Clinical Focus ›› 2024, Vol. 39 ›› Issue (4): 314-319.doi: 10.3969/j.issn.1004-583X.2024.04.003
Previous Articles Next Articles
Correlation between the lung ultrasound phenotype of gravity-dependent deaeration and poor prognosis in sepsis patients requiring mechanical ventilation
Wang Qian1, Yin Wanhong1( ), Zou Tongjuan1, Tie Xin1, Zhu Junchen2, Chen Lyulin2, Zeng Xueying1
), Zou Tongjuan1, Tie Xin1, Zhu Junchen2, Chen Lyulin2, Zeng Xueying1
- 1. Department of Critical Care Medicine, West China Hospital, Sichuan University, Chengdu 610041, China
2. Department of Critical Care Medicine, Affiliated Hospital of Chengdu University, Chengdu 610081, China
-
Received:2024-03-12Online:2024-04-20Published:2024-06-27 -
Contact:Yin Wanhong, Email:yinwanhong@wchscu.cn
CLC Number:
Cite this article
Wang Qian, Yin Wanhong, Zou Tongjuan, Tie Xin, Zhu Junchen, Chen Lyulin, Zeng Xueying. Correlation between the lung ultrasound phenotype of gravity-dependent deaeration and poor prognosis in sepsis patients requiring mechanical ventilation[J]. Clinical Focus, 2024, 39(4): 314-319.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.04.003
| 定义 | 肺部超声病理生理模式定义 | MLUS (分) |
|---|---|---|
| A | 检查区域胸膜正常+A线 | 0 |
| A1 | 检查区域胸膜滑动征消失+A线,可见“肺点” | NM |
| B1 | 检查区域3根以上少量B线 | 1 |
| B2 | 检查区域多根融合的B线 | 1 |
| C1 | 检查区域胸膜下肺小叶完全失充气,直径0.5 cm~1 cm,即“碎片征” | 3 |
| C2 | 检查区域实质回声混杂不均,大片实变,动态支气管征,胸水较少(液性暗区小于3 cm) | 3 |
| C3 | 检查区域实质回声相对均一,肺组织容积减少,大量胸水压迫,不张肺组织呈“水母征”,外缘胸膜光滑,支气管气相征早期明显,且动态支气管气征较多 | 3 |
| C4 | 检查区域实质回声相对均一,类似肝脏回声(肝样变),肺组织容积明显减少,胸水量少,早期呈静态支气管征,后期减少或无支气管征 | 3 |
