Clinical Focus ›› 2022, Vol. 37 ›› Issue (7): 591-598.doi: 10.3969/j.issn.1004-583X.2022.07.002
Previous Articles Next Articles
Meta analysis on effects of glucocorticoid on the immunotherapy of advanced cancer
Ye Qiana, Ling Zhaia, Liu Shenxianga, Lu Guotaob, Yin Xudonga( )
)
- a. Department of Oncology,Affiliated Hospital of Yangzhou University,Yangzhou,225100,China
b. Department of Gastroenterology,Affiliated Hospital of Yangzhou University,Yangzhou,225100,China
-
Received:2021-02-06Online:2022-07-20Published:2022-08-30 -
Contact:Yin Xudong E-mail:090005@yzu.edu.cn
CLC Number:
Cite this article
Ye Qian, Ling Zhai, Liu Shenxiang, Lu Guotao, Yin Xudong. Meta analysis on effects of glucocorticoid on the immunotherapy of advanced cancer[J]. Clinical Focus, 2022, 37(7): 591-598.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2022.07.002
| 作者 | 发表年份 (年) | 样本量 (例) | 国家 | 中位随访 时间(月) | 疾病 | 分期 | ICI类型 | 研究终点 | (PFS) | (OS) | NOS 评分 |
|---|---|---|---|---|---|---|---|---|---|---|---|
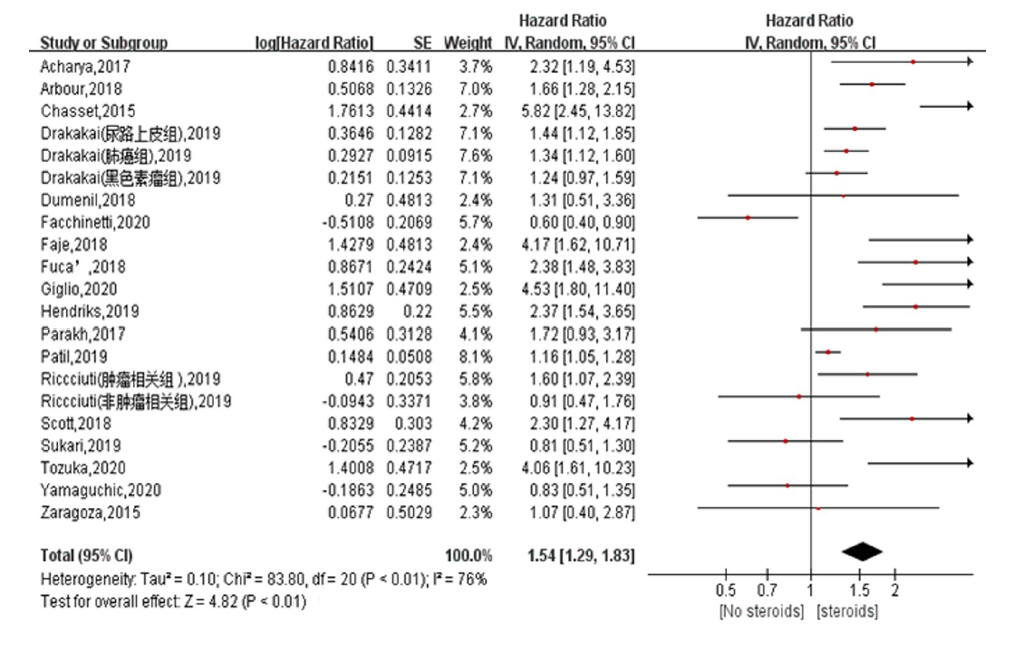
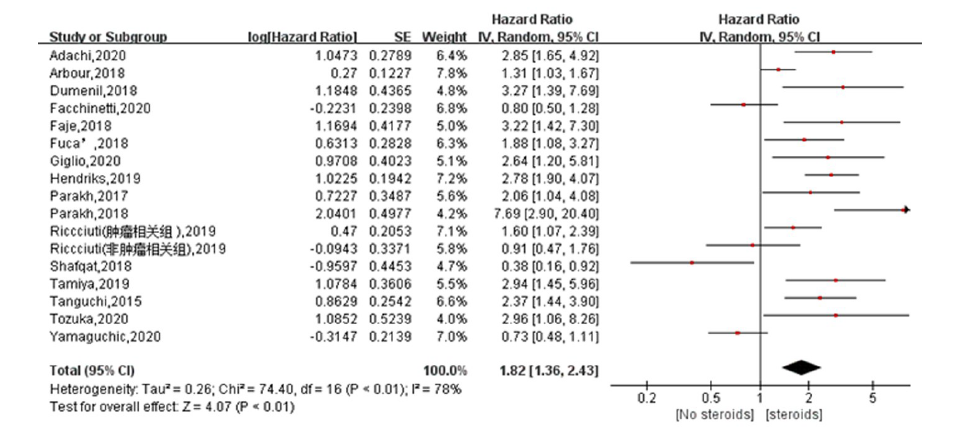
| Arbour[ | 2018 | 640 | 美国 | - | 肺癌 | 进展 | 纳武利尤单抗或帕博利珠单抗或阿特珠单抗或德瓦单抗 | OS/PFS | 1.31 | 1.66 | 7 |
| Parakh[ | 2018 | 45 | 澳大利亚 | 8.7 | 黑色素瘤 | Ⅳ | 纳武利尤单抗+伊匹单抗或者纳武利尤单抗单药 | PFS | 7.69 | - | 7 |
| Tamiya[ | 2019 | 213 | 日本 | 11.0 | 肺癌 | Ⅲ~Ⅳ | 帕博利珠单抗单药 | PFS | 3.161 | - | 7 |
| Riccciuti[ | 2019 | 650 | 美国 | - | 肺癌 | Ⅳ | 抗-PD-L1或者抗-PD-1+抗-CTLA4 | OS/PFS | 1.4/0.62 | 1.6/0.9 | 8 |
| Parakh[ | 2017 | 66 | 澳大利亚 | 7.0 | 黑色素瘤 | Ⅳ | 纳武利尤单抗或帕博利珠单抗 | OS/PFS | 2.06 | 1.72 | 7 |
| Shafqat[ | 2018 | 157 | 美国 | 6.7 | 多种 | Ⅳ | 纳武利尤单抗或帕博利珠单抗或阿特珠单抗 | PFS | 0.383 | - | 6 |
| Tozuka[ | 2020 | 197 | 日本 | 14.3 | 肺癌 | 进展 | 纳武利尤单抗或帕博利珠单抗或阿特珠单抗 | OS/PFS | 2.96 | 4.06 | 7 |
| Sukari[ | 2019 | 168 | 美国 | 26.2 | 多种 | Ⅳ | 纳武利尤单抗+帕博利珠单抗 | OS | - | 0.81 | 8 |
| Adachi[ | 2020 | 296 | 日本 | 22.6 | 肺癌 | Ⅳ | 纳武利尤单抗 | PFS | 2.85 | - | 8 |
| Acharya[ | 2017 | 72 | 美国 | 8.9 | 黑色素瘤 | Ⅳ | 纳武利尤单抗或帕博利珠单抗或伊匹单抗 | OS | - | 2.32 | 8 |
| Scott[ | 2018 | 210 | 美国 | - | 肺癌 | 进展 | 纳武利尤单抗 | OS | - | 2.30 | 6 |
