Clinical Focus ›› 2024, Vol. 39 ›› Issue (8): 684-692.doi: 10.3969/j.issn.1004-583X.2024.08.002
Previous Articles Next Articles
Efficacy and safety of laparoscopic Heller myotomy versus peroral endoscopic myotomy on esophageal achalasia: A meta-analysis
Ye Zhibo1, Li Keyong1, Que Changhao1, Wang Yaping1, Gou Yunjiu2( )
)
- 1. First School of Clinical Medical,Gansu University of Chinese Medicine,Lanzhou 730000,China
2. Department of Thoracic Surgery,Gansu Provincial Hospital,Lanzhou 730000,China
-
Received:2024-03-06Online:2024-08-20Published:2024-09-03 -
Contact:Gou Yunjiu,Email: gouyunjiu@163.com
CLC Number:
Cite this article
Ye Zhibo, Li Keyong, Que Changhao, Wang Yaping, Gou Yunjiu. Efficacy and safety of laparoscopic Heller myotomy versus peroral endoscopic myotomy on esophageal achalasia: A meta-analysis[J]. Clinical Focus, 2024, 39(8): 684-692.
share this article
Add to citation manager EndNote|Ris|BibTeX
URL: https://huicui.hebmu.edu.cn/EN/10.3969/j.issn.1004-583X.2024.08.002
| 纳入研究 | 研究方法 | 国家 | BMI | 手术方式 | 例数 | 年龄(岁) | 男/女(例) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LHM组 | POEM组 | LHM组 | POEM组 | LHM组 | POEM组 | LHM组 | POEM组 | ||||||
