Clinical Focus ›› 2025, Vol. 40 ›› Issue (1): 54-59.doi: 10.3969/j.issn.1004-583X.2025.01.008
Previous Articles Next Articles
Application value of right heart ultrasound combined with renal vascular doppler score in patients with end-stage renal disease during dialysis
Liu Yia, Zhao Haotiana, Wang Xiaonaa, Liu Yuanlina, Li Lia( ), Wang Zekaib
), Wang Zekaib
- a. Department of Ultrasound; b. Department of Nephrology, Hebei General Hospital,Shijiazhuang 050000,China
-
Received:2024-10-12Online:2025-01-20Published:2025-01-17 -
Contact:Li Li,Email: shrmgnk@126.com
CLC Number:
Cite this article
Liu Yi, Zhao Haotian, Wang Xiaona, Liu Yuanlin, Li Li, Wang Zekai. Application value of right heart ultrasound combined with renal vascular doppler score in patients with end-stage renal disease during dialysis[J]. Clinical Focus, 2025, 40(1): 54-59.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2025.01.008
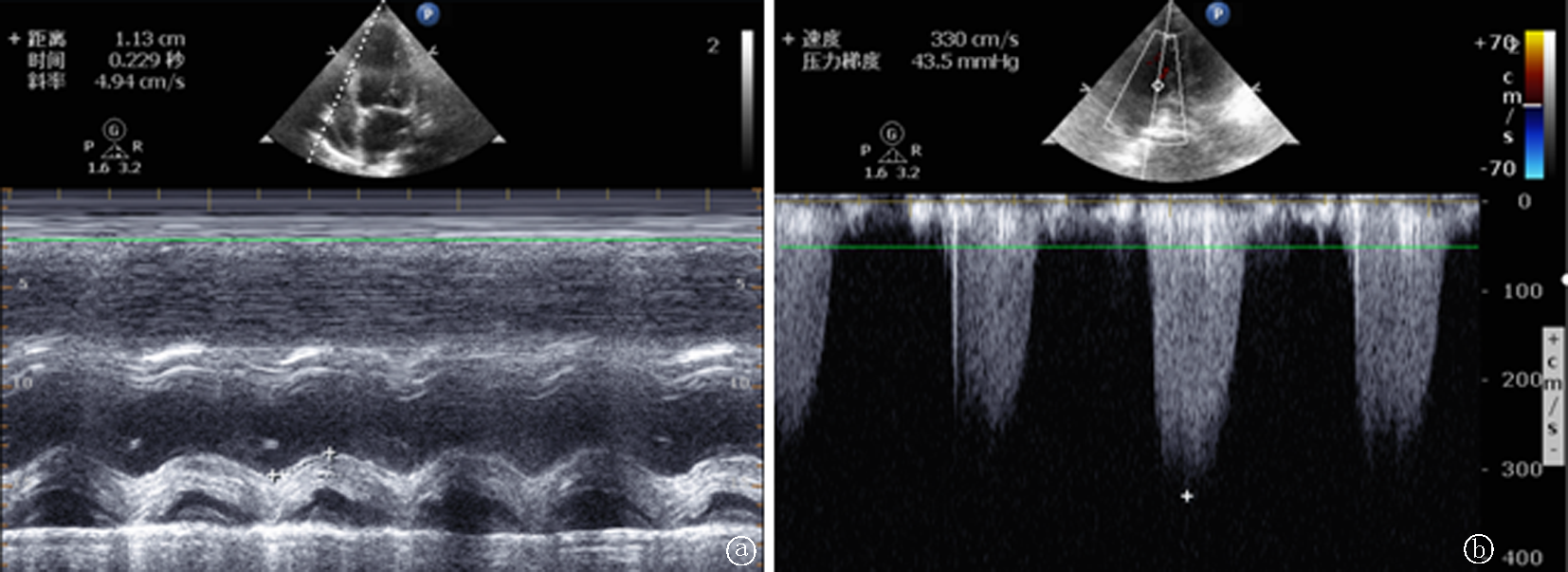
Fig.1 Measurement of ultrasound parameters of right heart function a. the systolic displacement of TAPSE was 11.3 mm; b. the maximum return velocity of the tricuspid valve was 3.3 m/s, and the pulmonary artery systolic pressure was 53 mmHg via Bernoulli equation method (1 mmHg=0.133 kPa)
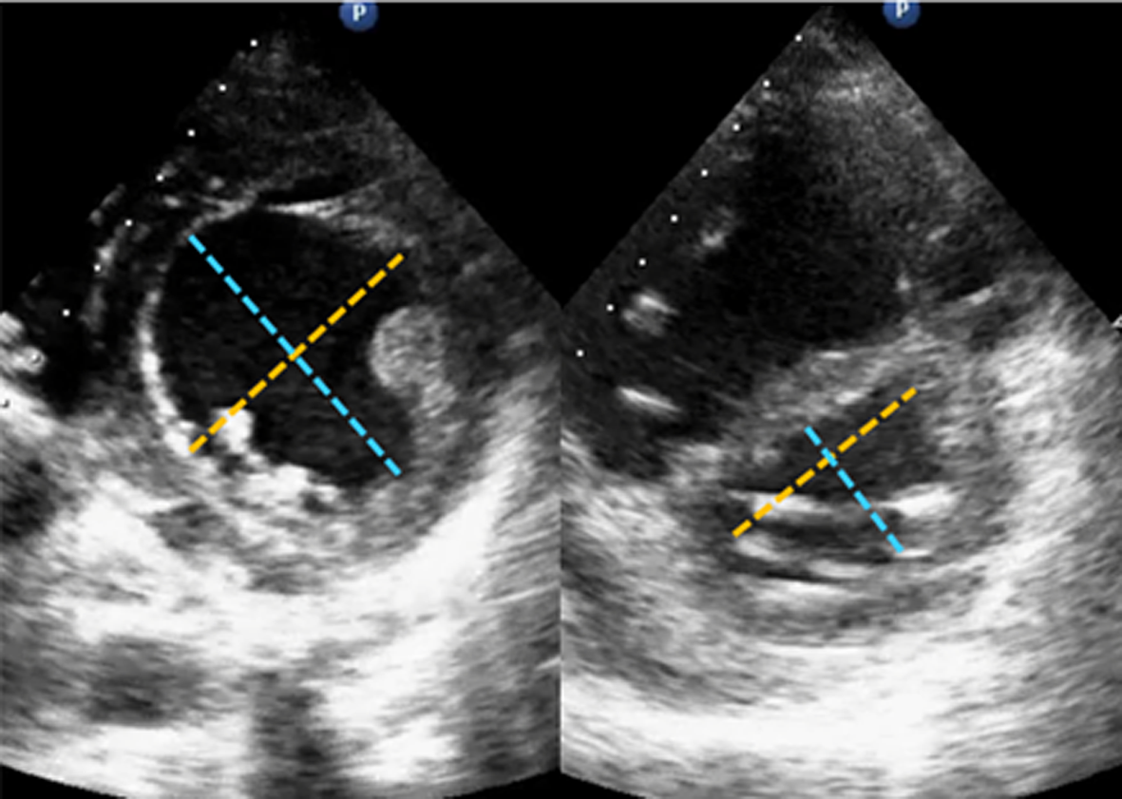
Fig.2 Short-axis eccentric indices measurements of the left ventricle a. the short axis ultrasound section with eccentricity index=transverse diameter (yellow line) / longitudinal diameter (blue line) was 0.97 in the control group; b. which was 1.39 in the dialysis group
