetologia, 2010, 53(10): 2147-2154.
doi: 10.1007/s00125-010-1836-3 pmid: 20596693 |
| [17] | American Diabetes Association. Standards of medical care in diabetes——2006[J]. Diabetes Care, 2006, 29(Suppl 1): S4-42. |
| [18] | Vujosevic S, Aldington SJ, Silva P, et al. Screening for diabetic retinopathy: New perspectives and challenges[J]. Lancet Diabetes Endocrinol, 2020, 8(4): 337-347. |
| [19] | Tung TH, Shih HC, Tsai ST, et al. A community-based study of the relationship between insulin resistance/beta-cell dysfunction and diabetic retinopathy among type II diabetics in Kinmen, Taiwan[J]. Ophthalmic Epidemiol, 2007, 14(3): 148-154. |
| [20] | Sharma VR, Matta ST, Haymond MW, et al. Measuring insulin resistance in humans[J]. Horm Res Paediatr, 2020, 93(11-12): 577-588. |
| [21] |
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects[J]. Metab Syndr Relat Disord, 2008, 6(4): 299-304.
doi: 10.1089/met.2008.0034 pmid: 19067533 |
| [22] | 庞敏, 魏祎, 翁孝刚. 2型糖尿病视网膜病变危险因素分析[J]. 新乡医学院学报, 2020, 37(3):270-273. |
| [23] |
Costagliola C. Oxidative state of glutathione in red blood cells and plasma of diabetic patients: In vivo and in vitro study[J]. Clin Physiol Biochem, 1990, 8(4): 204-210.
pmid: 2078922 |
| [24] |
Ellis TP, Choudhury RH, Kaul K, et al. Diabetic retinopathy and atherosclerosis: Is there a link?[J]. Curr Diabetes Rev, 2013, 9(2): 146-160.
doi: 10.2174/1573399811309020006 pmid: 23094754 |
| [25] | Costagliola C, Romano V, De Tollis M, et al. TNF-alpha levels in tears: A novel biomarker to assess the degree of diabetic retinopathy[J]. Mediators Inflamm, 2013, 2013: 629529. |
| [26] |
Semeraro F, Cancarini A, Morescalchi F, et al. Serum and intraocular concentrations of erythropoietin and vascular endothelial growth factor in patients with type 2 diabetes and proliferative retinopathy[J]. Diabetes Metab, 2014, 40(6): 445-451.
doi: 10.1016/j.diabet.2014.04.005 pmid: 24878492 |
| [27] |
Cancarini A, Costagliola C, Dell'omo R, et al. Effect of intravitreal bevacizumab on serum, aqueous, and vitreous humor levels of erythropoietin in patients with proliferative diabetic retinopathy[J]. Minerva Endocrinol, 2014, 39(4): 305-311.
pmid: 25371057 |
| [28] |
Costagliola C, Daniele A, Dell'omo R, et al. Aqueous humor levels of vascular endothelial growth factor and adiponectin in patients with type 2 diabetes before and after intravitreal bevacizumab injection[J]. Exp Eye Res, 2013, 110: 50-54.
doi: 10.1016/j.exer.2013.02.004 pmid: 23454098 |
| [29] | Tarr JM, Kaul K, Chopra M, et al. Pathophysiology of diabetic retinopathy[J]. ISRN Ophthalmol, 2013, 2013: 343560. |
| [30] | Semeraro F, Cancarini A, Dell'omo R, et al. Diabetic retinopathy: Vascular and inflammatory disease[J]. J Diabetes Res, 2015, 2015: 582060. |
| [31] | Kowluru RA. Diabetic retinopathy and NADPH oxidase-2: A sweet slippery road[J]. Antioxidants (Basel), 2021, 10(5):783. |
| [32] | Er LK, Wu S, Chou HH, et al. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals[J]. PLoS One, 2016, 11(3): e0149731. |
| [33] | Zheng S, Shi S, Ren X, et al. Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: Cross-sectional and prospective cohort study[J]. J Transl Med, 2016, 14(1): 260. |
| [34] |
Vekasi J, Marton ZS, Kesmarky G, et al. Hemorheological alterations in patients with diabetic retinopathy[J]. Clin Hemorheol Microcirc, 2001, 24(1): 59-64.
