

临床荟萃 ›› 2024, Vol. 39 ›› Issue (4): 370-375.doi: 10.3969/j.issn.1004-583X.2024.04.013
收稿日期:2023-08-27
出版日期:2024-04-20
发布日期:2024-06-28
通讯作者:
冶秀鹏, Email:
Received:2023-08-27
Online:2024-04-20
Published:2024-06-28
摘要:
费城染色体阴性(Philadelphia chromosome, Ph-)的骨髓增殖性肿瘤(myeloproliferative neoplasms, MPN)是一类以造血干细胞克隆性增殖为特征的恶性血液病,主要包括真性红细胞增多症、原发性血小板增多症和原发性骨髓纤维化。大多数情况下(Ph-)MPN 的克隆性增殖是通过基因突变驱动的,这些基因突变导致了信号转导通路的失调和细胞因子释放等异常,最终促使血栓形成,发病机制复杂,影响因素多样。本文主要就基因突变,血细胞和炎症状态,年龄、血栓病史和心血管危险因素等影响(Ph-)MPN患者血栓形成的机制和血栓的防治进行综述,旨在为临床提供一定的参考。
中图分类号:
陈岚, 李叶琼, 冶秀鹏. 费城染色体阴性骨髓增殖性肿瘤患者血栓形成影响因素[J]. 临床荟萃, 2024, 39(4): 370-375.
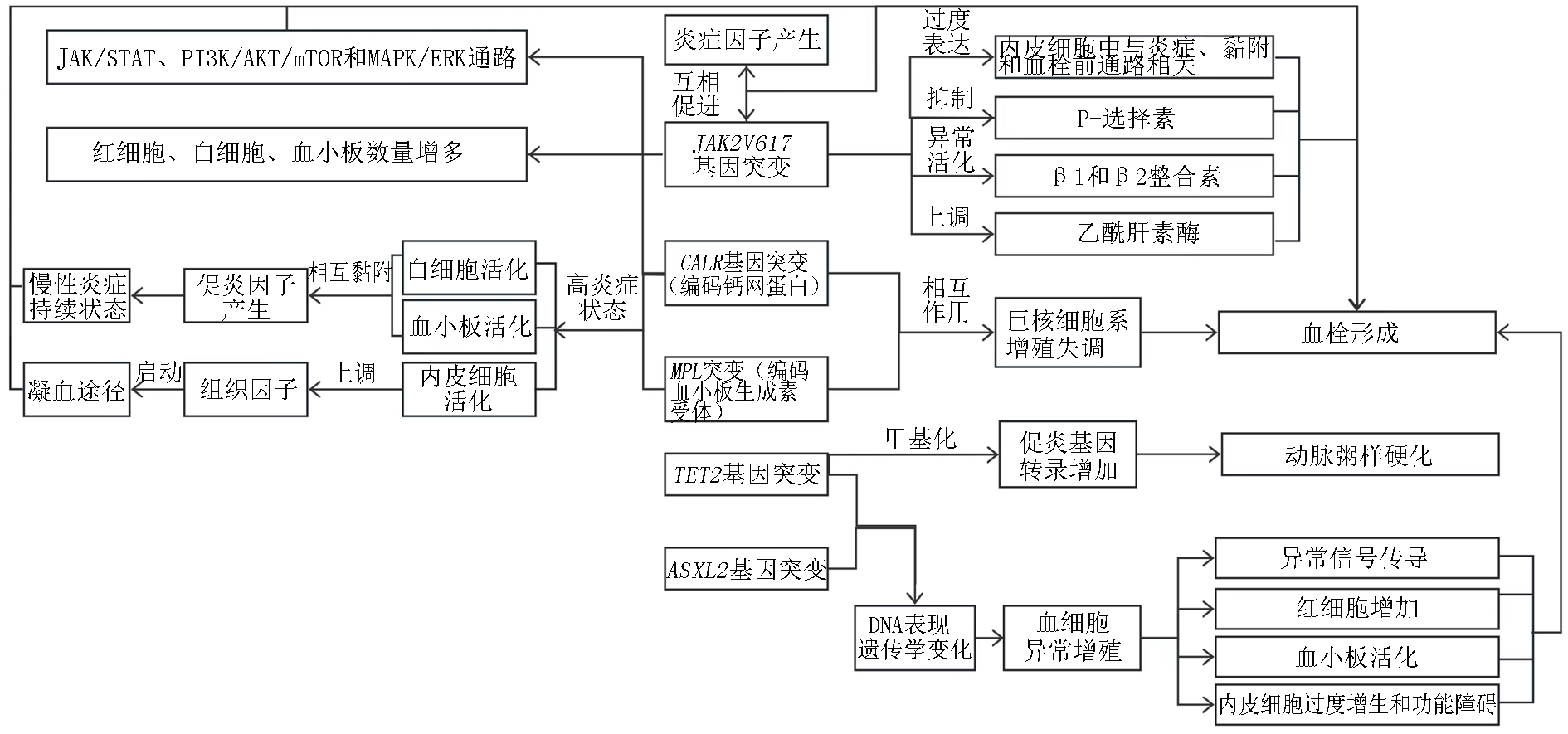
图1 基因突变致血栓形成机制 注:JAK:非受体型酪氨酸蛋白激酶;STAT:信号传导和转录激活蛋白;PI3K:磷脂酰肌醇3;mTOR:哺乳动物的雷帕霉素靶蛋白;MAPK/EPK:丝裂原活化蛋白激酶
Fig 1. Mechanism of thrombosis caused by gene mutations Note:JAK:janus kinase;STAT:signal transducer and activator of transcription;PI3K:phosphatidylinositol 3;mTOR:mammalian target of rapamycin;MAPK/EPK:mitogen-activated protein kinase
| [1] | De Stefano V, Vannucchi AM, Ruggeri M, et al. Splanchnic vein thrombosis in myeloproliferative neoplasms: Risk factors for recurrences in a cohort of 181 patients[J]. Blood Cancer J, 2016, 6(11):e493. |
| [2] | Rungjirajittranon T, Owattanapanich W, Ungprasert P, et al. A systematic review and meta-analysis of the prevalence of thrombosis and bleeding at diagnosis of Philadelphia-negative myeloproliferative neoplasms[J]. BMC cancer, 2019, 19:1-9. |
| [3] | Song IC, Yeon SH, Lee MW, et al. Thrombotic and hemorrhagic events in 2016 World Health Organization-defined Philadelphia-negative myeloproliferative neoplasm[J]. Korean J Intern Med, 2021, 36(5):1190. |