| Fucà[ | 2018 | 151 | 意大利 | 28.6 | 肺癌 | Ⅳ | 抗-PD-L1或抗-PD-1+抗-CTLA4 | OS/PFS | 1.88 | 2.38 | 8 |
| Chasset[ | 2015 | 45 | 法国 | 21.9 | 黑色素瘤 | Ⅲ~Ⅳ | 伊匹单抗 | OS | - | 5.82 | 7 |
| Dumenil[ | 2018 | 65 | 法国 | - | 肺癌 | ⅢB~Ⅳ | 纳武利尤单抗 | OS/PFS | 3.27 | 1.31 | 6 |
| Hendriks[ | 2019 | 1 052 | 法国/荷兰 | 15.8 | 肺癌 | 进展 | 抗-PD-L1或抗-PD-1 | OS/PFS | 2.78 | 2.37 | 7 |
| Tanguchi[ | 2015 | 201 | 日本 | - | 肺癌 | Ⅳ | 纳武利尤单抗 | PFS | 2.37 | - | 6 |
| Zaragoza[ | 2015 | 58 | 法国 | 31.0 | 黑色素瘤 | Ⅲ~Ⅳ | 伊匹单抗 | OS | - | 1.07 | 6 |
| Yamaguchic[ | 2020 | 131 | 日本 | 11.1 | 肺癌 | Ⅲ~Ⅳ | 纳武利尤单抗或帕博利珠单抗 | OS/PFS | 0.73 | 0.83 | 6 |
| Faje[ | 2018 | 98 | 美国 | - | 黑色素瘤 | Ⅳ | 伊匹单抗 | OS/PFS | 3.22 | 4.17 | 6 |
| Giglio[ | 2020 | 413 | 法国 | 24.4 | 肺癌 | ⅢB~Ⅳ | 抗-PD-L1 | OS/PFS | 2.64 | 4.53 | 8 |
| Facchinetti[ | 2020 | 153 | 法国 | 18.2 | 肺癌 | ⅢB~Ⅳ | 帕博利珠单抗 | OS/PFS | 0.8 | 0.6 | 7 |
| Patil[ | 2019 | 11 143 | 美国 | - | 肺癌 | 进展 | - | OS | - | 1.16 | 6 |
| Drakaki[ | 2019 | 2 213 | 美国 | - | 多种 | 进展 | - | OS | - | 1.34/1.24/1.44 | 6 |
| 作者 | 发表年份 (年) | 样本量 (例) | 国家 | 中位随访 时间(月) | 疾病 | 分期 | ICI类型 | 研究终点 | (PFS) | (OS) | NOS 评分 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Arbour[ | 2018 | 640 | 美国 | - | 肺癌 | 进展 | 纳武利尤单抗或帕博利珠单抗或阿特珠单抗或德瓦单抗 | OS/PFS | 1.31 | 1.66 | 7 |
| Parakh[ | 2018 | 45 | 澳大利亚 | 8.7 | 黑色素瘤 | Ⅳ | 纳武利尤单抗+伊匹单抗或者纳武利尤单抗单药 | PFS | 7.69 | - | 7 |
| Tamiya[ | 2019 | 213 | 日本 | 11.0 | 肺癌 | Ⅲ~Ⅳ | 帕博利珠单抗单药 | PFS | 3.161 | - | 7 |
| Riccciuti[ | 2019 | 650 | 美国 | - | 肺癌 | Ⅳ | 抗-PD-L1或者抗-PD-1+抗-CTLA4 | OS/PFS | 1.4/0.62 | 1.6/0.9 | 8 |
| Parakh[ | 2017 | 66 | 澳大利亚 | 7.0 | 黑色素瘤 | Ⅳ | 纳武利尤单抗或帕博利珠单抗 | OS/PFS | 2.06 | 1.72 | 7 |
| Shafqat[ | 2018 | 157 | 美国 | 6.7 | 多种 | Ⅳ | 纳武利尤单抗或帕博利珠单抗或阿特珠单抗 | PFS | 0.383 | - | 6 |
| Tozuka[ | 2020 | 197 | 日本 | 14.3 | 肺癌 | 进展 | 纳武利尤单抗或帕博利珠单抗或阿特珠单抗 | OS/PFS | 2.96 | 4.06 | 7 |
| Sukari[ | 2019 | 168 | 美国 | 26.2 | 多种 | Ⅳ | 纳武利尤单抗+帕博利珠单抗 | OS | - | 0.81 | 8 |
| Adachi[ | 2020 | 296 | 日本 | 22.6 | 肺癌 | Ⅳ | 纳武利尤单抗 | PFS | 2.85 | - | 8 |
| Acharya[ | 2017 | 72 | 美国 | 8.9 | 黑色素瘤 | Ⅳ | 纳武利尤单抗或帕博利珠单抗或伊匹单抗 | OS | - | 2.32 | 8 |
