Clinical Focus ›› 2022, Vol. 37 ›› Issue (7): 616-622.doi: 10.3969/j.issn.1004-583X.2022.07.006
Previous Articles Next Articles
Effect of pSOFA score combined with C-reactive protein and procalcitonin in prognosis assessment of sepsis children
Zhou Bin1, Zeng Cizheng2( ), Huang Yuge2, Zhong Mianling2, Wu Jiayuan2
), Huang Yuge2, Zhong Mianling2, Wu Jiayuan2
- 1. Pediatric Intensive Care Unit,Xiamen Children's Hospital (Xiamen Hospital of Children's Hospital Affiliated to Fudan University),Xiamen 361006,China
2. Children's Medical Center,Affiliated Hospital of Guangdong Medical University,Zhanjiang 524001,China
-
Received:2022-06-11Online:2022-07-20Published:2022-08-30 -
Contact:Zeng Cizheng E-mail:zengcizheng2010@163.com
CLC Number:
Cite this article
Zhou Bin, Zeng Cizheng, Huang Yuge, Zhong Mianling, Wu Jiayuan. Effect of pSOFA score combined with C-reactive protein and procalcitonin in prognosis assessment of sepsis children[J]. Clinical Focus, 2022, 37(7): 616-622.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2022.07.006
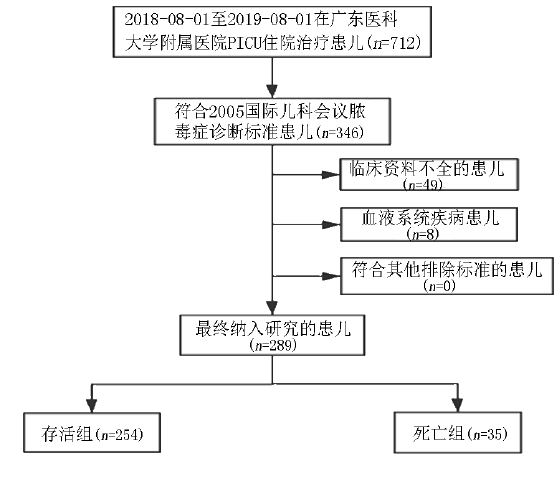
| 项目 | 存活组 | 死亡组 | χ2/ | |
|---|---|---|---|---|
| 例数 | 254 | 35 | ||
| 男/女 | 165/89 | 23/12 | 0.008 | 0.930 |
| 年龄[月, | 5.5[2.0,22.3] | 17.0[6.0,53.0] | 3.388 | 0.001 |
| PICU住院时间(d, | 6.6±7.2 | 8.4±13.4 | -1.142 | 0.215 |
| 总住院时间(d, | 12.8±9.7 | 9.0±16.3 | 1.352 | 0.185 |
| 机械通气时间(d, | 1.1±4.9 | 4.0±4.7 | -3.448 | 0.001 |
| 持续泵入血管活性药物[例(%)] | 57(22.4) | 32(91.4) | 68.695 | 0.000 |
| 胃肠功能(正常/肠麻痹/肠出血)[例(%)] | 250(98.4)/3(1.2)/1(0.4) | 27(77.1)/8(22.9)/0 | 23.463 | 0.000 |
| 格拉斯哥昏迷评分[分,M(P25,P75)] | 13[13,13] | 5[3,10] | -9.948 | 0.000 |
| CRP[mg/L, | 6.9[2.9,20.8] | 8.1[3.7,72.7] | 0.904 | 0.366 |
| PCT[ng/L, | 0.3[0.1,1.7] | 1.6[0.4,20.5] | 3.196 | 0.001 |
| pSOFA(分, | 3.0±2.4 | 10.6±3.9 | -11.137 | 0.000 |
| 项目 | 存活组 | 死亡组 | χ2/ | |
|---|---|---|---|---|
| 例数 | 254 | 35 | ||
| 男/女 | 165/89 | 23/12 | 0.008 | 0.930 |
| 年龄[月, | 5.5[2.0,22.3] | 17.0[6.0,53.0] | 3.388 | 0.001 |