Tab.1 Lung ultrasound pathophysiological patterns in each region
| 定义 | 肺部超声病理生理模式定义 | MLUS (分) |
|---|---|---|
| A | 检查区域胸膜正常+A线 | 0 |
| A1 | 检查区域胸膜滑动征消失+A线,可见“肺点” | NM |
| B1 | 检查区域3根以上少量B线 | 1 |
| B2 | 检查区域多根融合的B线 | 1 |
| C1 | 检查区域胸膜下肺小叶完全失充气,直径0.5 cm~1 cm,即“碎片征” | 3 |
| C2 | 检查区域实质回声混杂不均,大片实变,动态支气管征,胸水较少(液性暗区小于3 cm) | 3 |
| C3 | 检查区域实质回声相对均一,肺组织容积减少,大量胸水压迫,不张肺组织呈“水母征”,外缘胸膜光滑,支气管气相征早期明显,且动态支气管气征较多 | 3 |
| C4 | 检查区域实质回声相对均一,类似肝脏回声(肝样变),肺组织容积明显减少,胸水量少,早期呈静态支气管征,后期减少或无支气管征 | 3 |
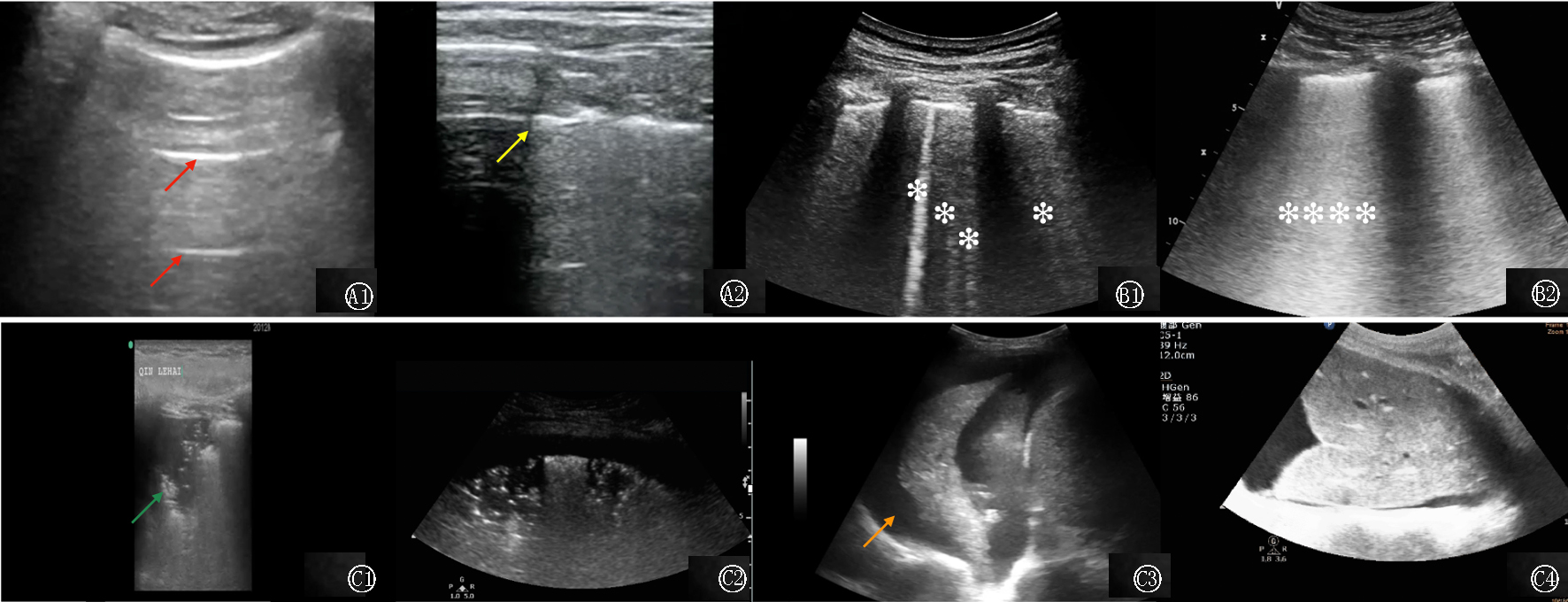
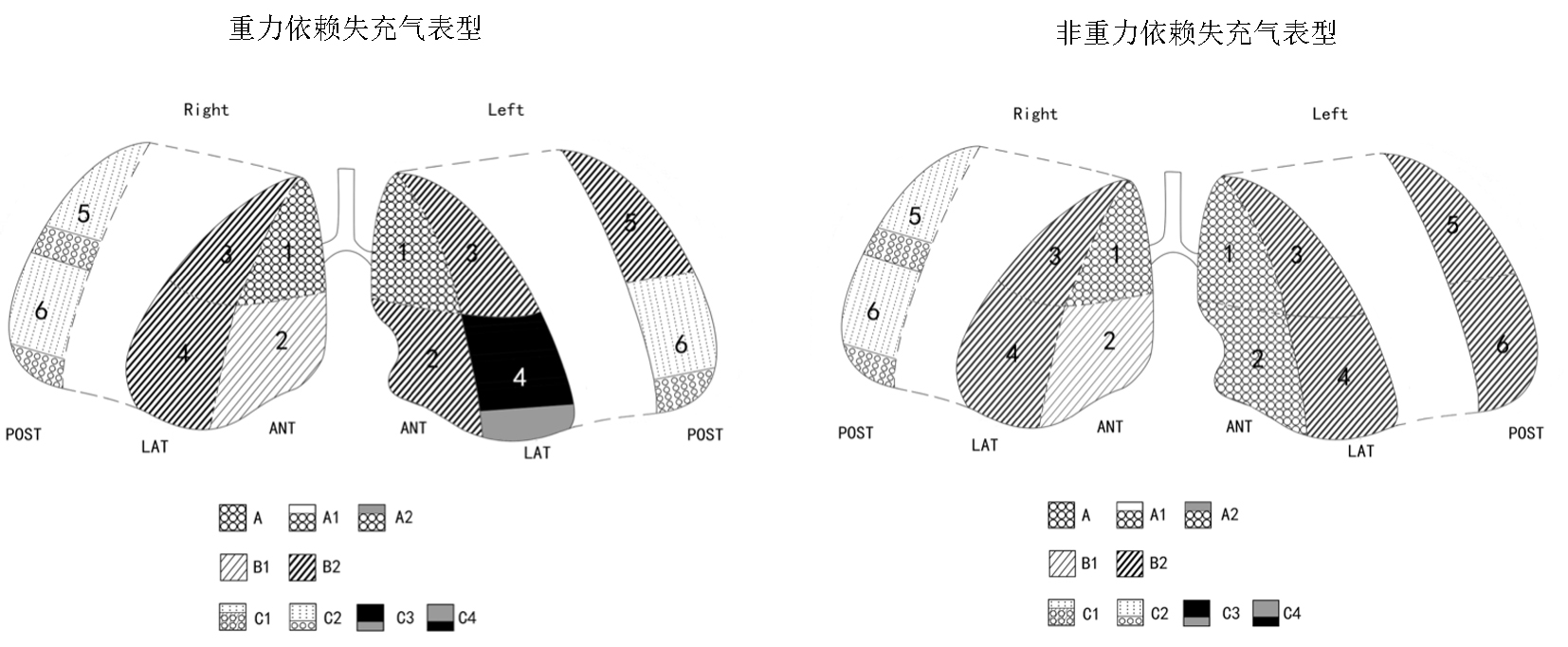
Fig.1 Different lung ultrasound patterns The red arrows presented A-lines(hyperechoic horizontal line); The yellow arrow presented “lung point” indicating pneumothorax; The green arrow presented “fragment sign”; The orange arrow presented “jellyfish sign” indicating pleural effusion; Presented B1-lines (isolated hyperechoic vertical line, marked by snowflake), Presented B2-lines(coalescent hyperechoic vertical line, marked by snowflakes)
| 指标 | 总体( | 生存组( | 死亡组( | 统计值 | |
|---|---|---|---|---|---|
| 年龄(岁) | 57.5±15.2 | 56.02±14.43 | 62.08±16.75 | 0.032 | |
| 性别[例(%)] | |||||
| 男性 女性 | 103(66.5) 52(33.5) | 79(67.52) 38(32.48) | 24(63.16) 14(36.84) | χ2=0.245 | 0.621 |
| 体温(℃) | 37.6±0.9 | 37.6±0.95 | 37.48±0.82 | 0.465 | |
| 心率(次/min) | 115.00±24.00 | 112.8±24.43 | 119.6±21.85 | 0.130 | |
| MAAP(mmHg) | 70.3±12.0 | 70.81±11.66 | 68.61±11.35 | 0.309 | |
| 血氧饱和度(%) | 96.7±3.5 | 96.82±3.58 | 96.42±3.26 | 0.542 | |
| 呼吸频率 (次/min) | 24.4±4.6 | 24.1±4.33 | 25.42±5.22 | 0.124 | |