| Scott[ | 2018 | 210 | 美国 | - | 肺癌 | 进展 | 纳武利尤单抗 | OS | - | 2.30 | 6 |
| Fucà[ | 2018 | 151 | 意大利 | 28.6 | 肺癌 | Ⅳ | 抗-PD-L1或抗-PD-1+抗-CTLA4 | OS/PFS | 1.88 | 2.38 | 8 |
| Chasset[ | 2015 | 45 | 法国 | 21.9 | 黑色素瘤 | Ⅲ~Ⅳ | 伊匹单抗 | OS | - | 5.82 | 7 |
| Dumenil[ | 2018 | 65 | 法国 | - | 肺癌 | ⅢB~Ⅳ | 纳武利尤单抗 | OS/PFS | 3.27 | 1.31 | 6 |
| Hendriks[ | 2019 | 1 052 | 法国/荷兰 | 15.8 | 肺癌 | 进展 | 抗-PD-L1或抗-PD-1 | OS/PFS | 2.78 | 2.37 | 7 |
| Tanguchi[ | 2015 | 201 | 日本 | - | 肺癌 | Ⅳ | 纳武利尤单抗 | PFS | 2.37 | - | 6 |
| Zaragoza[ | 2015 | 58 | 法国 | 31.0 | 黑色素瘤 | Ⅲ~Ⅳ | 伊匹单抗 | OS | - | 1.07 | 6 |
| Yamaguchic[ | 2020 | 131 | 日本 | 11.1 | 肺癌 | Ⅲ~Ⅳ | 纳武利尤单抗或帕博利珠单抗 | OS/PFS | 0.73 | 0.83 | 6 |
| Faje[ | 2018 | 98 | 美国 | - | 黑色素瘤 | Ⅳ | 伊匹单抗 | OS/PFS | 3.22 | 4.17 | 6 |
| Giglio[ | 2020 | 413 | 法国 | 24.4 | 肺癌 | ⅢB~Ⅳ | 抗-PD-L1 | OS/PFS | 2.64 | 4.53 | 8 |
| Facchinetti[ | 2020 | 153 | 法国 | 18.2 | 肺癌 | ⅢB~Ⅳ | 帕博利珠单抗 | OS/PFS | 0.8 | 0.6 | 7 |
| Patil[ | 2019 | 11 143 | 美国 | - | 肺癌 | 进展 | - | OS | - | 1.16 | 6 |
| Drakaki[ | 2019 | 2 213 | 美国 | - | 多种 | 进展 | - | OS | - | 1.34/1.24/1.44 | 6 |
| 作者 | 样本量 (例) | GC种类 | 使用时间窗 | 剂量 | 治疗目的 |
|---|---|---|---|---|---|
| Arbour[ | 90 | 强的松 | ICI治疗前30天到开始治疗后 | >10 mg vs <10 mg | 肿瘤相关症状 |
| Parakh[ | 13 | 强的松或地塞米松 | - | ≥10 mg/d或2~8 mg | NS |
| Tamiya[ | 14 | - | ICI开始治疗后 | - | NS |
| Riccciuti[ | 93 | 强的松 | ICI开始治疗后 | >10 mg vs <10 mg | 肿瘤相关症状/非肿瘤相关症状 |
| Parakh[ | 15 | 地塞米松 | ICI开始治疗后 | 0.5~12 mg | 肿瘤相关症状(BMS) |
| Shafqat[ | 21 | 强的松 | 平均8.5周 | - | 非肿瘤相关症状(irAEs) |
| Tozuka[ | 4 | 强的松 | ICI开始治疗后 | 10 mg | 肿瘤相关症状 |
| Sukari[ | 77 | - | - | - | 非肿瘤相关症状(irAEs) |
| Adachi[ | 30 | - | ICI开始治疗后 | - | 肿瘤相关症状(60%)/非肿瘤相关症状(30%) |
| Acharya[ | 21 | 地塞米松 | ICI开始治疗后 | 4 mg/d或4 mg/6~12 h | 肿瘤相关症状(90%) |
| Scott[ | 66 | 强的松 | ICI开始治疗后 | ≥10 mg/d | 肿瘤相关症状/非肿瘤相关症状 |
| Fuca[ | 35 | 强的松 | ICI开始治疗后28天内 | 中位数280 mg(20~875 mg) | 肿瘤相关症状/非肿瘤相关症状 |
| Chasset[ | 12 | 强的松 | ICI开始治疗后30天内 | 平均数0.6 mg/kg(0.2~1.2 mg/kg) | 肿瘤相关症状(BMS) |
| Dumenil[ | 10 | - | ICI开始治疗前1周 | 中位数25 mg(12.5~37.5 mg) | 肿瘤相关症状(BMS) |
| Hendriks[ | 141 | - | ICI开始治疗后 | - | 肿瘤相关症状(BMS) |