| [4] |
Kim J, Byun JM, Hong J, et al. Incidence, characteristics and risk factors of thromboembolic events in East Asian patients with BCR-ABL1 negative myeloproliferative neoplasms[J]. Scientific Reports, 2021, 11(1):17819.
doi: 10.1038/s41598-021-97464-4 pmid: 34497309 |
| [5] | Gecht J, Tsoukakis I, Kricheldorf K, et al. Kidney dysfunction is associated with thrombosis and disease severity in myeloproliferative neoplasms: Implications from the German Study Group for MPN Bioregistry[J]. Cancers, 2021, 13(16):4086. |
| [6] | Zhang Y, Zhou Y, Wang Y, et al. Thrombosis among 1537 patients with JAK2V617F-mutated myeloproliferative neoplasms: Risk factors and development of a predictive model[J]. Cancer medicine, 2020, 9(6):2096-2105. |
| [7] | Wille K, Deventer E, Sadjadian P, et al. Arterial and venous thromboembolic complications in 832 patients with BCR-ABL-negative myeloproliferative neoplasms[J]. Hamostaseologie, 2023. |
| [8] | Mulas O, Mola B, Costa A, et al. Renin-angiotensin inhibitors reduce thrombotic complications in essential thrombocythemia and polycythemia vera patients with arterial hypertension[J]. Ann Hematol, 2023, 102(10):2717-2723. |
| [9] | 秦福丽, 郭志强. JAK2阳性骨髓增殖性肿瘤患者65例临床特征分析[J]. 临床内科杂志, 2020, 37(10):737-739. |
| [10] | 刘雯丽. Ⅰ JAK2突变在动脉粥样硬化与血栓形成中的作用和机制研究 Ⅱ ω3多不饱和脂肪酸代谢产物在早期非酒精性脂肪肝中的作用和机制研究[D]. 天津医科大学, 2018. |
| [11] |
Singh K VP, Ahuja A, et al. Correlation of thrombosis and clinicohematological parameters with JAK2V617F mutation in Philadelphia-negative CMPNs: A study from India[J]. J Lab Physicians, 2022, 14(4):394-397.