| 乳酸(mmol/L) | 2.0(1.5, 2.6) | 1.9(1.4, 2.3) | 2.5(1.8, 3) | 0.006 | |
| 氧合指数 | 221.25(149.8, 288.29) | 224(153.75, 279.75) | 204.665(121, 309) | 0.294 | |
| 白细胞计数(×109/L) | 11.17(7.42, 14.34) | 10.57(7.42, 13.64) | 11.935(8.32, 17.09) | 0.054 | |
| C-反应蛋白(mg/L) | 79.0(16.2, 137) | 72(10.2, 137) | 94.9(39, 140) | 0.079 | |
| 白细胞介素6(ng/L) | 64.0(18.77, 164.0) | 61.08(39.34, 109.4) | 93(48, 306.3) | 0.022 | |
| 降钙素原(μg/L) | 1.16(0.26, 8.4) | 0.81(0.17, 3.9) | 6.59(0.78, 12.1) | 0.008 | |
| APACHE Ⅱ评分(分) | 25.1±6.5 | 23.69±6.04 | 29.26±6.34 | <0.01 | |
| SOFA评分(分) | 10.1±4.0 | 9.48±3.9 | 11.82±3.94 | 0.002 | |
| 合并高血压[例(%)] | |||||
| 是 否 | 58(37.4) 97(62.6) | 43(36.7) 74(63.2) | 15(39.5) 23(60.5) | χ2=0.091 | 0.763 |
| 合并糖尿病[例(%)] | |||||
| 是 否 | 30(19.4) 125(80.6) | 19(16.2) 98(83.8) | 11(28.9) 27(71.1) | χ2=2.968 | 0.085 |
| 主要感染部位[例(%)] | |||||
| 肺部 | 93(60.0) | 76(64.9) | 17(44.7) | ||
| 腹部 | 50(32.3) | 31(26.5) | 19(50.0) | ||
| 颈部脓肿 | 4(2.6) | 4(3.4) | 0 | - | 0.079 |
| 泌尿系 | 4(2.6) | 3(2.6) | 1(2.6) | ||
| 肛周脓肿 | 2(1.3) | 1(0.9) | 1(2.6) | ||
| 血源性 | 2(1.3) | 2(1.7) | 0 | ||
| NE[μg/(kg·min)] | 0.19(0.10, 0.46) | 0.05(0, 0.15714) | 0.344155(0.18182, 0.8) | <0.01 | |
| MLUS(分) | 16.88±8.38 | 16.06±7.81 | 19.39±9.64 | 0.032 | |
| 间质性失充气模式[例(%)] | |||||
| 否 是 | 98(63.2) 57(36.8) | 79(67.5) 38(32.5) | 19(50.0) 19(50.0) | χ2=3.7874 | 0.052 |
| 不张性失充气模式[例(%)] | |||||
| 否 是 | 111(71.6) 44(28.4) | 83(70.9) 34(29.1) | 28(73.7) 10(26.3) | χ2=0.1062 | 0.742 |
| 实变性失充气模式[例(%)] | |||||
| 否 是 | 57(36.8) 98(63.2) | 46(39.3) 71(60.7) | 11(28.9) 27(71.1) | χ2=1.326 | 0.250 |