| Tanguchi[ | 12 | - | - | 中位数6.25 mg(1.56~12.5 mg) | 肿瘤相关症状/非肿瘤相关症状 |
| Zaragoza[ | 15 | - | ICI开始治疗前 | - | - |
| Yamaguchic[ | NR | - | - | - | 非肿瘤相关症状(irAEs) |
| Faje[ | 64 | 强的松 | ICI开始治疗后 | 22.4 mg vs 5 mg | 非肿瘤相关症状(irAEs) |
| Giglio[ | 114 | 强的松 | ICI开始治疗后8周 | ≥10 mg | 肿瘤相关症状/非肿瘤相关症状 |
| Facchinetti[ | 47 | 强的松 | ICI开始治疗后 | ≥10 mg/d | NS |
| Patil[ | 1581 | 强的松 | ICI开始治疗后30内 | ≥10 mg | NS |
| Drakaki[ | 556 | - | ICI治疗前14天到开始治疗后30天内 | - | 肿瘤相关症状 |
| 作者 | 样本量 (例) | GC种类 | 使用时间窗 | 剂量 | 治疗目的 |
|---|---|---|---|---|---|
| Arbour[ | 90 | 强的松 | ICI治疗前30天到开始治疗后 | >10 mg vs <10 mg | 肿瘤相关症状 |
| Parakh[ | 13 | 强的松或地塞米松 | - | ≥10 mg/d或2~8 mg | NS |
| Tamiya[ | 14 | - | ICI开始治疗后 | - | NS |
| Riccciuti[ | 93 | 强的松 | ICI开始治疗后 | >10 mg vs <10 mg | 肿瘤相关症状/非肿瘤相关症状 |
| Parakh[ | 15 | 地塞米松 | ICI开始治疗后 | 0.5~12 mg | 肿瘤相关症状(BMS) |
| Shafqat[ | 21 | 强的松 | 平均8.5周 | - | 非肿瘤相关症状(irAEs) |
| Tozuka[ | 4 | 强的松 | ICI开始治疗后 | 10 mg | 肿瘤相关症状 |
| Sukari[ | 77 | - | - | - | 非肿瘤相关症状(irAEs) |
| Adachi[ | 30 | - | ICI开始治疗后 | - | 肿瘤相关症状(60%)/非肿瘤相关症状(30%) |
| Acharya[ | 21 | 地塞米松 | ICI开始治疗后 | 4 mg/d或4 mg/6~12 h | 肿瘤相关症状(90%) |
| Scott[ | 66 | 强的松 | ICI开始治疗后 | ≥10 mg/d | 肿瘤相关症状/非肿瘤相关症状 |
| Fuca[ | 35 | 强的松 | ICI开始治疗后28天内 | 中位数280 mg(20~875 mg) | 肿瘤相关症状/非肿瘤相关症状 |
| Chasset[ | 12 | 强的松 | ICI开始治疗后30天内 | 平均数0.6 mg/kg(0.2~1.2 mg/kg) | 肿瘤相关症状(BMS) |
| Dumenil[ | 10 | - | ICI开始治疗前1周 | 中位数25 mg(12.5~37.5 mg) | 肿瘤相关症状(BMS) |
| Hendriks[ | 141 | - | ICI开始治疗后 | - | 肿瘤相关症状(BMS) |
| Tanguchi[ | 12 | - | - | 中位数6.25 mg(1.56~12.5 mg) | 肿瘤相关症状/非肿瘤相关症状 |
| Zaragoza[ | 15 | - | ICI开始治疗前 | - | - |
| Yamaguchic[ | NR | - | - | - | 非肿瘤相关症状(irAEs) |
| Faje[ | 64 | 强的松 | ICI开始治疗后 | 22.4 mg vs 5 mg | 非肿瘤相关症状(irAEs) |
| Giglio[ | 114 | 强的松 | ICI开始治疗后8周 | ≥10 mg | 肿瘤相关症状/非肿瘤相关症状 |
| Facchinetti[ | 47 | 强的松 | ICI开始治疗后 | ≥10 mg/d | NS |
| Patil[ | 1581 | 强的松 | ICI开始治疗后30内 | ≥10 mg | NS |
| Drakaki[ | 556 | - | ICI治疗前14天到开始治疗后30天内 | - | 肿瘤相关症状 |
| 项目 | 例数 | OS | | | PFS | | |
|---|---|---|---|---|---|---|---|
| 癌种 | |||||||
| 非小细胞肺癌 | 15 | 1.49(1.2~1.86) | 0.0003 | 79% | 1.75(1.31~2.34) | 0.0001 | 76% |