| 指标 | 例数 | 年龄 (岁) | 性别[例(%)] | BMI (kg/m2) | 心率 (次/min) | 收缩压 (mmHg) | 舒张压 (mmHg) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | ||||||||||||
| 需透析组 | 21 | 58.81±17.38 | 13(61.9) | 8(38.1) | 23.95(2.56) | 89.71±17.01 | 145.76±21.07 | 84.38±15.28 | |||||
| 对照组 | 25 | 53.20±14.57 | 17(68.0) | 8(32.0) | 25.62(6.89) | 86.68±14.47 | 152.68±20.93 | 87.88±12.47 | |||||
| 统计值 | χ2=0.187 | ||||||||||||
| 0.240 | 0.665 | 0.125 | 0.517 | 0.272 | 0.397 | ||||||||
| 指标 | 肾小球滤过率 (ml/min) | 肌酐 (μmol/L) | WBC (×109/L) | NEUT (%) | 下肢水肿 [例(%)] | ||||||||
| 需透析组 | 7.29±2.98 | 569.60(410.25) | 8.18(5.80) | 81.90(11.40) | 8(38.1) | ||||||||
| 对照组 | 8.53±3.24 | 528.00(372.92) | 6.98(1.83) | 80.20(13.70) | 12(48.0) | ||||||||
| 统计值 | χ2=0.456 | ||||||||||||
| 0.187 | 0.408 | 0.434 | 0.421 | 0.500 | |||||||||
Tab.1 Baseline data between the two groups
| 指标 | 例数 | 年龄 (岁) | 性别[例(%)] | BMI (kg/m2) | 心率 (次/min) | 收缩压 (mmHg) | 舒张压 (mmHg) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | ||||||||||||
| 需透析组 | 21 | 58.81±17.38 | 13(61.9) | 8(38.1) | 23.95(2.56) | 89.71±17.01 | 145.76±21.07 | 84.38±15.28 | |||||
| 对照组 | 25 | 53.20±14.57 | 17(68.0) | 8(32.0) | 25.62(6.89) | 86.68±14.47 | 152.68±20.93 | 87.88±12.47 | |||||
| 统计值 | χ2=0.187 | ||||||||||||
| 0.240 | 0.665 | 0.125 | 0.517 | 0.272 | 0.397 | ||||||||
| 指标 | 肾小球滤过率 (ml/min) | 肌酐 (μmol/L) | WBC (×109/L) | NEUT (%) | 下肢水肿 [例(%)] | ||||||||
| 需透析组 | 7.29±2.98 | 569.60(410.25) | 8.18(5.80) | 81.90(11.40) | 8(38.1) | ||||||||