| 住院时间(d) | 23(14, 38) | 26(16, 44) | 14.5(8, 29) | 0.001 | |
| ICU住院时间(d) | 16(8, 29) | 17(9, 33) | 13(7, 24) | 0.050 | |
| 机械通气时间(h) | 241(114, 472.29) | 227(97, 443.65) | 305(183.53, 572.07) | 0.026 |
Tab.2 Comparison of clinical data between the two groups
| 指标 | 总体( | 生存组( | 死亡组( | 统计值 | |
|---|---|---|---|---|---|
| 年龄(岁) | 57.5±15.2 | 56.02±14.43 | 62.08±16.75 | 0.032 | |
| 性别[例(%)] | |||||
| 男性 女性 | 103(66.5) 52(33.5) | 79(67.52) 38(32.48) | 24(63.16) 14(36.84) | χ2=0.245 | 0.621 |
| 体温(℃) | 37.6±0.9 | 37.6±0.95 | 37.48±0.82 | 0.465 | |
| 心率(次/min) | 115.00±24.00 | 112.8±24.43 | 119.6±21.85 | 0.130 | |
| MAAP(mmHg) | 70.3±12.0 | 70.81±11.66 | 68.61±11.35 | 0.309 | |
| 血氧饱和度(%) | 96.7±3.5 | 96.82±3.58 | 96.42±3.26 | 0.542 | |
| 呼吸频率 (次/min) | 24.4±4.6 | 24.1±4.33 | 25.42±5.22 | 0.124 | |
| 乳酸(mmol/L) | 2.0(1.5, 2.6) | 1.9(1.4, 2.3) | 2.5(1.8, 3) | 0.006 | |
| 氧合指数 | 221.25(149.8, 288.29) | 224(153.75, 279.75) | 204.665(121, 309) | 0.294 | |
| 白细胞计数(×109/L) | 11.17(7.42, 14.34) | 10.57(7.42, 13.64) | 11.935(8.32, 17.09) | 0.054 | |
| C-反应蛋白(mg/L) | 79.0(16.2, 137) | 72(10.2, 137) | 94.9(39, 140) | 0.079 | |
| 白细胞介素6(ng/L) | 64.0(18.77, 164.0) | 61.08(39.34, 109.4) | 93(48, 306.3) | 0.022 | |
| 降钙素原(μg/L) | 1.16(0.26, 8.4) | 0.81(0.17, 3.9) | 6.59(0.78, 12.1) | 0.008 | |
| APACHE Ⅱ评分(分) | 25.1±6.5 | 23.69±6.04 | 29.26±6.34 | <0.01 | |
| SOFA评分(分) | 10.1±4.0 | 9.48±3.9 | 11.82±3.94 | 0.002 | |
| 合并高血压[例(%)] | |||||
| 是 否 | 58(37.4) 97(62.6) | 43(36.7) 74(63.2) | 15(39.5) 23(60.5) | χ2=0.091 | 0.763 |
| 合并糖尿病[例(%)] | |||||
