Clinical Focus ›› 2025, Vol. 40 ›› Issue (1): 21-28.doi: 10.3969/j.issn.1004-583X.2025.01.003
Previous Articles Next Articles
The potential of geriatric nutritional risk index in predicting the short-term outcome of intravenous thrombolysis in elderly individuals with acute cerebral infarction
Liu Jinhua1( ), Wang Chunmei1, Wang Ying2, Chen Kai1
), Wang Chunmei1, Wang Ying2, Chen Kai1
- 1. Department of Laboratory, Tianjin Beichen Hospital, Tianjin 300400,China
2. Department of Laboratory, Tianjin Beichen District Pudong Street Community Health Service Center, Tianjin 300400,China
-
Received:2024-09-28Online:2025-01-20Published:2025-01-17 -
Contact:Liu Jinhua,Email:1067479381@qq.com
CLC Number:
Cite this article
Liu Jinhua, Wang Chunmei, Wang Ying, Chen Kai. The potential of geriatric nutritional risk index in predicting the short-term outcome of intravenous thrombolysis in elderly individuals with acute cerebral infarction[J]. Clinical Focus, 2025, 40(1): 21-28.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2025.01.003
| 组别 | 例数 | 性别[例(%)] | 吸烟 [例(%)] | 饮酒 [例(%)] | 年龄 (年) | BMI (kg/m2) | 高血压 [例(%)] | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | ||||||||||||||
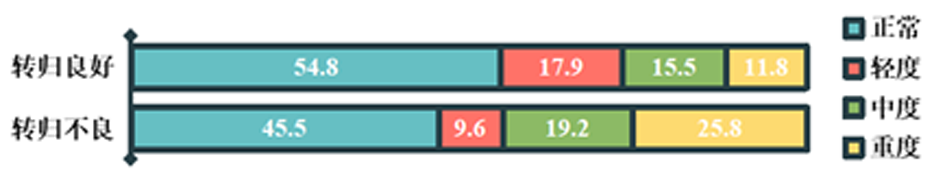
| 转归良好组 | 575 | 263(45.7) | 312(54.3) | 127(22.1) | 109(19.0) | 69.00±8.59 | 28.06±2.59 | 486(84.5) | |||||||
| 转归不良组 | 198 | 86(43.4) | 112(56.6) | 36(18.2) | 37(18.7) | 75.14±4.63 | 25.78±3.62 | 164(82.8) | |||||||
| 0.316 | 1.350 | 2.174 | 9.570 | 9.565 | 0.316 | ||||||||||
| 0.574 | 0.245 | 0.337 | <0.001 | <0.001 | 0.574 | ||||||||||
| 组别 | 糖尿病 [例(%)] | 脑卒中/TIA [例(%)] | 冠状动脉疾病 [例(%)] | 心房颤动 [例(%)] | SAO [例(%)] | LAA [例(%)] | CE [例(%)] | UND [例(%)] | |||||||
| 转归良好组 | 202(35.1) | 109(19.0) | 155(27.0) | 51(8.9) | 222(38.6) | 210(36.5) | 112(19.5) | 31(5.4) | |||||||
| 转归不良组 | 73(36.9) | 42(21.2) | 57(28.8) | 20(10.1) | 51(25.8) | 92(46.5) | 40(20.2) | 15(7.6) | |||||||
| χ2值 | 0.194 | 0.477 | 0.248 | 0.268 | 11.835 | ||||||||||
| 0.659 | 0.490 | 0.618 | 0.605 | 0.008 | |||||||||||
Tab.1 General information between the two groups
| 组别 | 例数 | 性别[例(%)] | 吸烟 [例(%)] | 饮酒 [例(%)] | 年龄 (年) | BMI (kg/m2) | 高血压 [例(%)] | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | ||||||||||||||