| 蒋彬[ | R | 中国 | NA | NA | LHM | POEM | 61 | 44.1±14.8 | 45.4±14.6 | 14/16 | 18/13 | ||
| Hungness[ | R | 美国 | 25 | 27 | LHM | POEM | 73 | 49 | 38 | 29/26 | 13/5 | ||
| Ujiki[ | PNC | 美国 | 26.5±1.3 | 25.3±1.1 | LHM | POEM | 39 | 60.2±4.7 | 64.1±4.8 | 12/9 | 13/5 | ||
| Bhayani[ | R | 美国 | NA | NA | LHM | POEM | 101 | 57 56 | 31/33 | 19/18 | |||
| Kumagai[ | PNC | 瑞典 | 22.9±3.6 | 23.3±3.7 | LHM | POEM | 83 | 45 | 45.5 | 19/22 | 27/15 | ||
| Chan[ | R | 中国 | NA | NA | LHM | POEM | 56 | 38.4 | 48.2 | 11/12 | 12/21 | ||
| Leeds[ | PNC | 美国 | 28.8±5.2 | 25.7±4.0 | LHM | POEM | 23 | 52.7±12.4 | 52.0±16.9 | 6/5 | 4/8 | ||
| Peng[ | R | 中国 | NA | NA | LHM | POEM | 31 | 44.7±21.6 | 37.5±13.0 | 8/10 | 8/5 | ||
| Werner[ | RCT | 美国 | 24.5±4.5 | 24.8±4.6 | LHM | POEM | 221 | 48.6±14.6 | 41.7±14.8 | 60/49 | 68/44 | ||
| Wirsching[ | PNC | 美国 | 27 | 30 | LHM | POEM | 51 | 56.6 | 58 | 12/16 | 11/12 | ||
| Ali[ | R | 巴西 | NA | NA | LHM | POEM | 40 | 44.2±13.2 | 44.9±14.6 | 14/6 | 12/8 | ||
| Costantini[ | PNC | 意大利 | 22 | 23 | LHM | POEM | 280 | 48 | 47 | 73/67 | 70/70 | ||