| 是 否 | 30(19.4) 125(80.6) | 19(16.2) 98(83.8) | 11(28.9) 27(71.1) | χ2=2.968 | 0.085 |
| 主要感染部位[例(%)] | |||||
| 肺部 | 93(60.0) | 76(64.9) | 17(44.7) | ||
| 腹部 | 50(32.3) | 31(26.5) | 19(50.0) | ||
| 颈部脓肿 | 4(2.6) | 4(3.4) | 0 | - | 0.079 |
| 泌尿系 | 4(2.6) | 3(2.6) | 1(2.6) | ||
| 肛周脓肿 | 2(1.3) | 1(0.9) | 1(2.6) | ||
| 血源性 | 2(1.3) | 2(1.7) | 0 | ||
| NE[μg/(kg·min)] | 0.19(0.10, 0.46) | 0.05(0, 0.15714) | 0.344155(0.18182, 0.8) | <0.01 | |
| MLUS(分) | 16.88±8.38 | 16.06±7.81 | 19.39±9.64 | 0.032 | |
| 间质性失充气模式[例(%)] | |||||
| 否 是 | 98(63.2) 57(36.8) | 79(67.5) 38(32.5) | 19(50.0) 19(50.0) | χ2=3.7874 | 0.052 |
| 不张性失充气模式[例(%)] | |||||
| 否 是 | 111(71.6) 44(28.4) | 83(70.9) 34(29.1) | 28(73.7) 10(26.3) | χ2=0.1062 | 0.742 |
| 实变性失充气模式[例(%)] | |||||
| 否 是 | 57(36.8) 98(63.2) | 46(39.3) 71(60.7) | 11(28.9) 27(71.1) | χ2=1.326 | 0.250 |
| 住院时间(d) | 23(14, 38) | 26(16, 44) | 14.5(8, 29) | 0.001 | |
| ICU住院时间(d) | 16(8, 29) | 17(9, 33) | 13(7, 24) | 0.050 | |
| 机械通气时间(h) | 241(114, 472.29) | 227(97, 443.65) | 305(183.53, 572.07) | 0.026 |
| 因素 | 95% | |||
|---|---|---|---|---|
| 年龄 | 1.021 | 0.996, 1.047 | 0.094 | |
| 乳酸 | 0.934 | 0.444, 1.963 | 0.857 | |
| 氧合指数 | 0.801 | 0.531, 1.206 | 0.288 | |
| 白细胞介素6 | 1.374 | 1.17, 1.614 | 0.000 | |
| APACHE Ⅱ评分 | 1.000 | 0.996, 1.004 | 0.960 | |
| SOFA评分 | 1.055 | 1.018, 1.093 | 0.003 | |
| 是否应用血管活性药物 | 是 vs 否 | 1.002 | 0.998, 1.006 | 0.309 |
| MLUS | 1.000 | 0.999, 1.001 | 0.767 | |
| 间质性失充气模式 | 是 vs 否 | 1.019 | 1.001, 1.038 | 0.042 |
| 不张性失充气模式 | 是 vs 否 | 1.111 | 1.057, 1.167 | <0.01 |
| 实变性失充气模式 | 是 vs 否 | 1.148 | 1.06, 1.243 | 0.001 |
