Clinical Focus ›› 2021, Vol. 36 ›› Issue (8): 677-684.doi: 10.3969/j.issn.1004-583X.2021.08.001
Effects of goal-directed fluid therapy on intraoperative balance between oxygen delivery and consumption and postoperative outcomes in thoracic surgery patients: a meta-analysis
Li Guanzhu1, Lai Yuan2, Zheng Xiaozhuo3, Jiang Ran3, Wei Ke3( )
)
- 1. Department of Anesthesiology,Second Affiliated Hospital, Guangzhou University of Chinese Medicine & Guangdong Provincial Hospital of Chinese Medicine, Guangzhou 510120, China
2. Department of Anesthesiology,Affiliated Hospital of Chongqing Three Gorges Medical College, Chongqing 404000, China
3. Department of Anesthesiology, the First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China
-
Received:2020-07-04Online:2021-08-20Published:2021-08-30 -
Contact:Wei Ke E-mail:wk202448@hospital-cumq.com
CLC Number:
Cite this article
Li Guanzhu, Lai Yuan, Zheng Xiaozhuo, Jiang Ran, Wei Ke. Effects of goal-directed fluid therapy on intraoperative balance between oxygen delivery and consumption and postoperative outcomes in thoracic surgery patients: a meta-analysis[J]. Clinical Focus, 2021, 36(8): 677-684.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2021.08.001
| 纳入研究 | 样本量(例) | 年龄(岁) | 手术类型 | 干预措施 | 结局指标 | |||
|---|---|---|---|---|---|---|---|---|
| G | C | G | C | G | C | |||