| 对照组 | 8.53±3.24 | 528.00(372.92) | 6.98(1.83) | 80.20(13.70) | 12(48.0) | ||||||||
| 统计值 | χ2=0.456 | ||||||||||||
| 0.187 | 0.408 | 0.434 | 0.421 | 0.500 | |||||||||
| 指标 | 例数 | RVD (mm) | TAPSE (mm) | S’ (cm/s) | 室间隔 偏心指数 | 三尖瓣最大 反流速度 (m/s) | 肺动脉收缩压 (mmHg) | R-RVDS (分) | L-RVDS (分) |
|---|---|---|---|---|---|---|---|---|---|
| 需透析组 | 21 | 36.43±5.55 | 15.19±3.02 | 12.35±2.52 | 1.06(0.12) | 3.00±0.81 | 47.00(26.50) | 1.26±0.26 | 1.36±0.32 |
| 对照组 | 25 | 31.76±4.42 | 17.86±1.89 | 14.79±2.13 | 1.02(0.05) | 2.57±0.45 | 35.00(15.00) | 1.54±0.43 | 1.60±0.46 |
| 统计值 | |||||||||
| 0.003 | 0.001 | 0.001 | 0.004 | 0.040 | 0.010 | 0.013 | 0.041 |
Tab.2 Ultrasound parameters between the two groups
| 指标 | 例数 | RVD (mm) | TAPSE (mm) | S’ (cm/s) | 室间隔 偏心指数 | 三尖瓣最大 反流速度 (m/s) | 肺动脉收缩压 (mmHg) | R-RVDS (分) | L-RVDS (分) |
|---|---|---|---|---|---|---|---|---|---|
| 需透析组 | 21 | 36.43±5.55 | 15.19±3.02 | 12.35±2.52 | 1.06(0.12) | 3.00±0.81 | 47.00(26.50) | 1.26±0.26 | 1.36±0.32 |
| 对照组 | 25 | 31.76±4.42 | 17.86±1.89 | 14.79±2.13 | 1.02(0.05) | 2.57±0.45 | 35.00(15.00) | 1.54±0.43 | 1.60±0.46 |
| 统计值 | |||||||||
| 0.003 | 0.001 | 0.001 | 0.004 | 0.040 | 0.010 | 0.013 | 0.041 |
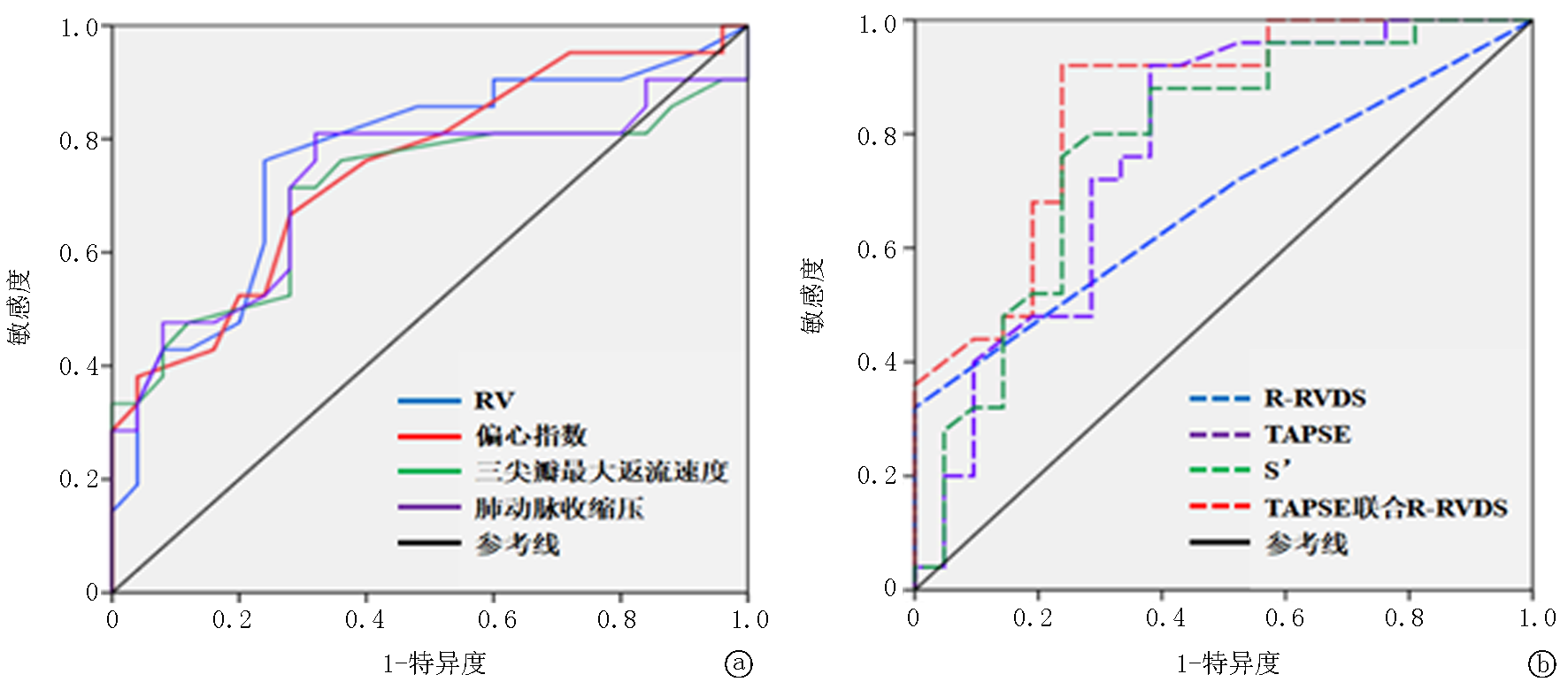
| AUC | 95% | 敏感度 | 特异度 | 界值 | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| RVD | 0.765(0.621~0.908) | 0.002 | 0.621 | 0.908 | 76.2 | 76.0 | 33.50 |
| 室间隔偏心指数 | 0.750(0.607~0.892) | 0.004 | 0.607 | 0.892 | 66.7 | 72.0 | 1.035 |