| Attaar[ | R | 美国 | 26.8±5.7 | 27.1±6.7 | LHM | POEM | 159 | 58.0±19.0 | 64.0±16.0 | 19/14 | 62/64 | ||
| Podboy[ | R | 美国 | NA | NA | LHM | POEM | 98 | 58.0±2.4 | 59.2±2.4 | 10/33 | 22/33 | ||
| Wong[ | PNC | 马来西亚 | NA | NA | LHM | POEM | 123 | 48.1±17.3 | 41.7±14.8 | 31/29 | 29/34 | ||
Tab.1 Baseline information of included studies
| 纳入研究 | 研究方法 | 国家 | BMI | 手术方式 | 例数 | 年龄(岁) | 男/女(例) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LHM组 | POEM组 | LHM组 | POEM组 | LHM组 | POEM组 | LHM组 | POEM组 | ||||||
| 蒋彬[ | R | 中国 | NA | NA | LHM | POEM | 61 | 44.1±14.8 | 45.4±14.6 | 14/16 | 18/13 | ||
| Hungness[ | R | 美国 | 25 | 27 | LHM | POEM | 73 | 49 | 38 | 29/26 | 13/5 | ||
| Ujiki[ | PNC | 美国 | 26.5±1.3 | 25.3±1.1 | LHM | POEM | 39 | 60.2±4.7 | 64.1±4.8 | 12/9 | 13/5 | ||
| Bhayani[ | R | 美国 | NA | NA | LHM | POEM | 101 | 57 56 | 31/33 | 19/18 | |||
| Kumagai[ | PNC | 瑞典 | 22.9±3.6 | 23.3±3.7 | LHM | POEM | 83 | 45 | 45.5 | 19/22 | 27/15 | ||
| Chan[ | R | 中国 | NA | NA | LHM | POEM | 56 | 38.4 | 48.2 | 11/12 | 12/21 | ||