| Zhang 2013 [ | 30 | 30 | 59.9±8.9 | 61.0±8.7 | 胸腔镜下肺叶切除术 | 基于SVV、CI的目标导向法 | 限制法 | ①③④⑤⑥ |
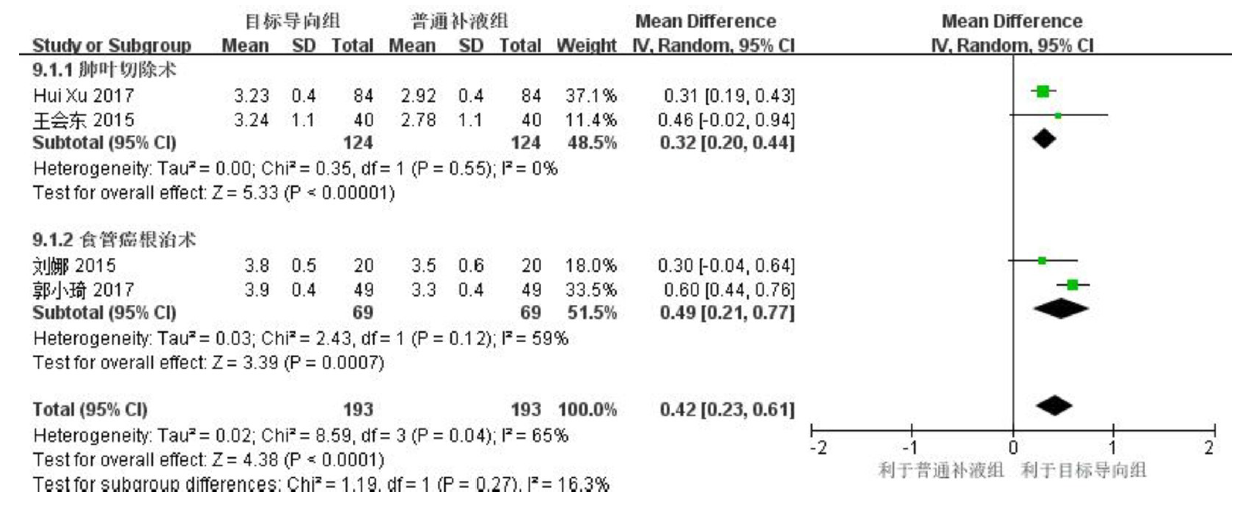
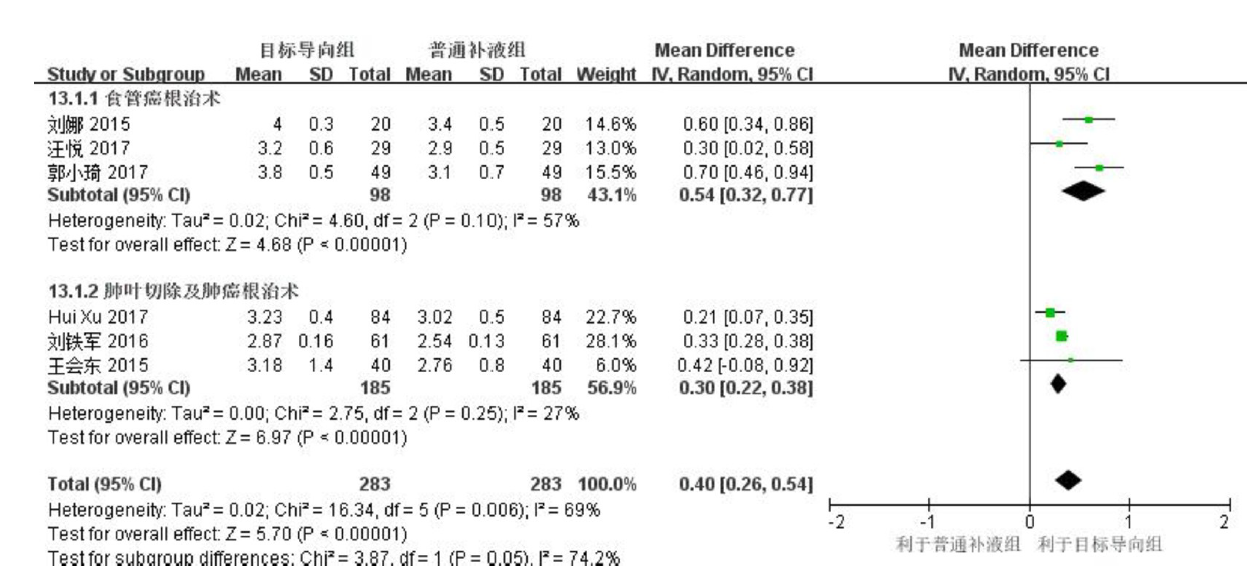
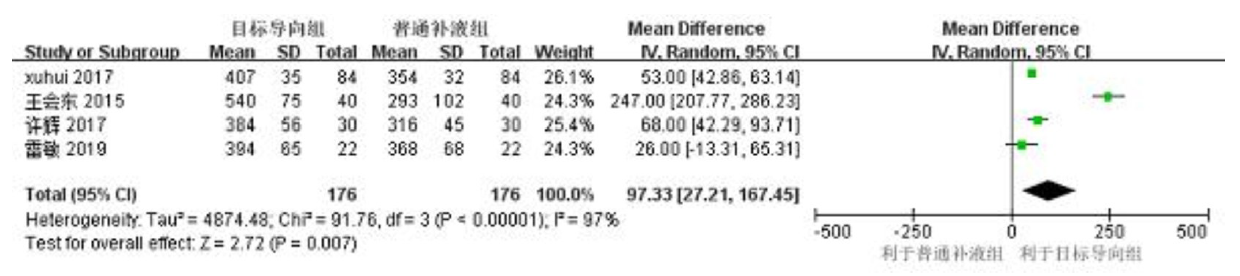
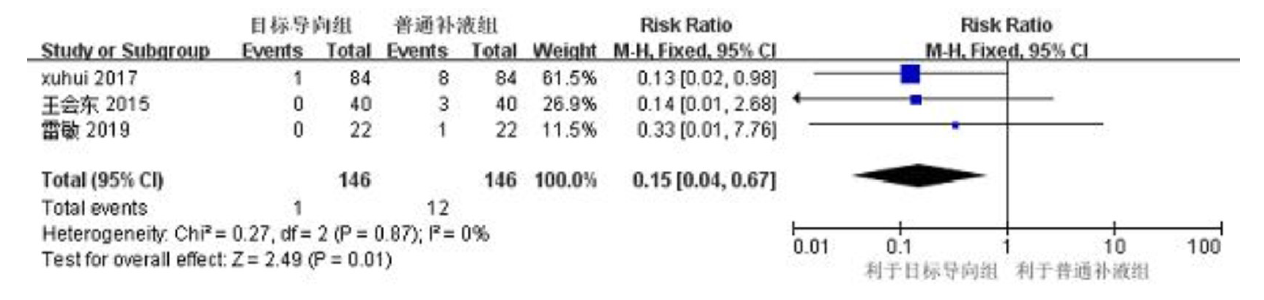
| Xu 2017 [ | 84 | 84 | 49±6 | 49±5 | 胸腔镜下肺叶切除术 | 基于SVV、CI的目标导向法 | 限制法 | ②③④⑤⑥ |
| 刘娜 2015[ | 20 | 20 | 69.1±4.2 | 68.5±3.8 | 食管癌根治术 | 基于ITBVI的目标导向法 | 限制法 | ①② |
| 王会东 2015[ | 40 | 40 | 47±12 | 53±9 | 肺叶切除术 | 基于SVV的目标导向法 | 开放法 | ②③④ |
| 雷敏 2019[ | 22 | 22 | 56±8 | 58±8 | 胸腔镜下肺叶切除术 | 基于SVV的目标导向法 | 开放法 | ①④⑤⑥ |
| 许辉 2017[ | 30 | 30 | 51±6 | 52±4 | 肺癌根治术 | 基于SVV、CI的目标导向法 | 限制法 | ③ |
| 汪悦 2017[ | 29 | 29 | 68±4 | 67±5 | 食管癌根治术 | 基于SVV、CI的目标导向法 | 限制法 | ② |
| 刘铁军 2016[ | 61 | 61 | 66.1±5.8 | 66.3±4.5 | 肺癌根治术 | 基于SVV、CI的目标导向法 | 开放法 | ①② |
| 郭小琦 2017[ | 49 | 49 | 70.5±6.3 | 69.1±8.2 | 食管癌根治术 | 基于ITBVI的目标导向法 | 正常法 | ①② |
| 白晓蕾 2019[ | 20 | 20 | 59.75±3.83 | 60.10±3.10 | 胸腔镜下肺叶切除术 | 基于LVETc及SV的目标导向法 | 限制法 | ①④⑤⑥ |
| 杨丽 2015[ | 20 | 20 | 57±6 | 58±9 | 开胸下肺叶切除术 | 基于SVV的目标导向法 | 正常法 | ① |
| 纳入研究 | 样本量(例) | 年龄(岁) | 手术类型 | 干预措施 | 结局指标 | |||
|---|---|---|---|---|---|---|---|---|
| G | C | G | C | G | C | |||
| Zhang 2013 [ | 30 | 30 | 59.9±8.9 | 61.0±8.7 | 胸腔镜下肺叶切除术 | 基于SVV、CI的目标导向法 | 限制法 | ①③④⑤⑥ |
| Xu 2017 [ | 84 | 84 | 49±6 | 49±5 | 胸腔镜下肺叶切除术 | 基于SVV、CI的目标导向法 | 限制法 | ②③④⑤⑥ |