| TAPSE | 0.770(0.626~0.913) | 0.002 | 0.626 | 0.913 | 92.0 | 61.9 | 15.50 |
| S’ | 0.780(0.640~0.920) | 0.001 | 0.640 | 0.920 | 76.0 | 76.2 | 13.55 |
| 三尖瓣最大反流速度 | 0.707(0.543~0.870) | 0.017 | 0.543 | 0.870 | 71.4 | 72.0 | 2.75 |
| 肺动脉收缩压 | 0.723(0.563~0.883) | 0.010 | 0.563 | 0.883 | 81.0 | 68.0 | 37.50 |
| R-RVDS | 0.682(0.529~0.835) | 0.035 | 0.529 | 0.835 | 32.0 | 100.0 | 1.75 |
| L-RVDS | 0.654(0.495~0.813) | 0.074 | 0.495 | 0.813 | 44.0 | 90.5 | 1.75 |
| TAPSE联合R-RVDS | 0.850(0.736~0.963) | <0.001 | 0.736 | 0.963 | 92.0 | 76.2 | - |
Tab.3 Predictive value of each index for predicting ESRD patients
| AUC | 95% | 敏感度 | 特异度 | 界值 | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| RVD | 0.765(0.621~0.908) | 0.002 | 0.621 | 0.908 | 76.2 | 76.0 | 33.50 |
| 室间隔偏心指数 | 0.750(0.607~0.892) | 0.004 | 0.607 | 0.892 | 66.7 | 72.0 | 1.035 |
| TAPSE | 0.770(0.626~0.913) | 0.002 | 0.626 | 0.913 | 92.0 | 61.9 | 15.50 |
| S’ | 0.780(0.640~0.920) | 0.001 | 0.640 | 0.920 | 76.0 | 76.2 | 13.55 |
| 三尖瓣最大反流速度 | 0.707(0.543~0.870) | 0.017 | 0.543 | 0.870 | 71.4 | 72.0 | 2.75 |
| 肺动脉收缩压 | 0.723(0.563~0.883) | 0.010 | 0.563 | 0.883 | 81.0 | 68.0 | 37.50 |
| R-RVDS | 0.682(0.529~0.835) | 0.035 | 0.529 | 0.835 | 32.0 | 100.0 | 1.75 |
| L-RVDS | 0.654(0.495~0.813) | 0.074 | 0.495 | 0.813 | 44.0 | 90.5 | 1.75 |
| TAPSE联合R-RVDS | 0.850(0.736~0.963) | <0.001 | 0.736 | 0.963 | 92.0 | 76.2 | - |
| [1] |
Cai QJ, Mukku VK, Ahmad M. Coronary artery disease in patients with chronic kidney disease: A clinical update[J]. Curr Cardiol Rev, 2013, 9(4):331-339.