| Leeds[ | PNC | 美国 | 28.8±5.2 | 25.7±4.0 | LHM | POEM | 23 | 52.7±12.4 | 52.0±16.9 | 6/5 | 4/8 | ||
| Peng[ | R | 中国 | NA | NA | LHM | POEM | 31 | 44.7±21.6 | 37.5±13.0 | 8/10 | 8/5 | ||
| Werner[ | RCT | 美国 | 24.5±4.5 | 24.8±4.6 | LHM | POEM | 221 | 48.6±14.6 | 41.7±14.8 | 60/49 | 68/44 | ||
| Wirsching[ | PNC | 美国 | 27 | 30 | LHM | POEM | 51 | 56.6 | 58 | 12/16 | 11/12 | ||
| Ali[ | R | 巴西 | NA | NA | LHM | POEM | 40 | 44.2±13.2 | 44.9±14.6 | 14/6 | 12/8 | ||
| Costantini[ | PNC | 意大利 | 22 | 23 | LHM | POEM | 280 | 48 | 47 | 73/67 | 70/70 | ||
| Attaar[ | R | 美国 | 26.8±5.7 | 27.1±6.7 | LHM | POEM | 159 | 58.0±19.0 | 64.0±16.0 | 19/14 | 62/64 | ||
| Podboy[ | R | 美国 | NA | NA | LHM | POEM | 98 | 58.0±2.4 | 59.2±2.4 | 10/33 | 22/33 | ||
| Wong[ | PNC | 马来西亚 | NA | NA | LHM | POEM | 123 | 48.1±17.3 | 41.7±14.8 | 31/29 | 29/34 | ||
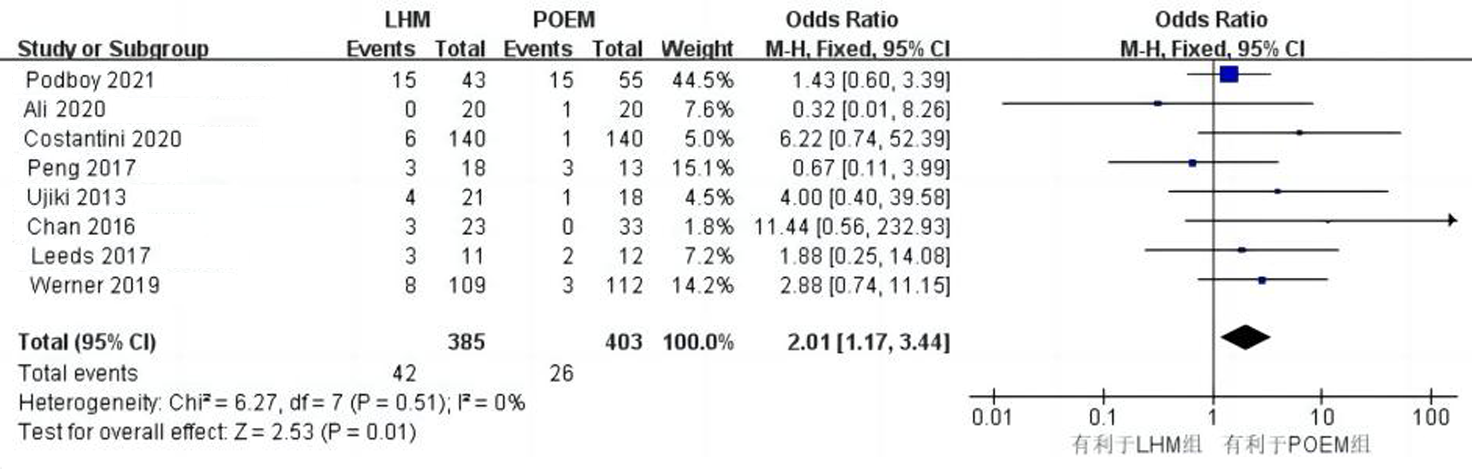
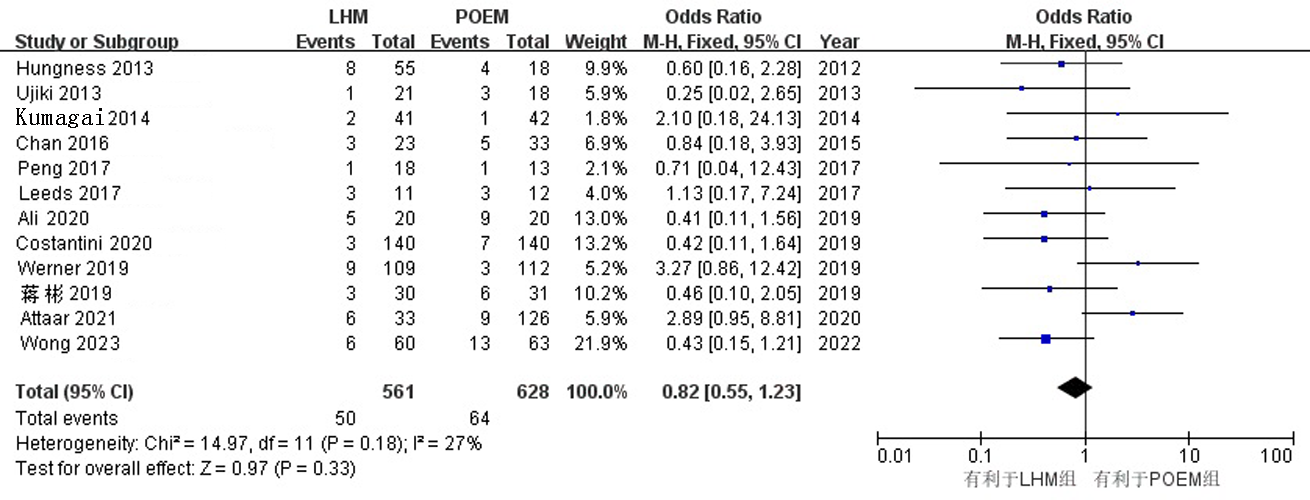
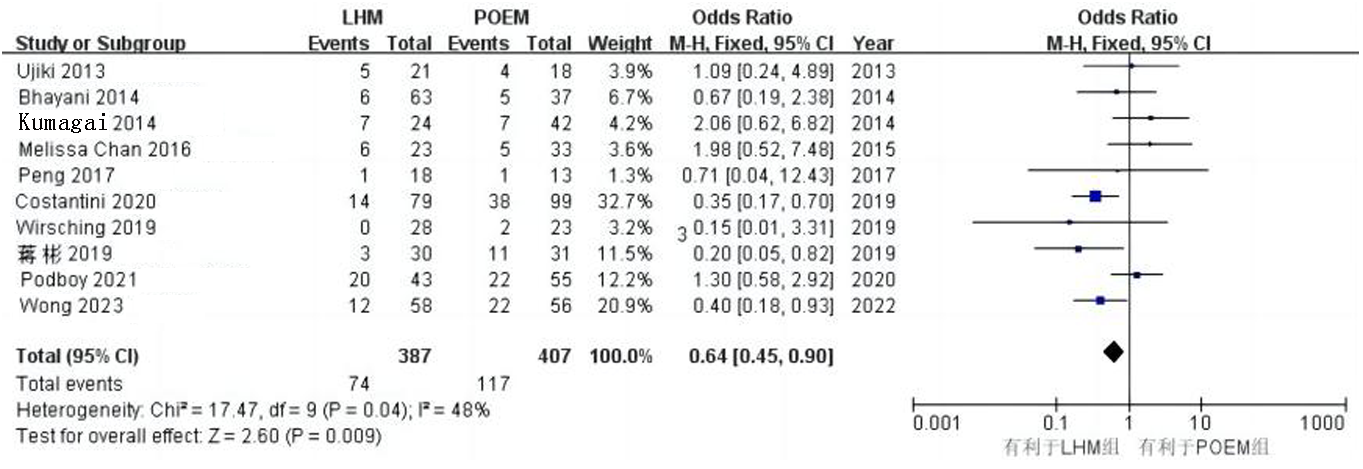
| 并发症 | 纳入研究数量 | 样本量(例) | 分析模型 | 95% | ||||
|---|---|---|---|---|---|---|---|---|
| LHM组 | POEM组 | |||||||
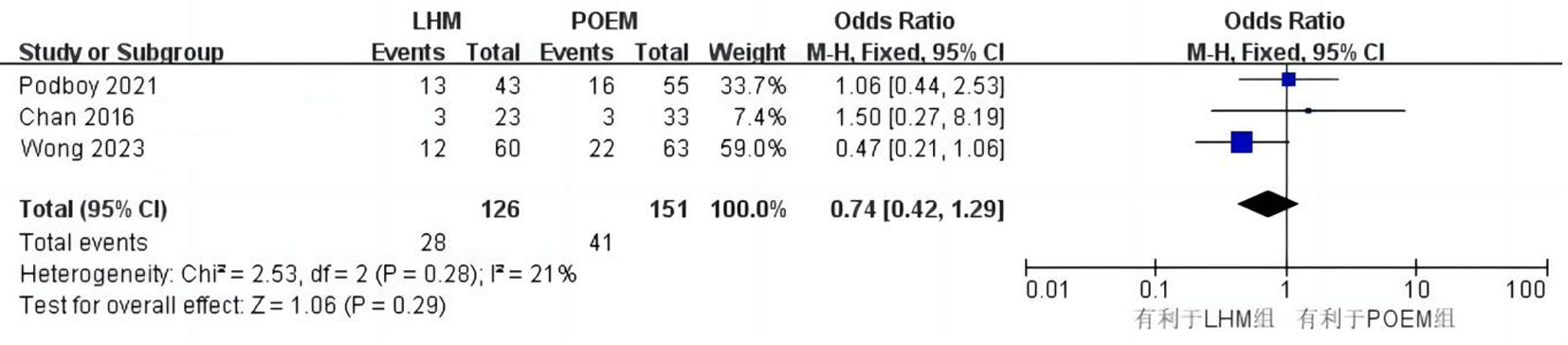
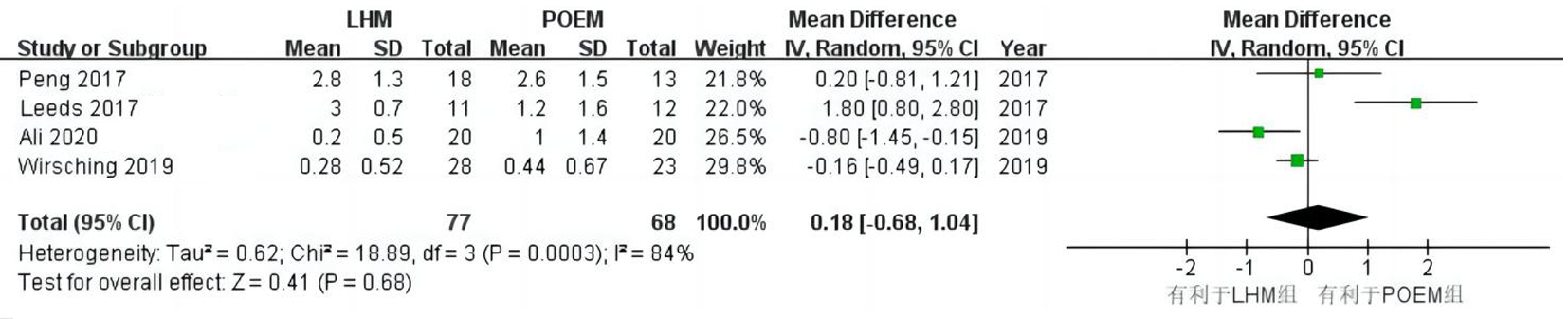