| PICU住院时间(d, | 6.6±7.2 | 8.4±13.4 | -1.142 | 0.215 |
| 总住院时间(d, | 12.8±9.7 | 9.0±16.3 | 1.352 | 0.185 |
| 机械通气时间(d, | 1.1±4.9 | 4.0±4.7 | -3.448 | 0.001 |
| 持续泵入血管活性药物[例(%)] | 57(22.4) | 32(91.4) | 68.695 | 0.000 |
| 胃肠功能(正常/肠麻痹/肠出血)[例(%)] | 250(98.4)/3(1.2)/1(0.4) | 27(77.1)/8(22.9)/0 | 23.463 | 0.000 |
| 格拉斯哥昏迷评分[分,M(P25,P75)] | 13[13,13] | 5[3,10] | -9.948 | 0.000 |
| CRP[mg/L, | 6.9[2.9,20.8] | 8.1[3.7,72.7] | 0.904 | 0.366 |
| PCT[ng/L, | 0.3[0.1,1.7] | 1.6[0.4,20.5] | 3.196 | 0.001 |
| pSOFA(分, | 3.0±2.4 | 10.6±3.9 | -11.137 | 0.000 |
| 影响因素 | 回归系数 | 标准误 | Wald χ2值 | | 95% | |
|---|---|---|---|---|---|---|
| 年龄 | 0.015 | 0.009 | 2.938 | 1.015 | 0.998-1.033 | 0.087 |
| 机械通气时间 | -0.070 | 0.047 | 2.267 | 0.932 | 0.851-1.021 | 0.132 |
| 是否持续静脉泵入血管活性药物 | -1.756 | 0.804 | 4.772 | 0.173 | 0.036-0.835 | 0.029 |
| 格拉斯哥昏迷评分 | -0.186 | 0.097 | 3.718 | 0.830 | 0.687-1.003 | 0.054 |
| 胃肠功能 | 0.371 | 1.972 | 0.106 | 1.372 | 0.204-9.216 | 0.745 |
| CRP | 0.007 | 0.005 | 1.686 | 1.007 | 0.997-1.017 | 0.194 |
| PCT | -0.015 | 0.013 | 1.477 | 0.985 | 0.961-1.009 | 0.224 |
| pSOFA评分 | 0.371 | 0.105 | 12.394 | 1.449 | 1.179-1.782 | 0.000 |
| 影响因素 | 回归系数 | 标准误 | Wald χ2值 | | 95% | |
|---|---|---|---|---|---|---|
| 年龄 | 0.015 | 0.009 | 2.938 | 1.015 | 0.998-1.033 | 0.087 |
| 机械通气时间 | -0.070 | 0.047 | 2.267 | 0.932 | 0.851-1.021 | 0.132 |
| 是否持续静脉泵入血管活性药物 | -1.756 | 0.804 | 4.772 | 0.173 | 0.036-0.835 | 0.029 |
| 格拉斯哥昏迷评分 | -0.186 | 0.097 | 3.718 | 0.830 | 0.687-1.003 | 0.054 |
| 胃肠功能 | 0.371 | 1.972 | 0.106 | 1.372 | 0.204-9.216 | 0.745 |
| CRP | 0.007 | 0.005 | 1.686 | 1.007 | 0.997-1.017 | 0.194 |
| PCT | -0.015 | 0.013 | 1.477 | 0.985 | 0.961-1.009 | 0.224 |
| pSOFA评分 | 0.371 | 0.105 | 12.394 | 1.449 | 1.179-1.782 | 0.000 |
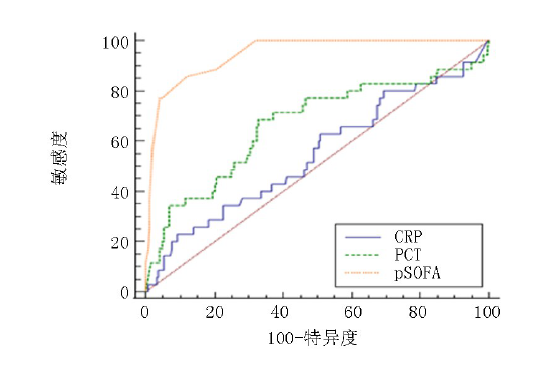
| 评分系统 | AUC | 95% | 最佳截 断值 | 敏感度 (%) | 特异度 (%) | 阳性预测 值(%) | 阴性预测 值(%) | | |
|---|---|---|---|---|---|---|---|---|---|
| CRP | 0.547 | 0.488-0.606 | >91.5 | 22.86 | 90.94 | 2.52 | 0.85 | 0.839 | 0.4016 |