doi: 10.2174/1573403x10666140214122234 pmid: 24527682 |
| [2] |
Bansal N. Evolution of cardiovascular disease during the transition to end-stage renal disease[J]. Semin Nephrol, 2017, 37(2):120-131.
doi: S0270-9295(16)30132-2 pmid: 28410646 |
| [3] | Christiadi D, Chai K, Chuah A, et al. Dynamic survival prediction of end-stage kidney disease using random survival forests for competing risk analysis[J]. Front Med (Lausanne), 2024, 11:1428073. |
| [4] | Ben Khadda Z, Lahmamsi H, El Karmoudi Y, et al. Chronic kidney disease of unknown etiology: A global health threat in rural agricultural communities-prevalence, suspected causes, mechanisms, and prevention strategies[J]. Pathophysiology, 2024, 31(4):761-786. |
| [5] | Arcentales-Vera K, Vera-Mendoza MF, Cevallos-Salas C, et al. Prevalence of cardiovascular instability during hemodialysis therapy in hospitalized patients: A systematic review and meta-analysis[J]. Sci Prog, 2024, 107(4):368504241308982. |
| [6] |
Martensson J, Bellomo R. Does fluid management affect the occurrence of acute kidney injury?[J]. Curr Opin Anaesthesiol, 2017, 30(1):84-91.
doi: 10.1097/ACO.0000000000000407 pmid: 27820741 |
| [7] | 王小亭, 刘大为, 张宏民, 等. 重症右心功能管理专家共识[J]. 中华内科杂志, 2017, 56(12):962-973. |
| [8] | Barozzi L, Valentino M, Santoro A, et al. Renal ultrasonography in critically ill patients[J]. Crit Care Med, 2007, 35(5):S198-S205. |
| [9] |
Levey AS. A decade after the KDOQI CKD guidelines[J]. Am J Kidney Dis, 2012, 60(5):683-685.