| 转归良好组 | 575 | 263(45.7) | 312(54.3) | 127(22.1) | 109(19.0) | 69.00±8.59 | 28.06±2.59 | 486(84.5) | |||||||
| 转归不良组 | 198 | 86(43.4) | 112(56.6) | 36(18.2) | 37(18.7) | 75.14±4.63 | 25.78±3.62 | 164(82.8) | |||||||
| 0.316 | 1.350 | 2.174 | 9.570 | 9.565 | 0.316 | ||||||||||
| 0.574 | 0.245 | 0.337 | <0.001 | <0.001 | 0.574 | ||||||||||
| 组别 | 糖尿病 [例(%)] | 脑卒中/TIA [例(%)] | 冠状动脉疾病 [例(%)] | 心房颤动 [例(%)] | SAO [例(%)] | LAA [例(%)] | CE [例(%)] | UND [例(%)] | |||||||
| 转归良好组 | 202(35.1) | 109(19.0) | 155(27.0) | 51(8.9) | 222(38.6) | 210(36.5) | 112(19.5) | 31(5.4) | |||||||
| 转归不良组 | 73(36.9) | 42(21.2) | 57(28.8) | 20(10.1) | 51(25.8) | 92(46.5) | 40(20.2) | 15(7.6) | |||||||
| χ2值 | 0.194 | 0.477 | 0.248 | 0.268 | 11.835 | ||||||||||
| 0.659 | 0.490 | 0.618 | 0.605 | 0.008 | |||||||||||
| 组别 | 例数 | NIHSS评分 (分) | 发病到溶栓 时间(h) | 出血转化 [例(%)] | 白细胞 (109/L) | 血红蛋白 (g/L) | 尿素氮 (mmol/L) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 转归良好组 | 575 | 4(2, 7) | 3.2(2.4, 3.8) | 12(2.1) | 7.7(5.8, 7.7) | 147.19±23.28 | 4.065(3.7, 5.53) | |||||
| 转归不良组 | 198 | 9(6, 12) | 3.7(2.5, 3.9) | 34(17.2) | 7.7(6.2, 7.7) | 142.69±26.19 | 4.59(3.7, 6.015) | |||||
| χ2/ | 9.952 | 3.516 | 59.882 | 0.734 | 2.272 | 2.426 | ||||||
| <0.001 | <0.001 | <0.001 | 0.463 | 0.023 | 0.015 | |||||||
| 组别 | 淋巴细胞 (109/L) | LDL-C (mmol/L) | 白蛋白 (g/L) | 肌酐 (μmol/L) | 空腹血糖 (mmol/L) | GNRI (分) | ||||||
| 转归良好组 | 2.148(1.898, 2.253) | 2.98(2.33, 3.70) | 39.4(36.3, 42.7) | 51(51, 64) | 5.2(4.8, 5.4) | 90.722(82.239, 100.055) | ||||||
| 转归不良组 | 2.148(2.067, 2.204) | 3.05(2.3, 3.81) | 39.9(35.7, 43) | 51(51, 62) | 5.2(5.2, 5.3) | 90.106(84.622, 98.141) | ||||||
| 1.247 | 0.648 | 0.708 | 1.272 | 1.384 | 6.108 | |||||||
| 0.212 | 0.517 | 0.479 | 0.203 | 0.166 | <0.001 | |||||||
Tab.2 Clinical indicators between the two groups
| 组别 | 例数 | NIHSS评分 (分) | 发病到溶栓 时间(h) | 出血转化 [例(%)] | 白细胞 (109/L) | 血红蛋白 (g/L) | 尿素氮 (mmol/L) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 转归良好组 | 575 | 4(2, 7) | 3.2(2.4, 3.8) | 12(2.1) | 7.7(5.8, 7.7) | 147.19±23.28 | 4.065(3.7, 5.53) | |||||
| 转归不良组 | 198 | 9(6, 12) | 3.7(2.5, 3.9) | 34(17.2) | 7.7(6.2, 7.7) | 142.69±26.19 | 4.59(3.7, 6.015) | |||||
| χ2/ | 9.952 | 3.516 | 59.882 | 0.734 | 2.272 | 2.426 | ||||||