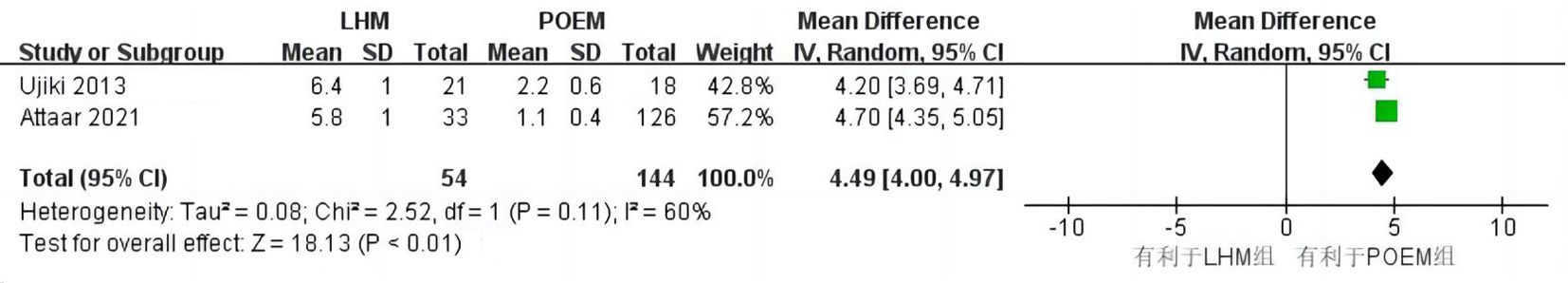
| 总体并发症 | 12[ | 561 | 628 | 27 | 0.82 | 固定效应模型 | (0.55, 1.23) | 0.33 |
| 胃食管反流病 | 10[ | 387 | 407 | 48 | 0.64 | 固定效应模型 | (0.45, 0.90) | <0.05 |
| 皮下气肿 | 5[ | 147 | 113 | 16 | 0.33 | 固定效应模型 | (0.11, 0.99) | 0.05 |
| 食管穿孔 | 7[ | 437 | 405 | 0 | 0.86 | 固定效应模型 | (0.39, 1.90) | 0.7 |
| 黏膜损伤 | 4[ | 129 | 129 | 67 | 0.86 | 随机效应模型 | (0.11, 6.61) | 0.89 |
Tab.2 Incidence of postoperative complications between the LHM group and the POEM group
| 并发症 | 纳入研究数量 | 样本量(例) | 分析模型 | 95% | ||||
|---|---|---|---|---|---|---|---|---|
| LHM组 | POEM组 | |||||||
| 总体并发症 | 12[ | 561 | 628 | 27 | 0.82 | 固定效应模型 | (0.55, 1.23) | 0.33 |
| 胃食管反流病 | 10[ | 387 | 407 | 48 | 0.64 | 固定效应模型 | (0.45, 0.90) | <0.05 |
| 皮下气肿 | 5[ | 147 | 113 | 16 | 0.33 | 固定效应模型 | (0.11, 0.99) | 0.05 |
| 食管穿孔 | 7[ | 437 | 405 | 0 | 0.86 | 固定效应模型 | (0.39, 1.90) | 0.7 |
| 黏膜损伤 | 4[ | 129 | 129 | 67 | 0.86 | 随机效应模型 | (0.11, 6.61) | 0.89 |
| [1] |
Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG Clinical Guidelines: Diagnosis and management of achalasia[J]. Am J Gastroenterol, 2020, 115(9): 1393-1411.