| PCT | 0.667 | 0.609-0.721 | >0.891 | 68.57 | 67.32 | 2.10 | 0.47 | 2.953 | 0.0031 |
| pSOFA | 0.947 | 0.914-0.970 | >5 | 85.71 | 88.19 | 7.26 | 0.16 | 28.149 | <0.0001 |
| pSOFA+CRP | 0.947 | 0.914-0.970 | >0.071 | 85.71 | 88.19 | 7.26 | 0.16 | 28.149 | <0.0001 |
| pSOFA+PCT | 0.947 | 0.914-0.970 | >0.071 | 85.71 | 88.19 | 7.26 | 0.16 | 28.149 | <0.0001 |
| 评分系统 | AUC | 95% | 最佳截 断值 | 敏感度 (%) | 特异度 (%) | 阳性预测 值(%) | 阴性预测 值(%) | | |
|---|---|---|---|---|---|---|---|---|---|
| CRP | 0.547 | 0.488-0.606 | >91.5 | 22.86 | 90.94 | 2.52 | 0.85 | 0.839 | 0.4016 |
| PCT | 0.667 | 0.609-0.721 | >0.891 | 68.57 | 67.32 | 2.10 | 0.47 | 2.953 | 0.0031 |
| pSOFA | 0.947 | 0.914-0.970 | >5 | 85.71 | 88.19 | 7.26 | 0.16 | 28.149 | <0.0001 |
| pSOFA+CRP | 0.947 | 0.914-0.970 | >0.071 | 85.71 | 88.19 | 7.26 | 0.16 | 28.149 | <0.0001 |
| pSOFA+PCT | 0.947 | 0.914-0.970 | >0.071 | 85.71 | 88.19 | 7.26 | 0.16 | 28.149 | <0.0001 |
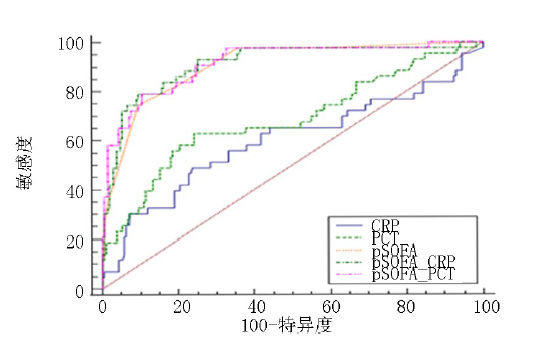
| 评分系统 | AUC | 95% | 最佳截 断值 | 敏感度 (%) | 特异度 (%) | 阳性预测 值(%) | 阴性预测 值(%) | | |
|---|---|---|---|---|---|---|---|---|---|
| CRP | 0.601 | 0.538-0.662 | >19.3 | 48.84 | 76.67 | 2.09 | 0.67 | 1.831 | 0.0671 |
| PCT | 0.684 | 0.623-0.741 | >1.01 | 62.79 | 76.19 | 2.64 | 0.49 | 3.660 | 0.0003 |
| pSOFA | 0.904 | 0.861-0.937 | >4 | 74.42 | 90.48 | 7.81 | 0.28 | 16.53 | <0.0001 |
| pSOFA+CRP | 0.911 | 0.869-0.943 | >0.2861 | 79.07 | 90.48 | 8.30 | 0.23 | 15.451 | <0.0001 |
| pSOFA+PCT | 0.913 | 0.872-0.945 | >0.2342 | 79.07 | 89.52 | 7.55 | 0.23 | 16.340 | <0.0001 |
| 评分系统 | AUC | 95% | 最佳截 断值 | 敏感度 (%) | 特异度 (%) | 阳性预测 值(%) | 阴性预测 值(%) | | |
|---|---|---|---|---|---|---|---|---|---|
| CRP | 0.601 | 0.538-0.662 | >19.3 | 48.84 | 76.67 | 2.09 | 0.67 | 1.831 | 0.0671 |
| PCT | 0.684 | 0.623-0.741 | >1.01 | 62.79 | 76.19 | 2.64 | 0.49 | 3.660 | 0.0003 |
| pSOFA | 0.904 | 0.861-0.937 | >4 | 74.42 | 90.48 | 7.81 | 0.28 | 16.53 | <0.0001 |
| pSOFA+CRP | 0.911 | 0.869-0.943 | >0.2861 | 79.07 | 90.48 | 8.30 | 0.23 | 15.451 | <0.0001 |