pmid: 11345235 |
| [35] | Williams MD, Nadler JL. Inflammatory mechanisms of diabetic complications[J]. Curr Diab Rep, 2007, 7(3): 242-248. |
| [36] | Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity[J]. Am J Physiol Cell Physiol, 2021, 320(3): C375-C391. |
| [37] |
El-Asrar AM. Role of inflammation in the pathogenesis of diabetic retinopathy[J]. Middle East Afr J Ophthalmol, 2012, 19(1): 70-74.
doi: 10.4103/0974-9233.92118 pmid: 22346117 |
| [38] |
Van Greevenbroek MM, Schalkwijk CG, Stehouwer CD. Obesity-associated low-grade inflammation in type 2 diabetes mellitus: Causes and consequences[J]. Neth J Med, 2013, 71(4): 174-187.
pmid: 23723111 |
| [39] | Kwon H, Pessin JE. Adipokines mediate inflammation and insulin resistance[J]. Front Endocrinol (Lausanne), 2013, 4: 71. |
| [40] | Fuentes E, Fuentes F, Vilahur G, et al. Mechanisms of chronic state of inflammation as mediators that link obese adipose tissue and metabolic syndrome[J]. Mediators Inflamm, 2013, 2013: 136584. |
| [41] |
Gray N, Picone G, Sloan F, et al. Relation between BMI and diabetes mellitus and its complications among US older adults[J]. South Med J, 2015, 108(1): 29-36.
doi: 10.14423/SMJ.0000000000000214 pmid: 25580754 |
| [42] | Zhu W, Wu Y, Meng YF, et al. Association of obesity and risk of diabetic retinopathy in diabetes patients: A meta-analysis of prospective cohort studies[J]. Medicine (Baltimore), 2018, 97(32): e11807. |
| [43] |
Heymsfield SB, Cefalu WT. Does body mass index adequately convey a patient's mortality risk?[J]. Jama, 2013, 309(1): 87-88.
doi: 10.1001/jama.2012.185445 pmid: 23280230 |
| [44] | Després JP. Body fat distribution and risk of cardiovascular disease: An update[J]. Circulation, 2012, 126(10): 1301-1313. |
| [45] |
Björntorp P. Metabolic implications of body fat distribution[J]. Diabetes Care, 1991, 14(12): 1132-1143.
doi: 10.2337/diacare.14.12.1132 pmid: 1773700 |
| [46] | Masuzaki H, Flier JS. Tissue-specific glucocorticoid reactivating enzyme, 11 beta-hydroxysteroid dehydrogenase type 1 (11 beta-HSD1)--a promising drug target for the treatment of metabolic syndrome[J]. Curr Drug Targets Immune Endocr Metabol Disord, 2003, 3(4): 255-262. |
| [47] |
Blüher M, Engeli S, Klöting N, et al. Dysregulation of the peripheral and adipose tissue endocannabinoid system in human abdominal obesity[J]. Diabetes, 2006, 55(11): 3053-3060.
doi: 10.2337/db06-0812 pmid: 17065342 |
| [48] | Côté M, Matias I, Lemieux I, et al. Circulating endocannabinoid levels, abdominal adiposity and related cardiometabolic risk factors in obese men[J]. Int J Obes (Lond), 2007, 31(4): 692-699. |
| [49] |
Panagiotakos DB, Pitsavos C, Yannakoulia M, et al. The implication of obesity and central fat on markers of chronic inflammation: The ATTICA study[J]. Atherosclerosis, 2005, 183(2): 308-315.