| 机械通气时间 | 3.324 | 1.271, 8.694 | 0.014 | |
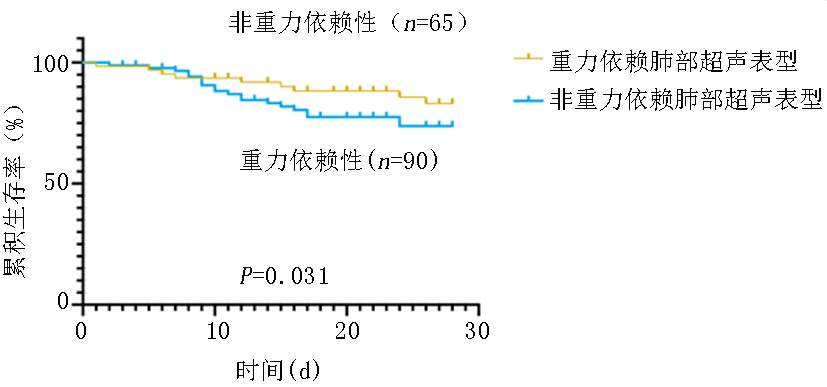
| 重力依赖失充气 | 是 vs 否 | 2.665 | 1.26, 4.768 | 0.008 |
Tab.3 Univariate COX proportional risk analysis of 28-day prognosis in sepsis patients requiring mechanical ventilation
| 因素 | 95% | |||
|---|---|---|---|---|
| 年龄 | 1.021 | 0.996, 1.047 | 0.094 | |
| 乳酸 | 0.934 | 0.444, 1.963 | 0.857 | |
| 氧合指数 | 0.801 | 0.531, 1.206 | 0.288 | |
| 白细胞介素6 | 1.374 | 1.17, 1.614 | 0.000 | |
| APACHE Ⅱ评分 | 1.000 | 0.996, 1.004 | 0.960 | |
| SOFA评分 | 1.055 | 1.018, 1.093 | 0.003 | |
| 是否应用血管活性药物 | 是 vs 否 | 1.002 | 0.998, 1.006 | 0.309 |
| MLUS | 1.000 | 0.999, 1.001 | 0.767 | |
| 间质性失充气模式 | 是 vs 否 | 1.019 | 1.001, 1.038 | 0.042 |
| 不张性失充气模式 | 是 vs 否 | 1.111 | 1.057, 1.167 | <0.01 |
| 实变性失充气模式 | 是 vs 否 | 1.148 | 1.06, 1.243 | 0.001 |
| 机械通气时间 | 3.324 | 1.271, 8.694 | 0.014 | |
| 重力依赖失充气 | 是 vs 否 | 2.665 | 1.26, 4.768 | 0.008 |
| 因素 | 95% | |||
|---|---|---|---|---|
| 年龄 | 0.968 | 0.933, 1.005 | 0.086 | |
| 乳酸 | 0.841 | 0.345, 2.05 | 0.703 | |
| 氧合指数 | 0.496 | 0.267, 0.924 | 0.027 | |
| 白细胞介素6 | 1.500 | 1.117, 2.016 | 0.007 | |
| APACHE Ⅱ评分 | 1.007 | 1.001, 1.014 | 0.035 | |
| SOFA评分 | 1.027 | 0.974, 1.083 | 0.320 | |
| 间质性失充气模式 | 是 vs 否 | 0.998 | 0.964, 1.033 | 0.910 |
| 不张性失充气模式 | 是 vs 否 | 1.147 | 1.053, 1.249 | 0.002 |
| 实变性失充气模式 | 是 vs 否 | 1.146 | 0.995, 1.321 | 0.059 |
| 机械通气时间 | 1.616 | 0.431, 6.058 | 0.476 | |
| 重力依赖性失充气 | 是 vs 否 | 2.003 | 1.112, 6.387 | 0.028 |
Tab.4 Multivariate COX proportional risk analysis of 28-day prognosis in sepsis patients requiring mechanical ventilation