| pSOFA+PCT | 0.913 | 0.872-0.945 | >0.2342 | 79.07 | 89.52 | 7.55 | 0.23 | 16.340 | <0.0001 |
| [1] |
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Defintion for Sepsis and Sepsis Shock (Sepsis 3.0)[J]. JAMA, 2016, 315(8):801-810.
doi: 10.1001/jama.2016.0287 URL |
| [2] |
Fleishmann-Struzek C, Goldfarb DM, Schlattmann P, et al. The global burden of paediatric and neonatal sepsis: A systematic review[J]. Lancet Respir Med, 2018, 6(3):223-230.
doi: 10.1016/S2213-2600(18)30063-8 URL |
| [3] |
Schlapbach LJ, Straney L, Alexander J, et al. Mortality related to invasive infections, sepsis, and septic shock in critically ill children in Australia and New Zealand, 2002-13: A multicentre retrospective cohort study[J]. Lancet Infect Dis, 2015, 15(1):46-54.
doi: 10.1016/S1473-3099(14)71003-5 pmid: 25471555 |
| [4] |
Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation[J]. Crit Care Med, 2009, 37(5):1649-1654.
doi: 10.1097/CCM.0b013e31819def97 pmid: 19325482 |
| [5] | Zhong M, Huang Y, Li T, et al. Day-1 PELOD-2 and day-1 “quick” PELOD-2 scores in children with sepsis in the PICU[J]. [published online ahead of print, 2019 Sep 30]. J Pediatr (RioJ). 2020, 96(5):660-665. |
| [6] | Gül F, Arslantaᶊ MK, Cinel İ, et al. Changing definitions of sepsis[J]. Turk J Anaesthesiol Reanim, 2017, 45(3):129-138 |
| [7] |
ACabrita J, Pinheiro I, Menezes Falcão L. Rethinking the concept of sepsis and septic shock[J]. Eur J Intern Med, 2018, 54:1-5.
doi: S0953-6205(18)30234-6 pmid: 29921471 |
| [8] | 李熙鸿. 关于脓毒症3.0的争议[J]. 中国小儿急救医学, 2017, 24(7):481-485. |
| [9] |
Weiss SL, Fitzgerald JC, Pappachan J, et al. Global epidemiology of pediatric severe sepsis: The sepsis prevalence, outcomes, and therapies study[J]. Am J Respir Crit Care Med. 2016, 193(2):223-224.
doi: 10.1164/rccm.1932erratum URL |
| [10] |
Wu Q, Nie J, Wu FX, et al. Prognostic value of high-sensitivity C-reactive protein, procalcitonin and pancreatic stone protein in pediatric sepsis[J]. Med Sci Monit, 2017, 23:1533-1539.