| 黑色素瘤 | 7 | 2.12(1.28~3.5) | 0.004 | 73% | 3.47(1.68~7.16) | 0.0008 | 57% |
| 尿路上皮癌 | 1 | 1.44(1.12~1.89) | - | - | - | - | - |
| ICI类型 | |||||||
| 抗PD-1/PD-L1 | 14 | 1.54(1.06~2.26) | 0.03 | 81% | 1.72(1.21~2.45) | 0.003 | 81% |
| 抗CTLA-4 | 3 | 3.02(1.12~8.18) | 0.03 | 71% | 3.22(1.42~7.3) | 0.005 | 81% |
| 其他 | 6 | 1.32(1.15~1.52) | <0.01 | 51% | 1.95(1.04~3.65) | 0.04 | 77% |
| 适应证 | |||||||
| 肿瘤相关症状 | 8 | 2.14(1.62~2.81) | <0.01 | 26% | 2.26(1.72~2.96) | <0.01 | 18% |
| 非肿瘤相关症状 | 5 | 1.13(0.65~1.96) | 0.68 | 70% | 0.94(0.46~1.93) | 0.87 | 78% |
| 国家 | |||||||
| 亚洲 | 2 | 1.74(0.37~8.24) | 0.48 | 89% | 2.04(1.07~3.9) | 0.03 | 83% |
| 欧洲 | 7 | 1.95(1.03~3.67) | 0.04 | 86% | 1.80(0.96~3.36) | 0.07 | 83% |
| 美洲 | 9 | 1.39(1.2~1.63) | <0.01 | 63% | 1.24(0.37~8.24) | 0.34 | 72% |
| 澳洲 | 2 | 1.72(0.93~3.17) | 0.05 | - | 3.79(1.05~13.75) | 0.04 | 79% |
| 研究类型 | |||||||
| 单中心 | 10 | 1.91(1.25~2.93) | 0.003 | 77% | 1.59(1.01~2.50) | 0.04 | 71% |
| 多中心 | 13 | 1.28(1.09~1.50) | 0.003 | 67% | 2.01(1.35~2.99) | 0.006 | 83% |
| 项目 | 例数 | OS | | | PFS | | |
|---|---|---|---|---|---|---|---|
| 癌种 | |||||||
| 非小细胞肺癌 | 15 | 1.49(1.2~1.86) | 0.0003 | 79% | 1.75(1.31~2.34) | 0.0001 | 76% |
| 黑色素瘤 | 7 | 2.12(1.28~3.5) | 0.004 | 73% | 3.47(1.68~7.16) | 0.0008 | 57% |
| 尿路上皮癌 | 1 | 1.44(1.12~1.89) | - | - | - | - | - |
| ICI类型 | |||||||
| 抗PD-1/PD-L1 | 14 | 1.54(1.06~2.26) | 0.03 | 81% | 1.72(1.21~2.45) | 0.003 | 81% |
| 抗CTLA-4 | 3 | 3.02(1.12~8.18) | 0.03 | 71% | 3.22(1.42~7.3) | 0.005 | 81% |
| 其他 | 6 | 1.32(1.15~1.52) | <0.01 | 51% | 1.95(1.04~3.65) | 0.04 | 77% |
| 适应证 | |||||||
| 肿瘤相关症状 | 8 | 2.14(1.62~2.81) | <0.01 | 26% | 2.26(1.72~2.96) | <0.01 | 18% |
| 非肿瘤相关症状 | 5 | 1.13(0.65~1.96) | 0.68 | 70% | 0.94(0.46~1.93) | 0.87 | 78% |
| 国家 | |||||||
| 亚洲 | 2 | 1.74(0.37~8.24) | 0.48 | 89% | 2.04(1.07~3.9) | 0.03 | 83% |
| 欧洲 | 7 | 1.95(1.03~3.67) | 0.04 | 86% | 1.80(0.96~3.36) | 0.07 | 83% |
| 美洲 | 9 | 1.39(1.2~1.63) | <0.01 | 63% | 1.24(0.37~8.24) | 0.34 | 72% |
| 澳洲 | 2 | 1.72(0.93~3.17) | 0.05 | - | 3.79(1.05~13.75) | 0.04 | 79% |