| <0.001 | <0.001 | <0.001 | 0.463 | 0.023 | 0.015 | |||||||
| 组别 | 淋巴细胞 (109/L) | LDL-C (mmol/L) | 白蛋白 (g/L) | 肌酐 (μmol/L) | 空腹血糖 (mmol/L) | GNRI (分) | ||||||
| 转归良好组 | 2.148(1.898, 2.253) | 2.98(2.33, 3.70) | 39.4(36.3, 42.7) | 51(51, 64) | 5.2(4.8, 5.4) | 90.722(82.239, 100.055) | ||||||
| 转归不良组 | 2.148(2.067, 2.204) | 3.05(2.3, 3.81) | 39.9(35.7, 43) | 51(51, 62) | 5.2(5.2, 5.3) | 90.106(84.622, 98.141) | ||||||
| 1.247 | 0.648 | 0.708 | 1.272 | 1.384 | 6.108 | |||||||
| 0.212 | 0.517 | 0.479 | 0.203 | 0.166 | <0.001 | |||||||
| 项目 | 回归系数 | 标准误 | Wald χ2值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 年龄 | 0.195 | 0.018 | 85.709 | <0.001 | 1.215 | 1.166 | 1.266 |
| 入院NIHSS评分 | 0.137 | 0.023 | 33.464 | <0.001 | 1.417 | 1.095 | 1.202 |
| TOAST病因分型 | |||||||
| SAO | - | 4.611 | 0.025 | - | - | ||
| LAA | 0.595 | 0.650 | 1.066 | 0.302 | 1.814 | 0.586 | 5.614 |
| CE | 1.214 | 0.639 | 4.696 | 0.030 | 3.367 | 1.123 | 10.096 |
| UND | 0.636 | 0.669 | 1.144 | 0.285 | 1.889 | 0.589 | 6.057 |
| 出血转化 | 0.216 | 0.057 | 34.831 | <0.001 | 1.241 | 1.155 | 1.333 |
| BMI | -2.328 | 0.048 | 18.922 | <0.001 | 0.097 | 0.034 | 0.278 |
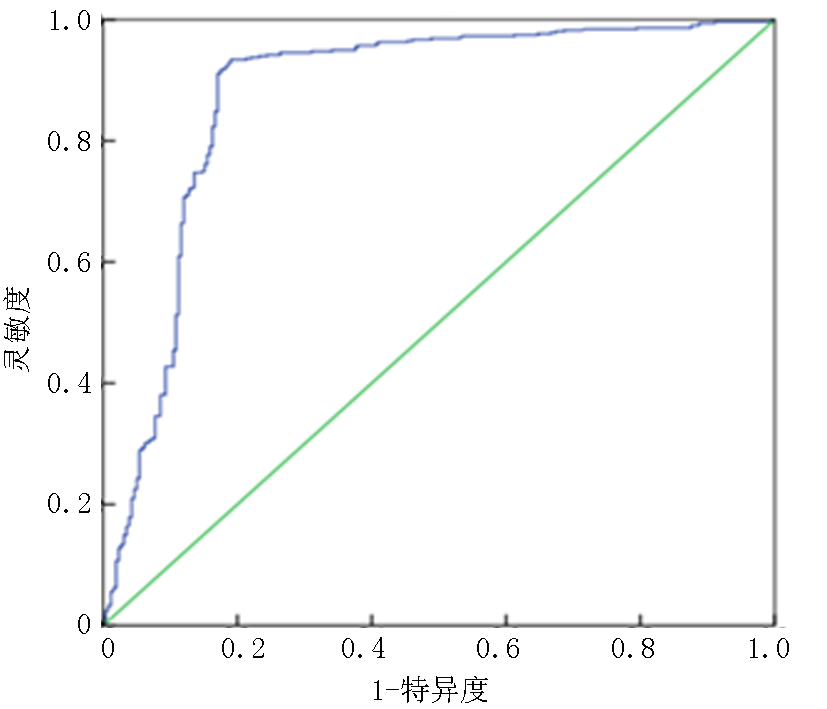
| 低GNRI | 0.739 | 0.243 | 10.181 | 0.001 | 2.093 | 1.330 | 3.295 |
Tab.3 Multivariate logistic regression analysis of risk factors for short-term outcomes of intravenous thrombolysis in AIS patients
| 项目 | 回归系数 | 标准误 | Wald χ2值 | 95% | |||
|---|---|---|---|---|---|---|---|
| 下限 | 上限 | ||||||
| 年龄 | 0.195 | 0.018 | 85.709 | <0.001 | 1.215 | 1.166 | 1.266 |
| 入院NIHSS评分 | 0.137 | 0.023 | 33.464 | <0.001 | 1.417 | 1.095 | 1.202 |
| TOAST病因分型 | |||||||
| SAO | - | 4.611 | 0.025 | - | - | ||
| LAA | 0.595 | 0.650 | 1.066 | 0.302 | 1.814 | 0.586 | 5.614 |
| CE | 1.214 | 0.639 | 4.696 | 0.030 | 3.367 | 1.123 | 10.096 |
| UND | 0.636 | 0.669 | 1.144 | 0.285 | 1.889 | 0.589 | 6.057 |
| 出血转化 | 0.216 | 0.057 | 34.831 | <0.001 | 1.241 | 1.155 | 1.333 |
| BMI | -2.328 | 0.048 | 18.922 | <0.001 | 0.097 | 0.034 | 0.278 |
| 低GNRI | 0.739 | 0.243 | 10.181 | 0.001 | 2.093 | 1.330 | 3.295 |
| [1] |
GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: A systematic analysis for the global burden of disease study 2016[J]. Lancet Neurol, 2019, 18(5): 459-480.