doi: 10.1053/j.ajkd.2012.08.019 pmid: 23067628 |
| [10] | 张宏民, 刘大为, 王小亭, 等. 感染性休克患者肾血流评分与肾血管阻力指数的关系[J]. 中华医学杂志, 2014, 94(27):2102-2105. |
| [11] | AbuRahma A, AbuRahma Z. Management of carotid disease in the end-stage renal disease patient[J]. Semin Vasc Surg, 2024, 37(4):427-432. |
| [12] | See EJ, Cullen V. Caring for Australians and New Zealanders with Kidney Impairment (CARI) Guideline Group. Commentary on the 2021 update of the KDIGO clinical practice guideline for management of blood pressure in chronic kidney disease[J]. Nephrology (Carlton), 2025, 30(1):e14414. |
| [13] | Bildacı YD, Korucu B, Oktan MA, et al. The relationship between body mass index changes and mortality in geriatric peritoneal dialysis patients: A case-control study[J]. BMC Nephrol, 2024, 25(1):474. |
| [14] |
Chen X, Wang X, Honore PM, et al. Renal failure in critically ill patients, beware of applying (central venous) pressure on the kidney[J]. Ann Intensive Care, 2018, 8(1):91-97.
doi: 10.1186/s13613-018-0439-x pmid: 30238174 |
| [15] | Venet M, Malik A, Gold S, et al. Impact of right ventricular pressure overload on myocardial stiffness assessed by natural wave imaging[J]. JACC Cardiovasc Imaging, 2024:S1936-878X(24)00284-00285. |
| [16] | Mears J, Kaleem S, Panchamia R, et al. Leveraging the capabilities of AI: Novice neurology-trained operators performing cardiac POCUS in patients with acute brain injury[J]. Neurocrit Care, 2024, 41(2):523-532. |
| [17] |
Li SY, Zhang Y, Shen TT, et al. Measuring of strain parameters reflects changes of right ventricular function before and after thrombolytic therapy in patients with acute pulmonary embolism[J]. Int J Cardiovasc Imaging, 2022, 38(10):2199-2208.
doi: 10.1007/s10554-022-02626-8 pmid: 37726462 |
| [18] | Jentzer JC, Tabi M, Wiley BM, et al. Doppler-derived haemodynamics performed during admission echocardiography predict in-hospital mortality in cardiac intensive care unit patients[J]. Eur Heart J Acute Cardiovasc Care, 2022, 11(8):640-650. |
| [19] |
Darmon M, Schortgen F, Vargas F, et al. Diagnostic accuracy of doppler renal resistive index for reversibility of acute kidney injury in critically ill patients[J]. Intensive Care Med, 2011, 37(1):68-76.
doi: 10.1007/s00134-010-2050-y pmid: 20862450 |
| [20] | Trutin I, Bajic Z, Turudic D, et al. Cystatin C, renal resistance index, and kidney injury molecule-1 are potential early predictors of diabetic kidney disease in children with type 1 diabetes[J]. Front Pediatr, 2022, 10:962048. |
| [21] | Capotondo L, Nicolaii GA, Garosi G. The role of color doppler in acute kidney injury[J]. Arch hal Urol Androl, 2010, 82(4):275-279. |
| [22] | Davis S, Huber D, Murali KM, et al. Elevated renal resistive index is independently predicted by older age, but not by the presence of chronic kidney disease: A retrospective cohort study[J]. Intern Med J, 2022, 52(10):1773-1779. |
| [23] | Golob Janˇciˇc S, Klavž J, Filipiˇc M, et al. Comparison of different eGFR formulas to measured glomerular filtration rate using iohexol in children and adolescents with mild chronic kidney disease[J]. Eur J Pediatr, 2024, 184(1):107. |
| [24] | He P, Liao L. Applicability of creatinine-based glomerular filtration rate assessment equations to patients with neurogenic bladder[J]. Front Physiol, 2024, 15:1501161. |
| [25] | Huang CH, Tsai CJ, Su CC, et al. Accelerated risk of renal disease progression in pre-ESRD patients with proton pump inhibitors use: A nationwide population-based study[J]. BMC Nephrol, 2024, 25(1):469. |