| 因素 | 95% | |||
|---|---|---|---|---|
| 年龄 | 0.968 | 0.933, 1.005 | 0.086 | |
| 乳酸 | 0.841 | 0.345, 2.05 | 0.703 | |
| 氧合指数 | 0.496 | 0.267, 0.924 | 0.027 | |
| 白细胞介素6 | 1.500 | 1.117, 2.016 | 0.007 | |
| APACHE Ⅱ评分 | 1.007 | 1.001, 1.014 | 0.035 | |
| SOFA评分 | 1.027 | 0.974, 1.083 | 0.320 | |
| 间质性失充气模式 | 是 vs 否 | 0.998 | 0.964, 1.033 | 0.910 |
| 不张性失充气模式 | 是 vs 否 | 1.147 | 1.053, 1.249 | 0.002 |
| 实变性失充气模式 | 是 vs 否 | 1.146 | 0.995, 1.321 | 0.059 |
| 机械通气时间 | 1.616 | 0.431, 6.058 | 0.476 | |
| 重力依赖性失充气 | 是 vs 否 | 2.003 | 1.112, 6.387 | 0.028 |
| [1] |
Gorman EA, O'Kane CM, McAuley DF. Acute respiratory distress syndrome in adults: Diagnosis, outcomes, long-term sequelae, and management[J]. Lancet, 2022, 400(10358):1157-1170.
doi: 10.1016/S0140-6736(22)01439-8 pmid: 36070788 |
| [2] | Joffre J, Hellman J, Ince C, et al. Endothelial responses in sepsis[J]. Am J Respir Crit Care Med, 2020, 202(3):361-370. |
| [3] | Bode C, Weis S, Sauer A, et al. Targeting the host response in sepsis: Current approaches and future evidence[J]. Crit Care, 2023, 27(1):478. |
| [4] | Buda N, Mendrala K, Skoczyński S, et al. Basics of Point-of-Care Lung Ultrasonography[J]. N Engl J Med, 2023, 389(21):e44. |
| [5] | Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome[J]. N Engl J Med, 2013, 368(23):2159-2168. |
| [6] |
Papazian L, Schmidt M, Hajage D, et al. Effect of prone positioning on survival in adult patients receiving venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis[J]. Intensive Care Med, 2022, 48(3):270-280.