| 刘娜 2015[ | 20 | 20 | 69.1±4.2 | 68.5±3.8 | 食管癌根治术 | 基于ITBVI的目标导向法 | 限制法 | ①② |
| 王会东 2015[ | 40 | 40 | 47±12 | 53±9 | 肺叶切除术 | 基于SVV的目标导向法 | 开放法 | ②③④ |
| 雷敏 2019[ | 22 | 22 | 56±8 | 58±8 | 胸腔镜下肺叶切除术 | 基于SVV的目标导向法 | 开放法 | ①④⑤⑥ |
| 许辉 2017[ | 30 | 30 | 51±6 | 52±4 | 肺癌根治术 | 基于SVV、CI的目标导向法 | 限制法 | ③ |
| 汪悦 2017[ | 29 | 29 | 68±4 | 67±5 | 食管癌根治术 | 基于SVV、CI的目标导向法 | 限制法 | ② |
| 刘铁军 2016[ | 61 | 61 | 66.1±5.8 | 66.3±4.5 | 肺癌根治术 | 基于SVV、CI的目标导向法 | 开放法 | ①② |
| 郭小琦 2017[ | 49 | 49 | 70.5±6.3 | 69.1±8.2 | 食管癌根治术 | 基于ITBVI的目标导向法 | 正常法 | ①② |
| 白晓蕾 2019[ | 20 | 20 | 59.75±3.83 | 60.10±3.10 | 胸腔镜下肺叶切除术 | 基于LVETc及SV的目标导向法 | 限制法 | ①④⑤⑥ |
| 杨丽 2015[ | 20 | 20 | 57±6 | 58±9 | 开胸下肺叶切除术 | 基于SVV的目标导向法 | 正常法 | ① |
| [1] |
De la Gala F, Piñeiro P, Reyes A, et al. Effect of intraoperative paravertebral or intravenous lidocaine versus control during lung resection surgery on postoperative complications: A randomized controlled trial[J]. Trials, 2019, 20(1):622.
doi: 10.1186/s13063-019-3677-9 URL |
| [2] |
Lederman D, Easwar J, Feldman J, et al. Anesthetic considerations for lung resection: Preoperative assessment, intraoperative challenges and postoperative analgesia[J]. Ann Transl Med, 2019, 7(15):356.
doi: 10.21037/atm.2019.03.67 pmid: 31516902 |
| [3] | 黄剑, 柳开忠, 刘文生. 胸部恶性肿瘤根治术后患者目标导向液体治疗的价值研究[J]. 中华危重症医学杂志, 2017, 10(3):182-187. |