doi: 10.1055/s-0042-1757230 pmid: 36531548 |
| [12] | Bader MS, Meyer SC. JAK2 in myeloproliferative neoplasms: still a protagonist[J]. Pharmaceuticals, 2022, 15(2):160. |
| [13] | 胡慧平. 骨髓增殖性肿瘤JAK2V617F基因突变与血栓栓塞相关性分析[J]. 中国药物与临床, 2020, 20(21):3597-3599. |
| [14] | Olschok K, Altenburg B, et al. The telomerase inhibitor imetelstat differentially targets JAK2V617F versus CALR mutant myeloproliferative neoplasm cells and inhibits JAK-STAT signaling[J]. Front Oncol, 2023, 13:1277453. |
| [15] | Fan C, Zhang Y, Yang R, et al. Leukocyte-associated immunoglobulin-like receptor 1 (LAIR-1) inhibits proliferation and promotes apoptosis of human HEL cells with JAK2V617F mutation by blocking the JAK/STAT and PI3K/AKT signaling pathways[J]. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi, 2024, 40(3):207-214. |
| [16] | Dunbar A, Bowman RL, Park Y, et al. JAK2V617F reversible activation shows an essential requirement for JAK2V617F in myeloproliferative neoplasms (MPNs)[J]. Blood, 2022, 140(Supplement 1):803-804. |
| [17] |
Kesarwani M, Kincaid Z, Azhar M, et al. MAPK-negative feedback regulation confers dependence to JAK2V617F signaling[J]. Leukemia, 2023, 37(8):1686-1697.
doi: 10.1038/s41375-023-01959-0 pmid: 37430058 |
| [18] | Reeves BN, Beckman JD. Novel pathophysiological mechanisms of thrombosis in myeloproliferative neoplasms[J]. Curr Hematol Malig Rep, 2021, 16:304-313. |
| [19] | Bhuria V, Baldauf CK, Schraven B, et al. Thromboinflammation in myeloproliferative neoplasms (MPN)-a puzzle still to be solved[J]. Int J Mol Sci, 2022, 23(6):3206. |
| [20] | Papageorgiou L, Elalamy I, Vandreden P, et al. Thrombotic and hemorrhagic issues associated with myeloproliferative neoplasms[J]. Clin Appl Thromb Hemost, 2022, 28:10760296221097969. |
| [21] | Castiglione M, Jiang YP, Mazzeo C, et al. Endothelial JAK2V617F mutation leads to thrombosis, vasculopathy, and cardiomyopathy in a murine model of myeloproliferative neoplasm[J]. J Thromb Haemost, 2020, 18(12):3359-3370. |
| [22] | Hamed H, Abdelhady EA, Elrazzaz MK, et al. Value of assessment of factor XI in patients with myeloproliferative neoplasms with and without thrombotic events[J]. J Hematol Egy, 2020, 45(1):40. |
| [23] | Guijarro-Hernández A, Eder-Azanza L, Hurtado C, et al. Transcriptomic analysis reveals JAK2/MPL-independent effects of calreticulin mutations in a C. elegans model[J]. Cells, 2023, 12(1):186. |
| [24] | Behrens K, Kauppi M, Viney EM, et al. Differential in vivo roles of MPL cytoplasmic tyrosine residues in murine hematopoiesis and myeloproliferative disease[J]. Leukemia, 2024:1-11. |
| [25] | Furuya C, Hashimoto Y, Morishita S, et al. MPL gene mutation is a possible risk factor for thrombosis in patients with essential thrombocythemia in Japan[J]. Hematology, 2023, 28(1):2229131. |
| [26] |
Marty C, Pecquet C, Nivarthi H, et al. Calreticulin mutants in mice induce an MPL-dependent thrombocytosis with frequent progression to myelofibrosis[J]. Blood, 2016, 127(10):1317-1324.
doi: 10.1182/blood-2015-11-679571 pmid: 26608331 |
| [27] |
Pich A, Riera L, Francia di Celle P, et al. JAK2V617F, CALR, and MPL mutations and bone marrow histology in patients with essential thrombocythaemia[J]. Acta Haematologica, 2018, 140(4):234-239.
doi: 10.1159/000493970 pmid: 30404086 |
| [28] | Lussana F, Carobbio A, Salmoiraghi S, et al. Driver mutations (JAK2V617F, MPLW515L/K or CALR), pentraxin-3 and C-reactive protein in essential thrombocythemia and polycythemia vera[J]. J Hematol Oncol, 2017, 10(1):54. |
| [29] |
Marty C, Pecquet C, Nivarthi H, et al. Calreticulin mutants in mice induce an MPL-dependent thrombocytosis with frequent progression to myelofibrosis[J]. Blood, 2016, 127(10):1317-1324.