doi: 10.1016/j.atherosclerosis.2005.03.010 pmid: 16285994 |
| [50] |
Man RE, Sabanayagam C, Chiang PP, et al. Differential association of generalized and abdominal obesity with diabetic retinopathy in asian patients with type 2 diabetes[J]. JAMA Ophthalmol, 2016, 134(3): 251-257.
doi: 10.1001/jamaophthalmol.2015.5103 pmid: 26720805 |
| [51] | Van Leiden HA, Dekker JM, Moll AC, et al. Risk factors for incident retinopathy in a diabetic and nondiabetic population: The Hoorn study[J]. Arch Ophthalmol, 2003, 121(2): 245-251. |
| [1] | 易静静, 圈启芳, 马婕. 调节小胶质细胞反应性:糖尿病视网膜病变新见解[J]. 临床荟萃, 2023, 38(4): 364-368. |
| [2] | 王德生, 孙志刚, 马周鹏. 血清超敏C反应蛋白及尿mAlb/Cr与糖尿病视网膜病变的相关性[J]. 临床荟萃, 2022, 37(3): 253-256. |
| [3] | 朱素华, 徐圣秋. 基质金属蛋白酶抑制剂在糖尿病视网膜病变的研究进展[J]. 临床荟萃, 2022, 37(12): 1148-1152. |
| [4] | 佟晶晶1,施克新2,冷飞2,李凤萍2. 血清胆红素水平与2型糖尿病视网膜病变的相关性[J]. 临床荟萃, 2020, 35(9): 816-822. |
| [5] | 江旭,刘尚全. 3 404例2型糖尿病患者视网膜病变患病率及其相关因素分析[J]. 临床荟萃, 2020, 35(1): 54-58. |
| [6] | 路阳,王瑞英,杜雅楠,张筱涵. 中国人群中血糖波动与2型糖尿病视网膜病变关系的meta分析[J]. 临床荟萃, 2020, 35(1): 13-20. |
| [7] | 路阳,王瑞英,杜雅楠,张筱涵. 血糖波动与糖尿病视网膜病变关系的研究进展[J]. 临床荟萃, 2019, 34(11): 1046-1049. |
| [8] | 陈璐;王龙;华飞;项守奎;徐茵;蒋晓红. 2型糖尿病患者血清胱抑素C与视网膜病变的关系[J]. 临床荟萃, 2015, 30(7): 796-798. |
| [9] | 王超;张靖航;彭悦;王鹏华. 高甘油三酯血症腰围表型与2型糖尿病性视网膜病变的相关性[J]. 临床荟萃, 2015, 30(6): 657-659663. |
| [10] | 刘敏;张勉之;朱玉霞;葛进;王丽敏. 血浆chemerin水平与增殖型糖尿病视网膜病变相关[J]. 临床荟萃, 2014, 29(2): 146-148. |
| [11] | 邢邯英;王超;魏聪;张会欣. 通心络对糖尿病小鼠视网膜组织血管内皮生长因子及色素上皮衍生因子表达的影响[J]. 临床荟萃, 2014, 29(12): 1382-1.38414e+007. |
| [12] | 倪雅楠;李强. 视黄醇结合蛋白4与2型糖尿病微血管病变的研究进展[J]. 临床荟萃, 2012, 27(9): 820-822. |
| [13] | 梁丹;王战建. 视黄醇结合蛋白4与2型糖尿病视网膜病变的研究进展[J]. 临床荟萃, 2012, 27(15): 1370-1373. |
| [14] | 刘亚;蒋延旺;许国华. 2型糖尿病视网膜病变与血超敏C反应蛋白和高同型半胱氨酸的关系[J]. 临床荟萃, 2012, 27(11): 967-968. |
| [15] | 姚明言;苏胜偶. 色素上皮衍生因子与氧化应激在糖尿病视网膜病变中的作用[J]. 临床荟萃, 2012, 27(10): 918-920. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||