| 研究类型 | |||||||
| 单中心 | 10 | 1.91(1.25~2.93) | 0.003 | 77% | 1.59(1.01~2.50) | 0.04 | 71% |
| 多中心 | 13 | 1.28(1.09~1.50) | 0.003 | 67% | 2.01(1.35~2.99) | 0.006 | 83% |
| [1] |
Nadal E, Massuti B, Dómine M, et al. Immunotherapy with checkpoint inhibitors in non-small cell lung cancer: Insights from long-term survivors[J]. Cancer Immunol Immunother, 2019, 68(3): 341-352.
doi: 10.1007/s00262-019-02310-2 pmid: 30725206 |
| [2] |
Queirolo P, Boutros A, Tanda E, et al. Immune-checkpoint inhibitors for the treatment of metastatic melanoma: A model of cancer immunotherapy[J]. Semin Cancer Biol, 2019, 59:290-297.
doi: S1044-579X(19)30195-6 pmid: 31430555 |
| [3] | Vassilakopoulos TP, Chatzidimitriou C, Asimakopoulos JV, et al. Immunotherapy in hodgkin lymphoma: Present status and future strategies[J]. Cancers (Basel), 2019, 11(8): 1071. |
| [4] |
Reck M, Taylor F, Penrod JR, et al. Impact of nivolumab versus docetaxel on health-related quality of life and symptoms in patients with advanced squamous non-small cell lung cancer: Results from the checkmate 017 study[J]. J Thorac Oncol, 2018, 13(2): 194-204.
doi: S1556-0864(17)32878-2 pmid: 29129758 |
| [5] |
Barlesi F, Garon EB, Kim DW, et al. Health-related quality of life in KEYNOTE-010: A phase Ⅱ/Ⅲ study of pembrolizumab versus docetaxel in patients with previously treated advanced, programmed death ligand 1-expressing NSCLC[J]. J Thorac Oncol, 2019, 14(5): 793-801.
doi: 10.1016/j.jtho.2019.01.016 URL |
| [6] |
Mazieres J, Rittmeyer A, Gadgeel S, et al. Atezolizumab versus docetaxel in pretreated patients with NSCLC: Final results from the randomized phase 2 POPLAR and phase 3 OAK clinical trials[J]. J Thorac Oncol, 2021, 16(1): 140-150.
doi: 10.1016/j.jtho.2020.09.022 pmid: 33166718 |
| [7] |
El Kaddissi A, Basse C. Nouvelles AMMs: durvalumab-En première ligne métastatique dans le cancer bronchique à petites cellules [New European approvals: Durvalumab-In first line metastatic small-cell lung cancer][J]. Bull Cancer, 2020, 107(12): 1208-1209.