doi: S1474-4422(18)30499-X pmid: 30879893 |
| [2] | Wang YJ, Li ZX, Gu HQ, et al. China stroke statistics: An update on the 2019 report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations[J]. Stroke Vasc Neurol, 2022, 7(5): 415-450. |
| [3] | Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: Results from a nationwide population-based survey of 480 687 adults[J]. Circulation, 2017, 135(8): 759-771. |
| [4] |
Dávalos A, Ricart W, Gonzalez-Huix F, et al. Effect of malnutrition after acute stroke on clinical outcome[J]. Stroke, 1996, 27(6): 1028-1032.
pmid: 8650709 |
| [5] |
Martineau J, Bauer JD, Isenring E, et al. Malnutrition determined by the patient-generated subjective global assessment is associated with poor outcomes in acute stroke patients[J]. Clin Nutr, 2005, 24(6): 1073-1077.
pmid: 16213064 |
| [6] |
Poor nutritional status on admission predicts poor outcomes after stroke: Observational data from the FOOD trial[J]. Stroke, 2003, 34(6): 1450-1456.
doi: 10.1161/01.STR.0000074037.49197.8C pmid: 12750536 |
| [7] |
Schuetz P, Fehr R, Baechli V, et al. Individualised nutritional support in medical inpatients at nutritional risk: A randomised clinical trial[J]. Lancet, 2019, 393(10188): 2312-2321.
doi: S0140-6736(18)32776-4 pmid: 31030981 |
| [8] |
Cederholm T, Bosaeus I, Barazzoni R, et al. Diagnostic criteria for malnutrition - an ESPEN consensus statement[J]. Clin Nutr, 2015, 34(3): 335-340.
doi: 10.1016/j.clnu.2015.03.001 pmid: 25799486 |
| [9] |
Jensen GL, Cederholm T, Correia M, et al. GLIM criteria for the diagnosis of malnutrition: A consensus report from the Global Clinical Nutrition Community[J]. JPEN J Parenter Enteral Nutr, 2019, 43(1): 32-40.
doi: 10.1002/jpen.1440 pmid: 30175461 |
| [10] |
Bouillanne O, Morineau G, Dupont C, et al. Geriatric nutritional risk index: A new index for evaluating at-risk elderly medical patients[J]. Am J Clin Nutr, 2005, 82(4): 777-783.
doi: 10.1093/ajcn/82.4.777 pmid: 16210706 |
| [11] | 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志, 2018, 51(9): 666-682. |
| [12] | 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性脑梗死后出血转化诊治共识2019[J]. 中华神经科杂志, 2019, 52(4): 252-265. |
| [13] |
Bamford JM, Sandercock PA, Warlow CP, et al. Interobserver agreement for the assessment of handicap in stroke patients[J]. Stroke, 1989, 20(6): 828.
doi: 10.1161/01.str.20.6.828 pmid: 2728057 |
| [14] |
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment[J]. Stroke, 1993, 24(1): 35-41.
doi: 10.1161/01.str.24.1.35 pmid: 7678184 |
| [15] |
Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association task force on practice guidelines and the obesity society[J]. J Am Coll Cardiol, 2014, 63(25 Pt B): 2985-3023.
doi: 10.1016/j.jacc.2013.11.004 pmid: 24239920 |
| [16] | Zhang G, Pan Y, Zhang R, et al. Prevalence and prognostic significance of malnutrition risk in patients with acute ischemic stroke: Results from the Third China National Stroke Registry[J]. Stroke, 2022, 53(1): 111-119. |
| [17] |
Zhang M, Ye S, Huang X, et al. Comparing the prognostic significance of nutritional screening tools and ESPEN-DCM on 3-month and 12-month outcomes in stroke patients[J]. Clin Nutr, 2021, 40(5): 3346-3353.