doi: 10.12659/MSM.900856 URL |
| [11] | Morad EA, Rabie RA, Almalky MA, et al. Evaluation of procalcitonin, C-reactive protein, and interleukin-6 as early markers for diagnosis of neonatal sepsis[J]. Int J Microbiol, 2020:8889086. |
| [12] | Sakyi SA, Enimil A, Adu DK, et al. Individual and combined bioscore model of presepsin, procalcitonin, and high sensitive C-reactive protein as biomarkers for early diagnosis of paediatric sepsis[J]. Heliyon, 2020, 6(9):e04841. |
| [13] | 中华医学会儿科学分会医院感染管理与控制专业委员会. 血清降钙素原检测在儿童感染性疾病中的临床应用专家共识[J]. 中华儿科杂志, 2019, 57(1):9-15. |
| [14] |
Castelli GP, Pognani C, Cita M, et al. Procalcitonin, C-reactive protein, white blood cells and SOFA score in ICU: Diagnosis and monitoring of sepsis[J]. Minerva Anestesiol, 2006, 72(1-2):69-80.
pmid: 16407808 |
| [15] | Matics TJ, Sanchez-Pinto LN. Adaptation and Validation of a Pediatric Sequential Organ Failure Assessment Score and Evaluation of the Sepsis-3 Definitions in Critically Ill Children[J]. JAMA Pediatr, 2017, 171(10):e172352. |
| [16] |
Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics[J]. Pediatr Crit Care Med, 2005, 6(1):2-8.
doi: 10.1097/01.PCC.0000149131.72248.E6 URL |
| [17] | Van der Poll T, Van de Veerdonk FL, Scicluna BP, et al. The immunopathology of sepsis and potential therapeutic targets[J]. Nat Rev Immuno, 2017, 17(7):407-420. |
| [18] | Sheng Z, Yao Y. Sepsis and multiple organ dysfunction syndrome[J]. Chin J Emerg Med, 2003, 1(9):653-654. |
| [19] |
Rizzo AN, Dudek SM. Endothelial glycocalyx repair: Building a wall to protect the lung during sepsis[J]. Am J Respir Cell Mol Biol, 2017, 56(6):687-688.
doi: 10.1165/rcmb.2017-0065ED URL |
| [20] | Edmond K, Zaidi A. New approaches to preventing, diagnosing, and treating neonatalsepsis[J]. PLoS medicine, 2010, 7(3):e1000213. |
| [21] | 崔福鑫, 张瑜, 杜超, 等. 血清PCT与心脏标志物对脓毒症儿童病情程度的检测效果[J]. 临床儿科杂志, 2013, 31(17):174-176. |
| [22] |
Cour M, Bresson D, Hernu R, et al. SOFA score to assess the severity of the post-cardiac arrest syndrome[J]. Resuscitation, 2016, 102:110-115.
doi: 10.1016/j.resuscitation.2016.03.001 pmid: 26965206 |
| [23] |
An K, Wang Y, Li B, et al. Prognostic factors and outcome of patients undergoing hematopoietic stem cell transplantation who are admitted to pediatric intensive care unit[J]. BMC Pediatr, 2016, 16(1):138.
doi: 10.1186/s12887-016-0669-8 pmid: 27544347 |
| [24] | 卢秀兰, 仇君, 祝益民, 等. 小儿危重病例评分在重症手足口病病情及预后评估中的作用[J]. 中国当代儿科杂志, 2015, 17(9):961-964. |
| [25] | 张康羿, 胡勤锦. 降钙素原预测脓毒症儿童患者预后的临床价值[J]. 职业卫生与病伤, 2017, 32(6):369-371. |
| [26] | 王玉巧, 刘亮, 杨腊梅, 等. 降钙素原、急性生理和慢性健康状态评分对脓毒症预后评价[J]. 宁夏医科大学学报, 2018, 40(11):1309-1310. |
| [27] | 李晓梅, 杨国辉. 脓毒症早期诊断及预后评估相关指标研究进展[J]. 疑难病杂志, 2022, 21(7):768-771. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||