doi: 10.14309/ajg.0000000000000731 pmid: 32773454 |
| [2] | 刘瑛, 金世柱, 徐婉莹. 贲门失弛缓症发病机制的研究进展[J]. 中国比较医学杂志, 2020, 30(10): 138-142. |
| [3] | Schlottmann F, Herbella FAM, Patti MG. The evolution of the treatment of esophageal achalasia: From the open to the minimally invasive approach[J]. World J Surg, 2022, 46(7): 1522-1526. |
| [4] |
Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia[J]. Endoscopy, 2010, 42(4): 265-271.
doi: 10.1055/s-0029-1244080 pmid: 20354937 |
| [5] | Rolland S, Paterson W, Bechara R. Achalasia: Current therapeutic options[J]. Neurogastroenterol Motil, 2023, 35(1): e14459. |
| [6] | Pesce M, Sweis R. Advances and caveats in modern achalasia management[J]. Ther Adv Chronic Dis, 2021, 12: 2040622321993437. |
| [7] | 中华医学会消化内镜学分会超级微创协作组, 中国医师协会内镜医师分会, 北京医学会消化内镜学分会. 中国贲门失弛缓症诊治专家共识(2020, 北京)[J]. 中华消化内镜杂志, 2021, 38(4):256-275. |
| [8] | 蒋彬, 张灵敏, 孙天宇, 等. 腹腔镜Heller手术与经口内镜下肌切开术治疗贲门失弛缓症的临床效果比较[J]. 第三军医大学学报, 2019, 41(22):2199-2204. |
| [9] |
Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy[J]. J Gastrointest Surg, 2013, 17(2): 228-235.
doi: 10.1007/s11605-012-2030-3 pmid: 23054897 |
| [10] | Ujiki MB, Yetasook AK, Zapf M, et al. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach[J]. Surgery, 2013, 154(4): 893-897. |
| [11] |
Bhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia[J]. Ann Surg, 2014, 259(6): 1098-1103.
doi: 10.1097/SLA.0000000000000268 pmid: 24169175 |
| [12] |
Kumagai K, Tsai JA, Thorell A, et al. Per-oral endoscopic myotomy for achalasia. Are results comparable to laparoscopic Heller myotomy?[J]. Scandinavian journal of gastroenterology, 2015, 50(5): 505-512.
doi: 10.3109/00365521.2014.934915 pmid: 25712228 |
| [13] |
Chan SM, Wu JC, Teoh AY, et al. Comparison of early outcomes and quality of life after laparoscopic Heller's cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia[J]. Dig Endosc, 2016, 28(1): 27-32.
doi: 10.1111/den.12507 pmid: 26108140 |
| [14] |
Leeds SG, Burdick JS, Ogola GO, et al. Comparison of outcomes of laparoscopic Heller myotomy versus per-oral endoscopic myotomy for management of achalasia[J]. Proc (Bayl Univ Med Cent), 2017, 30(4): 419-423.
pmid: 28966450 |
| [15] |
Peng L, Tian S, Du C, et al. Outcome of peroral endoscopic myotomy (POEM) for treating achalasia compared with laparoscopic heller myotomy (LHM)[J]. Surg Laparosc Endosc Percutan Tech, 2017, 27(1): 60-64.
doi: 10.1097/SLE.0000000000000368 pmid: 28145968 |
| [16] | Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia[J]. N Engl J Med, 2019, 381(23): 2219-2229. |
| [17] |
Wirsching A, Boshier PR, Klevebro F, et al. Comparison of costs and short-term clinical outcomes of per-oral endoscopic myotomy and laparoscopic Heller myotomy[J]. Am J Surg, 2019, 218(4): 706-711.
doi: S0002-9610(19)30160-6 pmid: 31353034 |
| [18] |
Ali AB, Khan NA, Nguyen DT, et al. Robotic and per-oral endoscopic myotomy have fewer technical complications compared to laparoscopic Heller myotomy[J]. Surg Endosc, 2020, 34(7): 3191-3196.