| [1] | Wang Chunjie, Xie Jing, Han Xue, Wu Dan, Chen Jianhua. Effect of individualized hemodialysis on dialysis complications in elderly patients with diabetic nephropathy [J]. Clinical Focus, 2024, 39(4): 332-336. |
| [2] | Liu Meng, Hu Guicai, Yang Zongna, Guo Weiwei, Chen Wanxin. Comparative study on volume load and nutritional status in hemodialysis patients with diabetic kidney disease and non-diabetic kidney disease [J]. Clinical Focus, 2021, 36(4): 332-335. |
| [3] | Wang Chao, Wan Duo, Li Sali, Wang Xi. Evaluation of carotid Doppler ultrasonography in degree and hemodynamics of atherosclerosis of chronic kidney disease [J]. Clinical Focus, 2021, 36(11): 1009-1012. |
| [4] | Shang Qihang, Chen Huaqian. Relationship between eosinophil levels and carotid atherosclerosis in maintenance hemodialysis patients [J]. Clinical Focus, 2021, 36(1): 44-48. |
| [5] | Chen Jianhua, LV Yanhui, Li Ying, Song Jingying, Wang Haifeng, Jia Yingjie, Wang Chunjie. Effects of different blood purification methods on microinflammatory state and procalcitonin in maintenance hemodialysis patients [J]. Clinical Focus, 2020, 35(5): 445-448. |
| [6] | Qi Xueting, Ma Zhigang, Lu Shouyan, Zhao Hui, Qian Rui, Huang Junyue. Effects of cinaclcetcombined with calcitriol on secondary hyperparathyroidism inpatients with maintenance hemodialysis [J]. Clinical Focus, 2020, 35(4): 348-352. |
| [7] | Huang Junyue, Ma Zhigang, Li Yingping, Xue Rong, Huang Wenhui, Jing Xiaojiang. Effects of high-flux hemodialysis combined with L-carnitine treatment on lipid metabolism in uremic patients [J]. Clinical Focus, 2019, 34(3): 253-256. |
| [8] | Feng Zhena, Guo Lana, Dong Chunxiaa, Shi Yanana, Jiao Ronghongb. Clinical analysis of 12 cases of pseudoaneurysm associated with hemodialysis [J]. Clinical Focus, 2019, 34(2): 144-147. |
| [9] | Zhou Xiaochun, Wang Xiaoling, Zhao Pengming, Li Jingjing, Shu Hong, Wang Jianqin. Analysis of the risk factors of death in 167 patients with maintenance hemodialysis [J]. Clinical Focus, 2018, 33(8): 695-699. |
| [10] | Du Shutonga, Wang Ziqianga, Ma Weihuaa, Fang Xiaofanga, Li Weidongb. Effects of parathyroid adenectomy on sleep quality of patients with severe secondary parathyroid hyperthyroidism [J]. Clinical Focus, 2018, 33(3): 217-220. |
| [11] | Shen Lei, Feng Xue, Wang Lihua, Hou Jingjing, Gao Yongning. The Relationship between sclerostin and vascular calcification in maintenance hemodialysis patients [J]. Clinical Focus, 2018, 33(10): 878-882. |
| [12] | Huang Junyue,Ma Zhigang,Xue Rong,Li Yingping,Jing Xiaojiang,Huang Wenhui. Different hemopurification modes on beta 2microglobulin and calciumphosphorous metabolism in maintenance hemodialysis patients [J]. Clinical Focus, 2017, 32(7): 575-578. |
| [13] | Zhou Fanli1, Lu Lan1, Fang Xian1, Long Kai1, Mao Yanqing2, Wu Chunxia1. Characteristics and influencing factors of vascular calcification in maintenance hemodialysis patients [J]. Clinical Focus, 2017, 32(10): 858-860. |
| [14] | Sun Yana,Sun Boa, Yan Guoqianga, Li Shenga, Tian Hongxiaa, Zhang Xua, Wang Yanb. Influence factors analysis on clinical outcomes of elderly patients of hemodialysis with congestive heart failure [J]. Clinical Focus, 2016, 31(10): 1075-1079. |
| [15] | Wei Qing;Liu Hong;Tang Rining;Liu Bicheng. Sevelamer on curative effect and endpoint events in hemodialysis patients--a meta analysis [J]. Clinical Focus, 2015, 30(9): 1008-1.0121e+007. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||