doi: 10.1182/blood-2015-11-679571 pmid: 26608331 |
| [30] | Faille D, Lamrani L, Loyau S, et al. Interferon alpha therapy increases pro-thrombotic biomarkers in patients with myeloproliferative neoplasms[J]. Cancers (Basel), 2020, 12(4):992. |
| [31] |
Rumi E, Pietra D, Pascutto C, et al. Clinical effect of driver mutations of JAK2, CALR, or MPL in primary myelofibrosis[J]. Blood, 2014, 124(7):1062-1069.
doi: 10.1182/blood-2014-05-578435 pmid: 24986690 |
| [32] |
Helbig G. Classical Philadelphia-negative myeloproliferative neoplasms: Focus on mutations and JAK2 inhibitors[J]. Med Oncol, 2018, 35(9):119.
doi: 10.1007/s12032-018-1187-3 pmid: 30074114 |
| [33] | Chan TS, Hwang YY, Tse E. Risk assessment of venous thromboembolism in hematological cancer patients: A review[J]. Expert Rev Hematol, 2020, 13(5):471-480. |
| [34] | Wang Z, Liu W, Wang D, et al. TET2 mutation may be more valuable in predicting thrombosis in ET patients compared to PV patients: A preliminary report[J]. J Clin Med, 2022, 11(22):6615. |
| [35] | Chia YC, Siti Asmaa MJ, Ramli M, et al. Molecular genetics of thrombotic myeloproliferative neoplasms: Implications in precision oncology[J]. Diagnostics (Basel), 2023, 13(1):163. |
| [36] |
Aswad MH, Kissová J, Ovesná P, et al. The clinical significance of circulating microparticles concerning thrombosis in BCR/ABL1-negative myeloproliferative neoplasms[J]. In Vivo, 2021, 35(6):3345-3353.
doi: 10.21873/invivo.12632 pmid: 34697168 |
| [37] | 马强. 血细胞计数预测骨髓增殖性肿瘤患者血栓形成的意义[J]. 宁夏医学杂志, 2020, 42(8):735-738. |
| [38] | 冯一鸣, 史家岚. 血小板在骨髓增殖性肿瘤血栓形成中的作用机制[J]. 中国临床研究, 2021, 34(12):1700-1704, 1710. |
| [39] |
Marin Oyarzún CP, Heller PG. Platelets as mediators of thromboinflammation in chronic myeloproliferative neoplasms[J]. Front Immunol, 2019, 10:1373.
doi: 10.3389/fimmu.2019.01373 pmid: 31258539 |
| [40] | Nasillo V, Riva G, Paolini A, et al. Inflammatory microenvironment and specific T cells in myeloproliferative neoplasms: Immunopathogenesis and novel immunotherapies[J]. Int J Mol Sci, 2021, 22(4):1906. |
| [41] | Masselli E, Pozzi G, Gobbi G, et al. Cytokine profiling in myeloproliferative neoplasms: Overview on phenotype correlation, outcome prediction, and role of genetic variants[J]. Cells, 2020, 9(9):2136. |
| [42] | Ferrer-Marín F, Cuenca-Zamora EJ, Guijarro-Carrillo PJ, et al. Emerging role of neutrophils in the thrombosis of chronic myeloproliferative neoplasms[J]. Int J Mol Sci, 2021, 22(3):1143. |
| [43] | Šefer D, Milji'c P, Kraguljac-Kurtovi'c N, et al. Correlation between leukocyte-platelet aggregates and thrombosis in myeloproliferative neoplasms[J]. Int J Lab Hematol, 2022, 44(2):302-312. |
| [44] | Huang MJ, He ZP, Tian HY, et al. Clinical features and risk factors of vein thrombosis in 259 patients with chronic myelofiberation neoplasms[J]. Zhonghua Xue Ye Xue Za Zhi, 2017, 38(7):623-625. |
| [45] |
Panova-Noeva M, Marchetti M, Spronk HM, et al. Platelet-induced thrombin generation by the calibrated automated thrombogram assay is increased in patients with essential thrombocythemia and polycythemia vera[J]. Am J Hematol, 2011, 86(4):337-342.