doi: 10.1007/s00464-019-07093-2 pmid: 31482358 |
| [19] |
Costantini A, Familiari P, Costantini M, et al. Poem versus laparoscopic heller myotomy in the treatment of esophageal achalasia: A case-control study from two high volume centers using the propensity score[J]. J Gastrointest Surg, 2020, 24(3): 505-515.
doi: 10.1007/s11605-019-04465-w pmid: 31848870 |
| [20] |
Attaar M, Su B, Wong HJ, et al. Comparing cost and outcomes between peroral endoscopic myotomy and laparoscopic heller myotomy[J]. Am J Surg, 2021, 222(1): 208-213.
doi: 10.1016/j.amjsurg.2020.10.037 pmid: 33162014 |
| [21] | Podboy AJ, Hwang JH, Rivas H, et al. Long-term outcomes of per-oral endoscopic myotomy compared to laparoscopic Heller myotomy for achalasia: A single-center experience[J]. Surg Endosc, 2021, 35(2): 792-801. |
| [22] | Wong WJ, Affendi N, Siow SL, et al. When is POEM truly equivalent to LHM? A comparison of complication rates during the learning curve[J]. Surg Endosc, 2023, 37(3): 1735-1741. |
| [23] | 李泽宇, 黄留业. 高分辨率食管测压在经口内镜下肌切开术治疗贲门失弛缓症中的应用价值[J]. 中国内镜杂志, 2021, 27(2): 55-60. |
| [24] |
Swanström LL. Achalasia: Treatment, current status and future advances[J]. Korean J Intern Med, 2019, 34(6): 1173-1180.
doi: 10.3904/kjim.2018.439 pmid: 30866609 |
| [25] |
Olson MT, Triantafyllou T, Singhal S. A Decade of investigation: peroral endoscopic myotomy versus laparoscopic heller myotomy for achalasia[J]. J Laparoendosc Adv Surg Tech A, 2019, 29(9): 1093-1104.
doi: 10.1089/lap.2019.0242 pmid: 31313957 |
| [26] |
Haisley KR, Swanström LL. The modern age of POEM: The past, present and future of per-oral endoscopic myotomy[J]. J Gastrointest Surg, 2021, 25(2): 551-557.
doi: 10.1007/s11605-020-04815-z pmid: 33140317 |
| [27] | 马晓冰, 王瑞玲, 李雪, 等. 经口内镜下肌切开术治疗贲门失弛缓症的研究进展[J]. 中华胃肠内镜电子杂志, 2015, 2(3): 108-112. |
| [28] |
Costantini M, Salvador R, Costantini A. Esophageal achalasia: Pros and cons of the treatment options[J]. World J Surg, 2022, 46(7): 1554-1560.
doi: 10.1007/s00268-022-06495-z pmid: 35238987 |
| [29] |
Schlottmann F, Luckett DJ, Fine J, et al. Laparoscopic heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: A systematic review and meta-analysis[J]. Ann Surg, 2018, 267(3): 451-460.
doi: 10.1097/SLA.0000000000002311 pmid: 28549006 |
| [30] |
Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia[J]. Gastrointest Endosc, 2020, 91(2): 213-227.e6.
doi: S0016-5107(19)31658-X pmid: 31839408 |
| [31] |
Talukdar R, Inoue H, Nageshwar Reddy D. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: A systematic review and meta-analysis[J]. Surg Endosc, 2015, 29(11): 3030-3046.
doi: 10.1007/s00464-014-4040-6 pmid: 25539695 |
| [32] | Gong F, Li Y, Ye S. Effectiveness and complication of achalasia treatment: A systematic review and network meta-analysis of randomized controlled trials[J]. Asian J Surg, 2023, 46(1): 24-34. |
| [33] |
Du C, Ma L, Chai N, et al. Factors affecting the effectiveness and safety of submucosal tunneling endoscopic resection for esophageal submucosal tumors originating from the muscularis propria layer[J]. Surg Endosc, 2018, 32(3): 1255-1264.
doi: 10.1007/s00464-017-5800-x pmid: 28842802 |
| [34] | Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: A series of 500 patients[J]. J Am Coll Surg, 2015, 221(2): 256-264. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||