| [4] | Wrzosek A, Jakowicka-Wordliczek J, Zajaczkowska R, et al. Perioperative restrictive versus goal-directed fluid therapy for adults undergoing major non-cardiac surgery[J]. Cochrane Database Syst Rev, 2019, 12:CD012767. |
| [5] |
Hasanin A, Zanata T, Osman S, et al. Pulse pressure variation-guided fluid therapy during supratentorial brain tumour excision: A randomized controlled trial[J]. Open Access Maced J Med Sci, 2019, 7(15):2474-2479.
doi: 10.3889/oamjms.2019.682 pmid: 31666850 |
| [6] |
Froghi F, Soggiu F, Ricciardi F, et al. Ward-based Goal-Directed Fluid Therapy (GDFT) in Acute Pancreatitis (GAP) trial: Study protocol for a feasibility randomised controlled trial[J]. BMJ Open, 2019, 9(10):e028783.
doi: 10.1136/bmjopen-2018-028783 URL |
| [7] |
Zhang J, Chen CQ, Lei XZ, et al. Goal-directed fluid optimization based on stroke volume variation and cardiac index during one-lung ventilation in patients undergoing thoracoscopy lobectomy operations: A pilot study[J]. Clinics (Sao Paulo), 2013, 68(7):1065-1070.
doi: 10.6061/clinics/2013(07)27 pmid: 23917675 |
| [8] |
Xu H, Shu SH, Wang D, et al. Goal-directed fluid restriction using stroke volume variation and cardiac index during one-lung ventilation: A randomized controlled trial[J]. J Thorac Dis, 2017, 9(9):2992-3004.