doi: 10.1016/j.clnu.2020.11.001 pmid: 33221053 |
| [18] |
Nishioka S, Omagari K, Nishioka E, et al. Concurrent and predictive validity of the mini nutritional assessment short-form and the geriatric nutritional risk index in older stroke rehabilitation patients[J]. J Hum Nutr Diet, 2020, 33(1): 12-22.
doi: 10.1111/jhn.12699 pmid: 31435986 |
| [19] |
Chen N, Li Y, Fang J, et al. Risk factors for malnutrition in stroke patients: A meta-analysis[J]. Clin Nutr, 2019, 38(1): 127-135.
doi: S0261-5614(17)31434-6 pmid: 29310894 |
| [20] | Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 Update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association[J]. Stroke, 2019, 50(12): e344-e418. |
| [21] |
Burgos R, Bretón I, Cereda E, et al. ESPEN guideline clinical nutrition in neurology[J]. Clin Nutr, 2018, 37(1): 354-396.
doi: S0261-5614(17)30318-7 pmid: 29274834 |
| [22] | Dennis M, Lewis S, Cranswick G, et al. FOOD: A multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke[J]. Health Technol Assess, 2006, 10(2): iii-iv, ix-x, 1-120. |
| [23] | Gao J, Zhao Y, Du M, et al. Serum albumin levels and clinical outcomes among ischemic stroke patients treated with endovascular thrombectomy[J]. Neuropsychiatr Dis Treat, 2021, 17: 401-411. |
| [24] |
Löwhagen Hendén P, Rentzos A, Karlsson JE, et al. Hypotension during endovascular treatment of ischemic stroke is a risk factor for poor neurological outcome[J]. Stroke, 2015, 46(9): 2678-2680.
doi: 10.1161/STROKEAHA.115.009808 pmid: 26173727 |
| [25] | Park HP, Nimmagadda A, DeFazio RA, et al. Albumin therapy augments the effect of thrombolysis on local vascular dynamics in a rat model of arteriolar thrombosis: A two-photon laser-scanning microscopy study[J]. Stroke, 2008, 39(5): 1556-1562. |
| [26] |
Reinhart WH, Nagy C. Albumin affects erythrocyte aggregation and sedimentation[J]. Eur J Clin Invest, 1995, 25(7): 523-528.
pmid: 7556371 |
| [27] | Jickling GC, Liu D, Stamova B, et al. Hemorrhagic transformation after ischemic stroke in animals and humans[J]. J Cereb Blood Flow Metab, 2014, 34(2): 185-199. |
| [28] | Zoellner H, Höfler M, Beckmann R, et al. Serum albumin is a specific inhibitor of apoptosis in human endothelial cells[J]. J Cell Sci, 1996, 109(Pt 10): 2571-2580. |
| [29] |
Spinella R, Sawhney R, Jalan R. Albumin in chronic liver disease: Structure, functions and therapeutic implications[J]. Hepatol Int, 2016, 10(1): 124-132.
doi: 10.1007/s12072-015-9665-6 pmid: 26420218 |
| [30] |
Che R, Huang X, Zhao W, et al. Low serum albumin level as a predictor of hemorrhage transformation after intravenous thrombolysis in ischemic stroke patients[J]. Sci Rep, 2017, 7(1): 7776.
doi: 10.1038/s41598-017-06802-y pmid: 28798356 |
| [31] | Naito H, Hosomi N, Nezu T, et al. Prognostic role of the controlling nutritional status score in acute ischemic stroke among stroke subtypes[J]. J Neurol Sci, 2020, 416: 116984. |
| [32] |
Gensicke H, Zinkstok SM, Roos YB, et al. IV thrombolysis and renal function[J]. Neurology, 2013, 81(20): 1780-1788.
doi: 10.1212/01.wnl.0000435550.83200.9e pmid: 24122182 |
| [33] | Lussier G, Evans AJ, Houston I, et al. Compact arterial monitoring device use in resuscitative endovascular balloon occlusion of the aorta (REBOA): A simple validation study in swine[J]. Cureus, 2024, 16(10): e70789. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||