doi: 10.1016/j.bulcan.2020.10.003 URL |
| [8] |
Arbour KC, Mezquita L, Long N, et al. Impact of baseline steroids on efficacy of programmed cell death-1 and programmed death-ligand 1 blockade in patients with non-small-cell lung cancer[J]. J Clin Oncol, 2018, 36(28): 2872-2878.
doi: 10.1200/JCO.2018.79.0006 pmid: 30125216 |
| [9] |
Wenker EP, Dupree JM, Langille GM, et al. The use of HCG-based combination therapy for recovery of spermatogenesis after testosterone use[J]. J Sex Med, 2015, 12(6): 1334-1337.
doi: 10.1111/jsm.12890 URL |
| [10] |
Pinato DJ, Kaseb A, Wang Y, et al. Impact of corticosteroid therapy on the outcomes of hepatocellular carcinoma treated with immune checkpoint inhibitor therapy[J]. J Immunother Cancer, 2020, 8(2) :e000726.
doi: 10.1136/jitc-2020-000726 URL |
| [11] | Parakh S, Randhawa M, Nguyen B, et al. Real-world efficacy and toxicity of combined nivolumab and ipilimumab in patients with metastatic melanoma[J]. Asia Pac J Clin Oncol, 2019, 15(1): 26-30. |
| [12] |
Tamiya M, Tamiya A, Hosoya K, et al. Efficacy and safety of pembrolizumab as first-line therapy in advanced non-small cell lung cancer with at least 50% PD-L1 positivity: A multicenter retrospective cohort study (HOPE-001)[J]. Invest New Drugs, 2019, 37(6): 1266-1273.
doi: 10.1007/s10637-019-00843-y URL |
| [13] |
Ricciuti B, Dahlberg SE, Adeni A, et al. Immune checkpoint inhibitor outcomes for patients with non-small-cell lung cancer receiving baseline corticosteroids for palliative versus nonpalliative indications[J]. J Clin Oncol, 2019, 37(22): 1927-1934.
doi: 10.1200/JCO.19.00189 pmid: 31206316 |
| [14] |
Parakh S, Park JJ, Mendis S, et al. Efficacy of anti-PD-1 therapy in patients with melanoma brain metastases[J]. Br J Cancer, 2017, 116(12): 1558-1563.
doi: 10.1038/bjc.2017.142 URL |
| [15] |
Shafqat H, Gourdin T, Sion A. Immune-related adverse events are linked with improved progression-free survival in patients receiving anti-PD-1/PD-L1 therapy[J]. Semin Oncol, 2018, 45(3): 156-163.
doi: S0093-7754(18)30009-5 pmid: 30348532 |
| [16] |
Tozuka T, Kitazono S, Sakamoto H, et al. Poor efficacy of anti-programmed cell death-1/ligand 1 monotherapy for non-small cell lung cancer patients with active brain metastases[J]. Thorac Cancer, 2020, 11(9): 2465-2472.
doi: 10.1111/1759-7714.13557 URL |
| [17] |
Sukari A, Nagasaka M, Alhasan R, et al. Cancer site and adverse events induced by immune checkpoint inhibitors: A retrospective analysis of real-life experience at a single institution[J]. Anticancer Res, 2019, 39(2): 781-790.
doi: 10.21873/anticanres.13175 pmid: 30711957 |
| [18] |
Adachi Y, Tamiya A, Taniguchi Y, et al. Predictive factors for progression-free survival in non-small cell lung cancer patients receiving nivolumab based on performance status[J]. Cancer Med, 2020, 9(4): 1383-1391.
doi: 10.1002/cam4.2807 URL |
| [19] |
Acharya S, Mahmood M, Mullen D, et al. Distant intracranial failure in melanoma brain metastases treated with stereotactic radiosurgery in the era of immunotherapy and targeted agents[J]. Adv Radiat Oncol, 2017, 2(4): 572-580.
doi: 10.1016/j.adro.2017.07.003 pmid: 29204524 |
| [20] |
Scott SC, Pennell NA. Early use of systemic corticosteroids in patients with advanced NSCLC treated with nivolumab[J]. J Thorac Oncol, 2018, 13(11): 1771-1775.
doi: S1556-0864(18)30711-1 pmid: 29935305 |
| [21] | Fucà G, Galli G, Poggi M, et al. Modulation of peripheral blood immune cells by early use of steroids and its association with clinical outcomes in patients with metastatic non-small cell lung cancer treated with immune checkpoint inhibitors[J]. ESMO Open, 2019, 4(1): e000457. |
| [22] |
Chasset F, Pages C, Biard L, et al. Single-center study under a French Temporary Authorization for Use (TAU) protocol for ipilimumab in metastatic melanoma: Negative impact of baseline corticosteroids[J]. Eur J Dermatol, 2015, 25(1): 36-44.