doi: 10.21037/jtd URL |
| [9] | 刘娜, 徐悦利, 李汝鸿, 等. 不同容量治疗方案对老年食管癌切除术患者血流动力学、血乳酸及氧供需平衡的影响[J]. 中国煤炭工业医学杂志, 2015, 18(6):966-970. |
| [10] | 王会东, 冀晋杰, 徐学敏, 等. 麻醉期间目标导向液体治疗对肺叶切除术后急性肺损伤的影响[J]. 解放军医学院学报, 2015, 36(11):1109-1112. |
| [11] | 雷敏, 鲍琪, 钟泰迪. 每搏变异度指导的液体目标导向治疗在胸腔镜手术中的应用[J]. 中国医药, 2019, 14(2):275-278. |
| [12] | 许辉, 疏树华, 王迪, 等. 目标导向液体治疗单肺通气肺癌根治术患者术中肺功能及中心静脉血炎症因子水平观察[J]. 山东医药, 2017, 57(19):94-96. |
| [13] | 汪悦, 李娟, 康芳, 等. 目标导向液体治疗对老年单肺通气患者局部脑氧饱和度及血流动力学的影响[J]. 临床麻醉学杂志, 2017, 33(9):837-841. |
| [14] | 刘铁军, 杨占魁, 高晓增, 等. 目标导向液体治疗对老年肺癌根治术患者术中凝血状态的影响[J]. 浙江临床医学, 2016, 18(3):516-517. |
| [15] | 郭小琦, 薛锋, 王鹏国, 等. 目标导向液体治疗对老年食管癌根治术患者围手术期血流动力学、血乳酸及细胞免疫功能的影响[J]. 癌症进展, 2017, 15(10):1209-1212. |
| [16] | 白晓蕾, 解雅英, 都义日, 等. 经食管超声心动描计术引导下目标导向液体治疗在肺叶切除术中的应用[J]. 中国现代医学杂志, 2019, 29(15):102-107. |
| [17] | 杨丽. 每搏量变异度在胸科手术全麻复合硬膜外麻醉患者中临床应用[D]. 中国医科大学, 2015:1-31. |
| [18] |
Coeckelenbergh S, Delaporte A, Ghoundiwal D, et al. Pleth variability index versus pulse pressure variation for intraoperative goal-directed fluid therapy in patients undergoing low-to-moderate risk abdominal surgery: A randomized controlled trial[J]. BMC Anesthesiol, 2019, 19(1):34.
doi: 10.1186/s12871-019-0707-9 pmid: 30851740 |
| [19] | Yin K, Ding J, Wu Y, et al. Goal-directed fluid therapy based on noninvasive cardiac output monitor reduces postoperative complications in elderly patients after gastrointestinal surgery: A randomized controlled trial[J]. Pak J Med Sci, 2018, 34(6):1320-1325. |
| [20] |
Torregiani G, Claroni C, Covotta M, et al. Impact of a goal-directed fluid therapy on length of hospital stay and costs of hepatobiliarypancreatic surgery: A prospective observational study[J]. J Comp Eff Res, 2018, 7(12):1171-1179.
doi: 10.2217/cer-2018-0041 URL |
| [21] | Jin J, Min S, Liu D, et al. Clinical and economic impact of goal-directed fluid therapy during elective gastrointestinal surgery[J]. Perioper Med (Lond), 2018, 7:22. |
| [22] |
Wu H, Wang W, Zhao G, et al. Effect of intraoperative fluid administration on perioperative outcomes in patients undergoing McKeown esophagogastrectomy[J]. Chin J Cancer Res, 2019, 31(5):742-748.
doi: 10.21147/j.issn.1000-9604.2019.05.04 URL |
| [23] |
Deng QW, Tan WC, Zhao BC, et al. Is goal-directed fluid therapy based on dynamic variables alone sufficient to improve clinical outcomes among patients undergoing surgery? A meta-analysis[J]. Crit Care, 2018, 22(1):298.
doi: 10.1186/s13054-018-2251-2 URL |
| [24] |
Weinberg L, Mackley L, Ho A, et al. Impact of a goal directed fluid therapy algorithm on postoperative morbidity in patients undergoing open right hepatectomy: A single centre retrospective observational study[J]. BMC Anesthesiol, 2019, 19(1):135.
doi: 10.1186/s12871-019-0803-x URL |
| [25] |
Bahlmann H, Hahn RG, Nilsson L, et al. Pleth variability index or stroke volume optimization during open abdominal surgery: A randomized controlled trial[J]. BMC Anesthesiol, 2018, 18(1):115.
doi: 10.1186/s12871-018-0579-4 pmid: 30121072 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||