doi: 10.1007/s00134-021-06604-x pmid: 35037993 |
| [7] | Wang Q, Zhu J, Chen L, et al. Successful treatment of severe ARDS caused by accidental inhalation of nitric acid fumes with veno-venous ECMO: A case report and literature review[J]. Medicine (Baltimore), 2022, 101(30):e29447. |
| [8] | Haaksma ME, Smit JM, Heldeweg MLA, et al. Extended lung ultrasound to differentiate between pneumonia and atelectasis in critically ill patients: A diagnostic accuracy study[J]. Crit Care Med, 2022, 50(5):750-759. |
| [9] | Smit MR, Hagens LA, Heijnen NFL, et al. Lung ultrasound prediction model for acute respiratory distress syndrome: A multicenter prospective observational study[J]. Am J Respir Crit Care Med, 2023, 207(12):1591-1601. |
| [10] |
Dargent A, Chatelain E, Si-Mohamed S, et al. Lung ultrasound score as a tool to monitor disease progression and detect ventilator-associated pneumonia during COVID-19-associated ARDS[J]. Heart Lung, 2021, 50(5):700-705.
doi: 10.1016/j.hrtlng.2021.05.003 pmid: 34107394 |
| [11] |
Costamagna A, Pivetta E, Goffi A, et al. Clinical performance of lung ultrasound in predicting ARDS morphology[J]. Ann Intensive Care, 2021, 11(1):51.
doi: 10.1186/s13613-021-00837-1 pmid: 33779834 |
| [12] | Smit JM, Haaksma ME, Winkler MH, et al. Lung ultrasound in a tertiary intensive care unit population: A diagnostic accuracy study[J]. Crit Care, 2021, 25(1):339. |
| [13] |
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med, 2021, 47(11):1181-1247.
doi: 10.1007/s00134-021-06506-y pmid: 34599691 |
| [14] |
Chiumello D, Mongodi S, Algieri I, et al. Assessment of lung aeration and recruitment by CT scan and ultrasound in acute respiratory distress syndrome patients[J]. Crit Care Med, 2018, 46(11):1761-1768.
doi: 10.1097/CCM.0000000000003340 pmid: 30048331 |
| [15] |
Wang Y, Shen Z, Lu X, et al. Sensitivity and specificity of ultrasound for the diagnosis of acute pulmonary edema: A systematic review and meta-analysis[J]. Med Ultrason, 2018, 1(1):32-36.
doi: 10.11152/mu-1223 pmid: 29400365 |
| [16] |
Yin W, Zou T, Qin Y, et al. Poor lung ultrasound score in shock patients admitted to the ICU is associated with worse outcome[J]. BMC Pulm Med, 2019, 19(1):1.
doi: 10.1186/s12890-018-0755-9 pmid: 30606165 |
| [17] |
Zou T, Yin W, Diddams M, et al. The global and regional lung ultrasound score can accurately evaluate the severity of lung disease in critically ill patients[J]. J Ultrasound Med, 2020, 39(9):1879-1880.
doi: 10.1002/jum.15278 pmid: 32302014 |
| [18] | 曾学英, 尹万红, 邹同娟, 等. 机械通气的休克患者肺部非重力依赖区超声评分与不良预后的相关性研究[J]. 四川大学学报(医学版), 2019, 50(6):798-802. |
| [19] | Zou T, Yin W, Kang Y. Application of critical care ultrasound in patients with COVID-19: Our experience and perspective[J]. IEEE Trans Ultrason Ferroelectr Freq Control, 2020, 67(11):2197-2206. |
| [20] | Zochios V, Yusuff H, Schmidt M, et al. Acute right ventricular injury phenotyping in ARDS[J]. Intensive Care Med, 2023, 49(1):99-102. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||