doi: 10.1684/ejd.2014.2471 pmid: 25500362 |
| [23] | Dumenil C, Massiani MA, Dumoulin J, et al. Clinical factors associated with early progression and grade 3-4 toxicity in patients with advanced non-small-cell lung cancers treated with nivolumab[J]. PLoS One, 2018, 13(4): e0195945. |
| [24] |
Hendriks LEL, Henon C, Auclin E, et al. Outcome of patients with non-small cell lung cancer and brain metastases treated with checkpoint inhibitors[J]. J Thorac Oncol, 2019, 14(7): 1244-1254.
doi: S1556-0864(19)30117-0 pmid: 30780002 |
| [25] |
Taniguchi Y, Tamiya A, Isa SI, et al. Predictive factors for poor progression-free survival in patients with non-small cell lung cancer treated with nivolumab[J]. Anticancer Res, 2017, 37(10): 5857-5862.
pmid: 28982912 |
| [26] |
Zaragoza J, Caille A, Beneton N, et al. High neutrophil to lymphocyte ratio measured before starting ipilimumab treatment is associated with reduced overall survival in patients with melanoma[J]. Br J Dermatol, 2016, 174(1): 146-151.
doi: 10.1111/bjd.14155 pmid: 26343230 |
| [27] |
Yamaguchi O, Imai H, Minemura H, et al. Efficacy and safety of immune checkpoint inhibitor monotherapy in pretreated elderly patients with non-small cell lung cancer[J]. Cancer Chemother Pharmacol, 2020, 85(4): 761-771.
doi: 10.1007/s00280-020-04055-7 URL |
| [28] |
Faje AT, Lawrence D, Flaherty K, et al. High-dose glucocorticoids for the treatment of ipilimumab-induced hypophysitis is associated with reduced survival in patients with melanoma[J]. Cancer, 2018, 124(18): 3706-3714.
doi: 10.1002/cncr.31629 pmid: 29975414 |
| [29] | de Giglio A, Mezquita L, Auclin E, et al. Impact of intercurrent introduction of steroids on clinical outcomes in advanced non-small-cell lung cancer (NSCLC) patients under immune-checkpoint inhibitors (ICI)[J]. Cancers (Basel), 2020, 12(10): 2827. |
| [30] |
Facchinetti F, Mazzaschi G, Barbieri F, et al. First-line pembrolizumab in advanced non-small cell lung cancer patients with poor performance status[J]. Eur J Cancer, 2020, 130: 155-167.
doi: S0959-8049(20)30096-4 pmid: 32220780 |
| [31] |
Patil PD, Fernandez AP, Velcheti V, et al. Cases from the irAE tumor board: A multidisciplinary approach to a patient treated with immune checkpoint blockade who presented with a new rash[J]. Oncologist, 2019, 24(1): 4-8.
doi: 10.1634/theoncologist.2018-0434 pmid: 30355774 |
| [32] |
Drakaki A, Luhn P, Wakelee H,et al, Association of systemic corticosteroids with overall survival in patients receiving cancer immunotherapy for advanced melanoma, non-small cell lung cancer or urothelial cancer in routine clinical practice[J]. Ann Oncol, 2019, 30(11): 16-32.
doi: 10.1093/annonc/mdy472 URL |
| [33] |
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9): 603-605.
doi: 10.1007/s10654-010-9491-z pmid: 20652370 |
| [34] | Petrelli F, Signorelli D, Ghidini M, et al. Association of steroids use with survival in patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis[J]. Cancers (Basel), 2020, 12(3):546. |
| [35] |
Maddocks K, Jones JA. Jones, Bruton tyrosine kinase inhibition in chronic lymphocytic leukemia[J]. Semin Oncol, 2016, 43(2): 251-259.
doi: 10.1053/j.seminoncol.2016.02.008 pmid: 27040703 |
| [36] |
Lynch MP, DeDonato DM, Kutney-Lee A. Geriatric oncology program development and gero-oncology nursing[J]. Semin Oncol Nurs, 2016, 32(1): 44-54.
doi: 10.1016/j.soncn.2015.11.006 pmid: 26830267 |
| [37] |
Jove M, Vilariño N, Nadal E. Nadal, Impact of baseline steroids on efficacy of programmed cell death-1 (PD-1) and programmed death-ligand 1 (PD-L1) blockade in patients with advanced non-small cell lung cancer[J]. Transl Lung Cancer Res, 2019, 8(Suppl 4): S364-S368.
doi: 10.21037/tlcr.2019.06.06 URL |
| [38] |
Giles AJ, Hutchinson MND, Sonnemann HM, et al. Dexamethasone-induced immunosuppression: Mechanisms and implications for immunotherapy[J]. J Immunother Cancer, 2018, 6(1): 51.
doi: 10.1186/s40425-018-0371-5 pmid: 29891009 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||