doi: 10.1002/ajh.21974 pmid: 21442635 |
| [46] | Schafer AI. Thrombotic, vascular, and bleeding complications of the myeloproliferative neoplasms[J]. Hematol Oncol Clin North Am, 2021, 35(2):305-324. |
| [47] | Vannucchi AM, Guglielmelli P. Acute myocardial infarction and chronic myeloproliferative neoplasms: Friend and enemy, depending on circumstances[J]. JACC Cardio Oncol, 2023, 5(4):469-471. |
| [48] |
Pasquer H, Daltro de Oliveira R, Vasseur L, et al. Distinct clinico-molecular arterial and venous thrombosis scores for myeloproliferative neoplasms risk stratification[J]. Leukemia, 2024, 38(2):326-339.
doi: 10.1038/s41375-023-02114-5 pmid: 38148396 |
| [49] | Baysal M, Bayrak M, Eʂkazan AE. Current evidence on the use of direct oral anticoagulants in patients with myeloproliferative neoplasm: A systematic review[J]. Expert Rev Hematol, 2023, 16(2):131-140. |
| [50] | Al-Mashdali AF, Aldapt MB, Rahhal A, et al. Pediatric Philadelphia-Negative myeloproliferative neoplasms in the era of WHO classification: A systematic review[J]. Diagnostics (Basel), 2023, 13(3):377. |
| [1] | 王娇燕, 严超, 应可净. 气道慢性炎症性疾病并发静脉血栓栓塞症的研究进展[J]. 临床荟萃, 2024, 39(5): 470-474. |
| [2] | 马丽娜, 焦焕利, 曹振华. 慢性非缺血性心功能衰竭合并血栓栓塞及药物治疗研究进展[J]. 临床荟萃, 2024, 39(1): 75-79. |
| [3] | 左腾, 王俊祥. 血清阴性类风湿关节炎发病机制的研究进展[J]. 临床荟萃, 2023, 38(8): 753-756. |
| [4] | 贾丽娜, 吴美妮, 尹昌浩. 2型糖尿病认知功能障碍发病机制的研究进展[J]. 临床荟萃, 2023, 38(6): 554-558. |
| [5] | 邹琳, 崔轶霞, 张娜娜, 陈思荣. 类风湿关节炎合并骨质疏松症发病机制和相关治疗药物对骨质疏松症影响的研究进展[J]. 临床荟萃, 2023, 38(3): 279-284. |
| [6] | 彭艳, 白碧玥, 朱晓峰, 尹昌浩. 酒精使用障碍患者认知功能损害发病机制的研究进展[J]. 临床荟萃, 2023, 38(12): 1131-1134. |
| [7] | 梁炳松, 李育英, 张岐平, 陈英道, 李健. 替罗非班治疗进展性穿支动脉梗死临床疗效的相关因素[J]. 临床荟萃, 2023, 38(12): 1091-1094. |
| [8] | 白碧玥, 彭艳, 朱晓峰, 尹昌浩. 缺血性脑卒中影响侧支循环建立因素的研究进展[J]. 临床荟萃, 2023, 38(11): 1034-1037. |
| [9] | 杨晓蓉, 周淑红, 潘亮, 郭莉江. 结缔组织病相关肺动脉高压的发病机制及其筛查的研究进展[J]. 临床荟萃, 2023, 38(10): 944-948. |
| [10] | 刘向东, 蔡延东, 秦延军, 李云松, 李亮, 高瑞姣, 任磊, 张彦荣. 运动性横纹肌溶解症并发急性肾功能不全及透析管相关性血栓1例并文献复习[J]. 临床荟萃, 2022, 37(9): 831-833. |
| [11] | 常雅君, 郭卫娜, 郭巧珍, 王天俊. 以孤立性头痛为主要表现的颅内静脉窦血栓1例并文献复习[J]. 临床荟萃, 2022, 37(3): 271-274. |
| [12] | 曾晓晴, 庄伟端, 陈丽芬. 卒中后癫痫发作发病机制的研究进展[J]. 临床荟萃, 2022, 37(2): 174-177. |
| [13] | 鲁奎, 郑龙. 急性脑梗死DWI阴性原因分析[J]. 临床荟萃, 2021, 36(8): 753-756. |
| [14] | 张小乐, 蔡肇栩, 张贺琼, 王洋洋, 陆少云, 杨春万. 血栓弹力图在初发急性心肌梗死患者中的临床应用[J]. 临床荟萃, 2021, 36(2): 125-128. |
| [15] | 尹园园, 任慧玲. 脑静脉窦血栓形成作为首发的神经白塞病1例报告并文献复习[J]. 临床荟萃, 2021, 36(2): 162-167. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
